Society Needs Regulations to Prevent Research Abuses

A tension exists between scientists/doctors and government regulators.
[Editor's Note: Our Big Moral Question this month is, "Do government regulations help or hurt the goal of responsible and timely scientific innovation?"]
Government regulations help more than hurt the goal of responsible and timely scientific innovation. Opponents might argue that without regulations, researchers would be free to do whatever they want. But without ethics and regulations, scientists have performed horrific experiments. In Nazi concentration camps, for instance, doctors forced prisoners to stay in the snow to see how long it took for these inmates to freeze to death. These researchers also removed prisoner's limbs in order to try to develop innovations to reconnect these body parts, but all the experiments failed.
Researchers in not only industry, but also academia have violated research participants' rights.
Due to these atrocities, after the war, the Nuremberg Tribunal established the first ethical guidelines for research, mandating that all study participants provide informed consent. Yet many researchers, including those in leading U.S. academic institutions and government agencies, failed to follow these dictates. The U.S. government, for instance, secretly infected Guatemalan men with syphilis in order to study the disease and experimented on soldiers, exposing them without consent to biological and chemical warfare agents. In the 1960s, researchers at New York's Willowbrook State School purposefully fed intellectually disabled children infected stool extracts with hepatitis to study the disease. In 1966, in the New England Journal of Medicine, Henry Beecher, a Harvard anesthesiologist, described 22 cases of unethical research published in the nation's leading medical journals, but were mostly conducted without informed consent, and at times harmed participants without offering them any benefit.
Despite heightened awareness and enhanced guidelines, abuses continued. Until a 1974 journalistic exposé, the U.S. government continued to fund the now-notorious Tuskegee syphilis study of infected poor African-American men in rural Alabama, refusing to offer these men penicillin when it became available as effective treatment for the disease.
In response, in 1974 Congress passed the National Research Act, establishing research ethics committees or Institutional Review Boards (IRBs), to guide scientists, allowing them to innovate while protecting study participants' rights. Routinely, IRBs now detect and prevent unethical studies from starting.
Still, even with these regulations, researchers have at times conducted unethical investigations. In 1999 at the Los Angeles Veterans Affairs Hospital, for example, a patient twice refused to participate in a study that would prolong his surgery. The researcher nonetheless proceeded to experiment on him anyway, using an electrical probe in the patient's heart to collect data.
Part of the problem and consequent need for regulations is that researchers have conflicts of interest and often do not recognize ethical challenges their research may pose.
Pharmaceutical company scandals, involving Avandia, and Neurontin and other drugs, raise added concerns. In marketing Vioxx, OxyContin, and tobacco, corporations have hidden findings that might undercut sales.
Regulations become increasingly critical as drug companies and the NIH conduct increasing amounts of research in the developing world. In 1996, Pfizer conducted a study of bacterial meningitis in Nigeria in which 11 children died. The families thus sued. Pfizer produced a Nigerian IRB approval letter, but the letter turned out to have been forged. No Nigerian IRB had ever approved the study. Fourteen years later, Wikileaks revealed that Pfizer had hired detectives to find evidence of corruption against the Nigerian Attorney General, to compel him to drop the lawsuit.
Researchers in not only industry, but also academia have violated research participants' rights. Arizona State University scientists wanted to investigate the genes of a Native American group, the Havasupai, who were concerned about their high rates of diabetes. The investigators also wanted to study the group's rates of schizophrenia, but feared that the tribe would oppose the study, given the stigma. Hence, these researchers decided to mislead the tribe, stating that the study was only about diabetes. The university's research ethics committee knew the scientists' plan to study schizophrenia, but approved the study, including the consent form, which did not mention any psychiatric diagnoses. The Havasupai gave blood samples, but later learned that the researchers published articles about the tribe's schizophrenia and alcoholism, and genetic origins in Asia (while the Havasupai believed they originated in the Grand Canyon, where they now lived, and which they thus argued they owned). A 2010 legal settlement required that the university return the blood samples to the tribe, which then destroyed them. Had the researchers instead worked with the tribe more respectfully, they could have advanced science in many ways.
Part of the problem and consequent need for regulations is that researchers have conflicts of interest and often do not recognize ethical challenges their research may pose.
Such violations threaten to lower public trust in science, particularly among vulnerable groups that have historically been systemically mistreated, diminishing public and government support for research and for the National Institutes of Health, National Science Foundation and Centers for Disease Control, all of which conduct large numbers of studies.
Research that has failed to follow ethics has in fact impeded innovation.
