New therapy may improve stem cell transplants for blood cancers

Ivan Dimov, Jeroen Bekaert and Nate Fernhoff - pictured here - recognized the need for a more effective cell sorting technology to reduce the risk of Graft vs Host disease, which affects many cancer patients after receiving stem cell transplants.
In 2018, Robyn was diagnosed with myelofibrosis, a blood cancer causing chronic inflammation and scarring. As a research scientist by training, she knew she had limited options. A stem cell transplant is a terminally ill patient's best chance for survival against blood cancers, including leukaemia. It works by destroying a patient's cancer cells and replacing them with healthy cells from a donor.
However, there is a huge risk of Graft vs Host disease (GVHD), which affects around 30-40% of recipients. Patients receive billions of cells in a stem cell transplant but only a fraction are beneficial. The rest can attack healthy tissue leading to GVHD. It affects the skin, gut and lungs and can be truly debilitating.
Currently, steroids are used to try and prevent GVHD, but they have many side effects and are effective in only 50% of cases. “I spoke with my doctors and reached out to patients managing GVHD,” says Robyn, who prefers not to use her last name for privacy reasons. “My concerns really escalated for what I might face post-transplant.”
Then she heard about a new highly precise cell therapy developed by a company called Orca Bio, which gives patients more beneficial cells and fewer cells that cause GVHD. She decided to take part in their phase 2 trial.
How It Works
In stem cell transplants, patients receive immune cells and stem cells. The donor immune cells or T cells attack and kill malignant cells. This is the graft vs leukaemia effect (GVL). The stem cells generate new healthy cells.
Unfortunately, T cells can also cause GVHD, but a rare subset of T cells, called T regulatory cells, can actually prevent GVHD.
Orca’s cell sorting technology distinguishes T regulatory cells from stem cells and conventional T cells on a large scale. It’s this cell sorting technology which has enabled them to create their new cell therapy, called Orca T. It contains a precise combination of stem cells and immune cells with more T regulatory cells and fewer conventional T cells than in a typical stem cell transplant.
“Ivan Dimov’s idea was to spread out the cells, keep them stationary and then use laser scanning to sort the cells,” explains Nate Fernhoff, co-founder of Orca Bio. “The beauty here is that lasers don't care how quickly you move them.”
Over the past 40 years, scientists have been trying to create stem cell grafts that contain the beneficial cells whilst removing the cells that cause GVHD. What makes it even harder is that most transplant centers aren’t able to manipulate grafts to create a precise combination of cells.
Innovative Cell Sorting
Ivan Dimov, Jeroen Bekaert and Nate Fernhoff came up with the idea behind Orca as postdocs at Stanford, working with cell pioneer Irving Weissman. They recognised the need for a more effective cell sorting technology. In a small study at Stanford, Professor Robert Negrin had discovered a combination of T cells, T regulatory cells and stem cells which prevented GVHD but retained the beneficial graft vs leukaemia effect (GVL). However, manufacturing was problematic. Conventional cell sorting is extremely slow and specific. Negrin was only able to make seven highly precise products, for seven patients, in a year. Annual worldwide cases of blood cancer number over 1.2 million.
“We started Orca with this idea: how do we use manufacturing solutions to impact cell therapies,” co-founder Fernhoff reveals. In conventional cell sorting, cells move past a stationary laser which analyses each cell. But cells can only be moved so quickly. At a certain point they start to experience stress and break down. This makes it very difficult to sort the 100 billion cells from a donor in a stem cell transplant.
“Ivan Dimov’s idea was to spread out the cells, keep them stationary and then use laser scanning to sort the cells,” Fernhoff explains. “The beauty here is that lasers don't care how quickly you move them.” They developed this technology and called it Orca Sort. It enabled Orca to make up to six products per week in the first year of manufacturing.
Every product Orca makes is for one patient. The donor is uniquely matched to the patient. They have to carry out the cell sorting procedure each time. Everything also has to be done extremely quickly. They infuse fresh living cells from the donor's vein to the patient's within 72 hours.
“We’ve treated almost 200 patients in all the Orca trials, and you can't do that if you don't fix the manufacturing process,” Fernhoff says. “We're working on what we think is an incredibly promising drug, but it's all been enabled by figuring out how to make a high precision cell therapy at scale.”
Clinical Trials
Orca revealed the results of their phase 1b and phase 2 trials at the end of last year. In their phase 2 trial only 3% of the 29 patients treated with Orca T cell therapy developed chronic GVHD in the first year after treatment. Comparatively, 43% of the 95 patients given a conventional stem cell transplant in a contemporary Stanford trial developed chronic GVHD. Of the 109 patients tested in phase 1b and phase 2 trials, 74% using Orca T didn't relapse or develop any form of GVHD compared to 34% in the control trial.
“Until a randomised study is done, we can make no assumption about the relative efficacy of this approach," says Jeff Szer, professor of haematology at the Royal Melbourne Hospital. "But the holy grail of separating GVHD and GVL is still there and this is a step towards realising that dream.”
Stan Riddell, an immunology professor, at Fred Hutchinson Cancer Centre, believes Orca T is highly promising. “Orca has advanced cell selection processes with innovative methodology and can engineer grafts with greater precision to add cell subsets that may further contribute to beneficial outcomes,” he says. “Their results in phase 1 and phase 2 studies are very exciting and offer the potential of providing a new standard of care for stem cell transplant.”
However, though it is an “intriguing step,” there’s a need for further testing, according to Jeff Szer, a professor of haematology at the Peter MacCallum Cancer Centre at the Royal Melbourne Hospital.
“The numbers tested were tiny and comparing the outcomes to anything from a phase 1/2 setting is risky,” says Szer. “Until a randomised study is done, we can make no assumption about the relative efficacy of this approach. But the holy grail of separating GVHD and GVL is still there and this is a step towards realising that dream.”
The Future
The team is soon starting Phase 3 trials for Orca T. Its previous success has led them to develop Orca Q, a cell therapy for patients who can't find an exact donor match. Transplants for patients who are only a half-match or mismatched are not widely used because there is a greater risk of GVHD. Orca Q has the potential to control GVHD even more and improve access to transplants for many patients.
Fernhoff hopes they’ll be able to help people not just with blood cancers but also with other blood and immune disorders. If a patient has a debilitating disease which isn't life threatening, the risk of GVHD outweighs the potential benefits of a stem cell transplant. The Orca products could take away that risk.
Meanwhile, Robyn has no regrets about participating in the Phase 2 trial. “It was a serious decision to make but I'm forever grateful that I did,” she says. “I have resumed a quality of life aligned with how I felt pre-transplant. I have not had a single issue with GVHD.”
“I want to be able to get one of these products to every patient who could benefit from it,” Fernhoff says. “It's really exciting to think about how Orca's products could be applied to all sorts of autoimmune disorders.”
Peanut allergies affect about a million children in the U.S., and most never outgrow them. Luckily, some promising remedies are in the works.
Ever since he was a baby, Sharon Wong’s son Brandon suffered from rashes, prolonged respiratory issues and vomiting. In 2006, as a young child, he was diagnosed with a severe peanut allergy.
"My son had a history of reacting to traces of peanuts in the air or in food,” says Wong, a food allergy advocate who runs a blog focusing on nut free recipes, cooking techniques and food allergy awareness. “Any participation in school activities, social events, or travel with his peanut allergy required a lot of preparation.”
Peanut allergies affect around a million children in the U.S. Most never outgrow the condition. The problem occurs when the immune system mistakenly views the proteins in peanuts as a threat and releases chemicals to counteract it. This can lead to digestive problems, hives and shortness of breath. For some, like Wong’s son, even exposure to trace amounts of peanuts could be life threatening. They go into anaphylactic shock and need to take a shot of adrenaline as soon as possible.
Typically, people with peanut allergies try to completely avoid them and carry an adrenaline autoinjector like an EpiPen in case of emergencies. This constant vigilance is very stressful, particularly for parents with young children.
“The search for a peanut allergy ‘cure’ has been a vigorous one,” says Claudia Gray, a pediatrician and allergist at Vincent Pallotti Hospital in Cape Town, South Africa. The closest thing to a solution so far, she says, is the process of desensitization, which exposes the patient to gradually increasing doses of peanut allergen to build up a tolerance. The most common type of desensitization is oral immunotherapy, where patients ingest small quantities of peanut powder. It has been effective but there is a risk of anaphylaxis since it involves swallowing the allergen.
"By the end of the trial, my son tolerated approximately 1.5 peanuts," Sharon Wong says.
DBV Technologies, a company based in Montrouge, France has created a skin patch to address this problem. The Viaskin Patch contains a much lower amount of peanut allergen than oral immunotherapy and delivers it through the skin to slowly increase tolerance. This decreases the risk of anaphylaxis.
Wong heard about the peanut patch and wanted her son to take part in an early phase 2 trial for 4-to-11-year-olds.
“We felt that participating in DBV’s peanut patch trial would give him the best chance at desensitization or at least increase his tolerance from a speck of peanut to a peanut,” Wong says. “The daily routine was quite simple, remove the old patch and then apply a new one. By the end of the trial, he tolerated approximately 1.5 peanuts.”
How it works
For DBV Technologies, it all began when pediatric gastroenterologist Pierre-Henri Benhamou teamed up with fellow professor of gastroenterology Christopher Dupont and his brother, engineer Bertrand Dupont. Together they created a more effective skin patch to detect when babies have allergies to cow's milk. Then they realized that the patch could actually be used to treat allergies by promoting tolerance. They decided to focus on peanut allergies first as the more dangerous.
The Viaskin patch utilizes the fact that the skin can promote tolerance to external stimuli. The skin is the body’s first defense. Controlling the extent of the immune response is crucial for the skin. So it has defense mechanisms against external stimuli and can promote tolerance.
The patch consists of an adhesive foam ring with a plastic film on top. A small amount of peanut protein is placed in the center. The adhesive ring is attached to the back of the patient's body. The peanut protein sits above the skin but does not directly touch it. As the patient sweats, water droplets on the inside of the film dissolve the peanut protein, which is then absorbed into the skin.