In popular culture, myths of immoral science and technology--from Frankenstein to Big Brother and Dr. Strangelove--loom.
Admittedly, regulations involve inherent tradeoffs. Following certain rules can take time and effort. Certain regulations may in fact limit research that might potentially advance knowledge, but be grossly unethical. For instance, if our society's sole goal was to have scientists innovate as much as possible, we might let them stick needles into healthy people's brains to remove cells in return for cash that many vulnerable poor people might find desirable. But these studies would clearly pose major ethical problems.
Research that has failed to follow ethics has in fact impeded innovation. In 1999, the death of a young man, Jesse Gelsinger, in a gene therapy experiment in which the investigator was subsequently found to have major conflicts of interest, delayed innovations in the field of gene therapy research for years.
Without regulations, companies might market products that prove dangerous, leading to massive lawsuits that could also ultimately stifle further innovation within an industry.
The key question is not whether regulations help or hurt science alone, but whether they help or hurt science that is both "responsible and innovative."
We don't want "over-regulation." Rather, the right amount of regulations is needed – neither too much nor too little. Hence, policy makers in this area have developed regulations in fair and transparent ways and have also been working to reduce the burden on researchers – for instance, by allowing single IRBs to review multi-site studies, rather than having multiple IRBs do so, which can create obstacles.
In sum, society requires a proper balance of regulations to ensure ethical research, avoid abuses, and ultimately aid us all by promoting responsible innovation.
[Ed. Note: Check out the opposite viewpoint here, and follow LeapsMag on social media to share your perspective.]
Recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen as soon as 18 months from now
Like all those whose kidneys have failed, Scott Burton’s life revolves around dialysis. For nearly two decades, Burton has been hooked up (or, since 2020, has hooked himself up at home) to a dialysis machine that performs the job his kidneys normally would. The process is arduous, time-consuming, and expensive. Except for a brief window before his body rejected a kidney transplant, Burton has depended on machines to take the place of his kidneys since he was 12-years-old. His whole life, the 39-year-old says, revolves around dialysis.
“Whenever I try to plan anything, I also have to plan my dialysis,” says Burton says, who works as a freelance videographer and editor. “It’s a full-time job in itself.”
Many of those on dialysis are in line for a kidney transplant that would allow them to trade thrice-weekly dialysis and strict dietary limits for a lifetime of immunosuppressants. Burton’s previous transplant means that his body will likely reject another donated kidney unless it matches perfectly—something he’s not counting on. It’s why he’s enthusiastic about the development of artificial kidneys, small wearable or implantable devices that would do the job of a healthy kidney while giving users like Burton more flexibility for traveling, working, and more.
Still, the devices aren’t ready for testing in humans—yet. But recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen as soon as 18 months from now, according to Jonathan Himmelfarb, a nephrologist at the University of Washington.
“It would liberate people with kidney failure,” Himmelfarb says.
An engineering marvel
Compared to the heart or the brain, the kidney doesn’t get as much respect from the medical profession, but its job is far more complex. “It does hundreds of different things,” says UCLA’s Ira Kurtz.
Kurtz would know. He’s worked as a nephrologist for 37 years, devoting his career to helping those with kidney disease. While his colleagues in cardiology and endocrinology have seen major advances in the development of artificial hearts and insulin pumps, little has changed for patients on hemodialysis. The machines remain bulky and require large volumes of a liquid called dialysate to remove toxins from a patient’s blood, along with gallons of purified water. A kidney transplant is the next best thing to someone’s own, functioning organ, but with over 600,000 Americans on dialysis and only about 100,000 kidney transplants each year, most of those in kidney failure are stuck on dialysis.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. Each of the 45 different cell types in the kidney do something different.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. To build an artificial heart, Kurtz says, you basically need to engineer a pump. An artificial pancreas needs to balance blood sugar levels with insulin secretion. While neither of these tasks is simple, they are fairly straightforward. The kidney, on the other hand, does more than get rid of waste products like urea and other toxins. Each of the 45 different cell types in the kidney do something different, helping to regulate electrolytes like sodium, potassium, and phosphorous; maintaining blood pressure and water balance; guiding the body’s hormonal and inflammatory responses; and aiding in the formation of red blood cells.
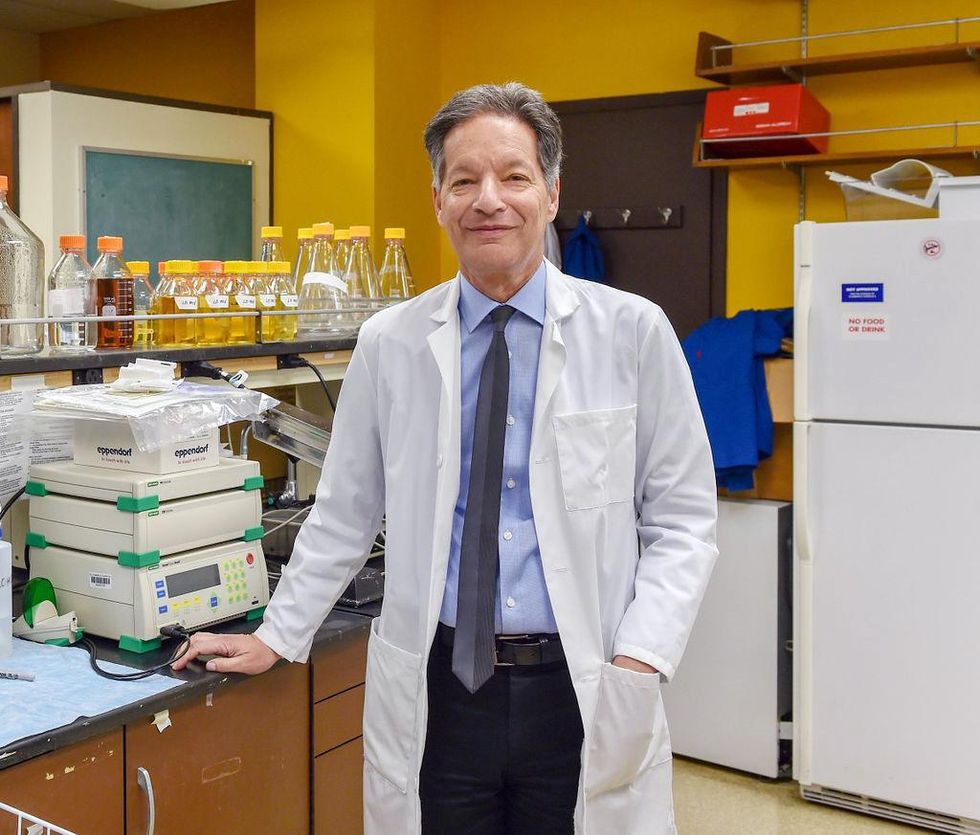
There's been little progress for patients during Ira Kurtz's 37 years as a nephrologist. Artificial kidneys would change that.
UCLA
Dialysis primarily filters waste, and does so well enough to keep someone alive, but it isn’t a true artificial kidney because it doesn’t perform the kidney’s other jobs, according to Kurtz, such as sensing levels of toxins, wastes, and electrolytes in the blood. Due to the size and water requirements of existing dialysis machines, the equipment isn’t portable. Physicians write a prescription for a certain duration of dialysis and assess how well it’s working with semi-regular blood tests. The process of dialysis itself, however, is conducted blind. Doctors can’t tell how much dialysis a patient needs based on kidney values at the time of treatment, says Meera Harhay, a nephrologist at Drexel University in Philadelphia.
But it’s the impact of dialysis on their day-to-day lives that creates the most problems for patients. Only one-quarter of those on dialysis are able to remain employed (compared to 85% of similar-aged adults), and many report a low quality of life. Having more flexibility in life would make a major different to her patients, Harhay says.
“Almost half their week is taken up by the burden of their treatment. It really eats away at their freedom and their ability to do things that add value to their life,” she says.
Art imitates life
The challenge for artificial kidney designers was how to compress the kidney’s natural functions into a portable, wearable, or implantable device that wouldn’t need constant access to gallons of purified and sterilized water. The other universal challenge they faced was ensuring that any part of the artificial kidney that would come in contact with blood was kept germ-free to prevent infection.
As part of last year’s KidneyX Prize, a partnership between the U.S. Department of Health and Human Services and the American Society of Nephrology, inventors were challenged to create prototypes for artificial kidneys. Himmelfarb’s team at the University of Washington’s Center for Dialysis Innovation won the prize by focusing on miniaturizing existing technologies to create a portable dialysis machine. The backpack sized AKTIV device (Ambulatory Kidney to Increase Vitality) will recycle dialysate in a closed loop system that removes urea from blood and uses light-based chemical reactions to convert the urea to nitrogen and carbon dioxide, which allows the dialysate to be recirculated.
Himmelfarb says that the AKTIV can be used when at home, work, or traveling, which will give users more flexibility and freedom. “If you had a 30-pound device that you could put in the overhead bins when traveling, you could go visit your grandkids,” he says.
Kurtz’s team at UCLA partnered with the U.S. Kidney Research Corporation and Arkansas University to develop a dialysate-free desktop device (about the size of a small printer) as the first phase of a progression that will he hopes will lead to something small and implantable. Part of the reason for the artificial kidney’s size, Kurtz says, is the number of functions his team are cramming into it. Not only will it filter urea from blood, but it will also use electricity to help regulate electrolyte levels in a process called electrodeionization. Kurtz emphasizes that these additional functions are what makes his design a true artificial kidney instead of just a small dialysis machine.
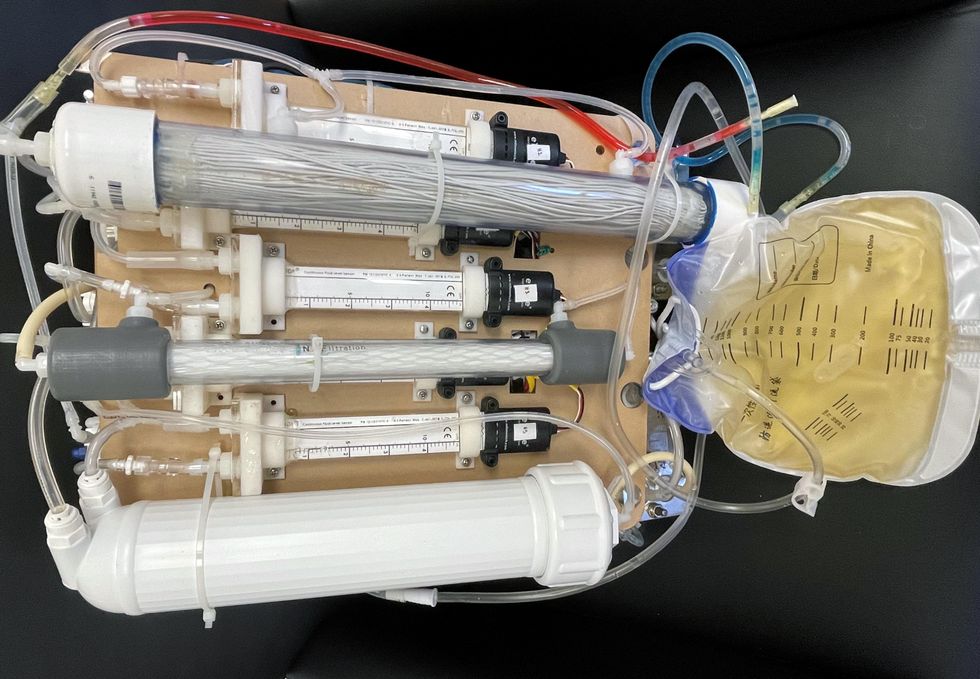
One version of an artificial kidney.
UCLA
“It doesn't have just a static function. It has a bank of sensors that measure chemicals in the blood and feeds that information back to the device,” Kurtz says.
Other startups are getting in on the game. Nephria Bio, a spinout from the South Korean-based EOFlow, is working to develop a wearable dialysis device, akin to an insulin pump, that uses miniature cartridges with nanomaterial filters to clean blood (Harhay is a scientific advisor to Nephria). Ian Welsford, Nephria’s co-founder and CTO, says that the device’s design means that it can also be used to treat acute kidney injuries in resource-limited settings. These potentials have garnered interest and investment in artificial kidneys from the U.S. Department of Defense.
For his part, Burton is most interested in an implantable device, as that would give him the most freedom. Even having a regular outpatient procedure to change batteries or filters would be a minor inconvenience to him.
“Being plugged into a machine, that’s not mimicking life,” he says.
Today’s more than 20,000 mental health apps have a wide range of functionalities and business models. Many of them can be useful for depression.
Even before the pandemic created a need for more telehealth options, depression was a hot area of research for app developers. Given the high prevalence of depression and its connection to suicidality — especially among today’s teenagers and young adults who grew up with mobile devices, use them often, and experience these conditions with alarming frequency — apps for depression could be not only useful but lifesaving.
“For people who are not depressed, but have been depressed in the past, the apps can be helpful for maintaining positive thinking and behaviors,” said Andrea K. Wittenborn, PhD, director of the Couple and Family Therapy Doctoral Program and a professor in human development and family studies at Michigan State University. “For people who are mildly to severely depressed, apps can be a useful complement to working with a mental health professional.”
Health and fitness apps, in general, number in the hundreds of thousands. These are driving a market expected to reach $102.45 billion by next year. The mobile mental health app market is a small part of this but still sizable at $500 million, with revenues generated through user health insurance, employers, and direct payments from individuals.
Apps can provide data that health professionals cannot gather on their own. People’s constant interaction with smartphones and wearable devices yields data on many health conditions for millions of patients in their natural environments and while they go about their usual activities. Compared with the in-office measurements of weight and blood pressure and the brevity of doctor-patient interactions, the thousands of data points gathered unobtrusively over an extended time period provide a far better and more detailed picture of the person and their health.
At their most advanced level, apps for mental health, including depression, passively gather data on how the user touches and interacts with the mobile device through changes in digital biomarkers that relate to depressive symptoms and other conditions.
Building on three decades of research since early “apps” were used for delivering treatment manuals to health professionals, today’s more than 20,000 mental health apps have a wide range of functionalities and business models. Many of these apps can be useful for depression.
Some apps primarily provide a virtual connection to a group of mental health professionals employed or contracted by the app. Others have options for meditation, sleeping or, in the case of industry leaders Calm and Headspace, overall well-being. On the cutting edge are apps that detect changes in a person’s use of mobile devices and their interactions with them.
Apps such as AbleTo, Happify Health, and Woebot Health focus on cognitive behavioral therapy, a type of counseling with proven potential to change a person’s behaviors and feelings. “CBT has been demonstrated in innumerable studies over the last several decades to be effective in the treatment of behavioral health conditions such as depression and anxiety disorders,” said Dr. Reena Pande, chief medical officer at AbleTo. “CBT is intended to be delivered as a structured intervention incorporating key elements, including behavioral activation and adaptive thinking strategies.”
These CBT skills help break the negative self-talk (rumination) common in patients with depression. They are taught and reinforced by some self-guided apps, using either artificial intelligence or programmed interactions with users. Apps can address loneliness and isolation through connections with others, even when a symptomatic person doesn’t feel like leaving the house.
At their most advanced level, apps for mental health, including depression, passively gather data on how the user touches and interacts with the mobile device through changes in “digital biomarkers” that can be associated with onset or worsening of depressive symptoms and other cognitive conditions. In one study, Mindstrong Health gathered a year’s worth of data on how people use their smartphones, such as scrolling through articles, typing and clicking. Mindstrong, whose founders include former leaders of the National Institutes of Health, modeled the timing and order of these actions to make assessments that correlated closely with gold-standard tests of cognitive function.
National organizations of mental health professionals have been following the expanding number of available apps over the years with keen interest. App Advisor is an initiative of the American Psychiatric Association that helps psychiatrists and other mental health professionals navigate the issues raised by mobile health technology. App Advisor does not rate or recommend particular apps but rather provides guidance about why apps should be assessed and how health professionals can do this.
A website that does review mental health apps is One Mind Psyber Guide, an independent nonprofit that partners with several national organizations. One Mind users can select among numerous search terms for the condition and therapeutic approach of interest. Apps are rated on a five-point scale, with reviews written by professionals in the field.
Do mental health apps related to depression have the kind of safety and effectiveness data required for medications and other medical interventions? Not always — and not often. Yet the overall results have shown early promise, Wittenborn noted.
“Studies that have attempted to detect depression from smartphone and wearable sensors [during a single session] have ranged in accuracy from about 86 to 89 percent,” Wittenborn said. “Studies that tried to predict changes in depression over time have been less accurate, with accuracy ranging from 59 to 85 percent.”
The Food and Drug Administration encourages the development of apps and has approved a few of them—mostly ones used by health professionals—but it is generally “hands off,” according to the American Psychiatric Association. The FDA has published a list of examples of software (including programming of apps) that it does not plan to regulate because they pose low risk to the public. First on the list is software that helps patients with diagnosed psychiatric conditions, including depression, maintain their behavioral coping skills by providing a “Skill of the Day” technique or message.
On its App Advisor site, the American Psychiatric Association says mental health apps can be dangerous or cause harm in multiple ways, such as by providing false information, overstating the app’s therapeutic value, selling personal data without clearly notifying users, and collecting data that isn’t relevant to mental health.
Although there is currently reason for caution, patients may eventually come to expect mental health professionals to recommend apps, especially as their rating systems, features and capabilities expand. Through such apps, patients might experience more and higher quality interactions with their mental health professionals. “Apps will continue to be refined and become more effective through future research,” said Wittenborn. “They will become more integrated into practice over time.”