The peanut protein is then captured by skin cells called Langerhans cells. They play an important role in getting the immune system to tolerate certain external stimuli. Langerhans cells take the peanut protein to lymph nodes which activate T regulatory cells. T regulatory cells suppress the allergic response.
A different patch is applied to the skin every day to increase tolerance. It’s both easy to use and convenient.
“The DBV approach uses much smaller amounts than oral immunotherapy and works through the skin significantly reducing the risk of allergic reactions,” says Edwin H. Kim, the division chief of Pediatric Allergy and Immunology at the University of North Carolina, U.S., and one of the principal investigators of Viaskin’s clinical trials. “By not going through the mouth, the patch also avoids the taste and texture issues. Finally, the ability to apply a patch and immediately go about your day may be very attractive to very busy patients and families.”
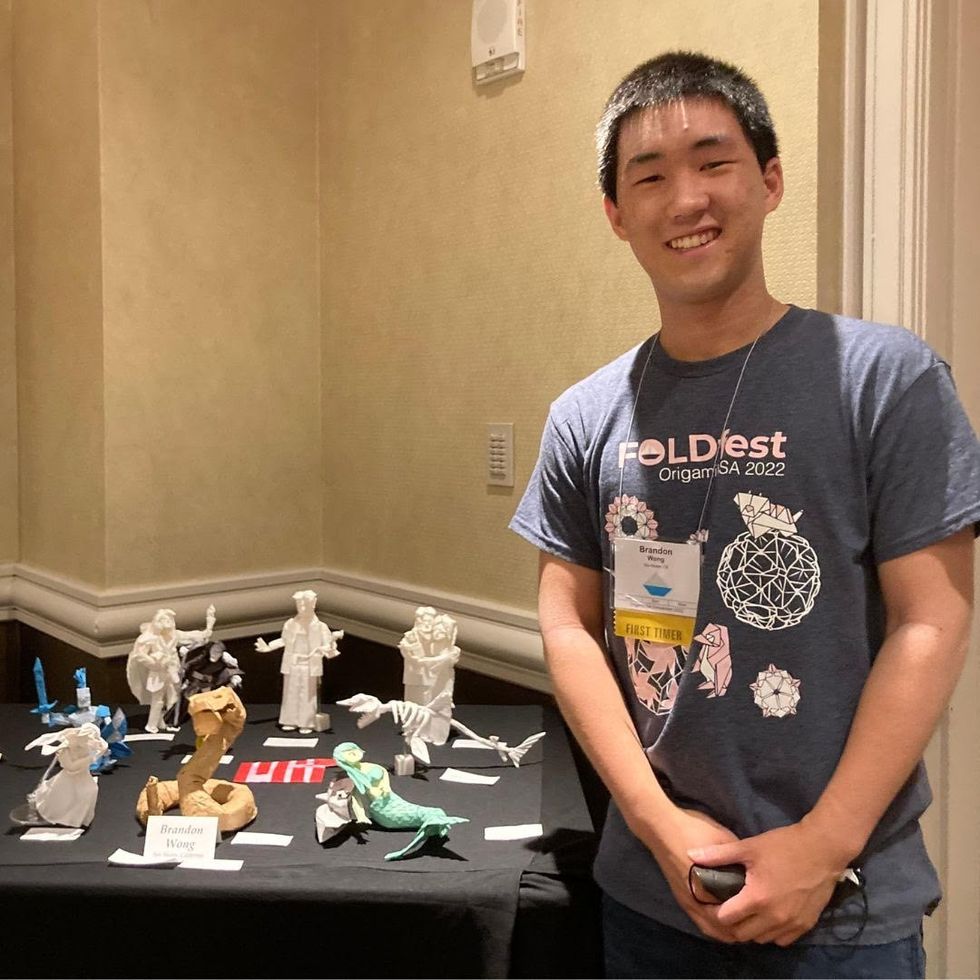
Brandon Wong displaying origami figures he folded at an Origami Convention in 2022
Sharon Wong
Clinical trials
Results from DBV's phase 3 trial in children ages 1 to 3 show its potential. For a positive result, patients who could not tolerate 10 milligrams or less of peanut protein had to be able to manage 300 mg or more after 12 months. Toddlers who could already tolerate more than 10 mg needed to be able to manage 1000 mg or more. In the end, 67 percent of subjects using the Viaskin patch met the target as compared to 33 percent of patients taking the placebo dose.
“The Viaskin peanut patch has been studied in several clinical trials to date with promising results,” says Suzanne M. Barshow, assistant professor of medicine in allergy and asthma research at Stanford University School of Medicine in the U.S. “The data shows that it is safe and well-tolerated. Compared to oral immunotherapy, treatment with the patch results in fewer side effects but appears to be less effective in achieving desensitization.”
The primary reason the patch is less potent is that oral immunotherapy uses a larger amount of the allergen. Additionally, absorption of the peanut protein into the skin could be erratic.
Gray also highlights that there is some tradeoff between risk and efficacy.
“The peanut patch is an exciting advance but not as effective as the oral route,” Gray says. “For those patients who are very sensitive to orally ingested peanut in oral immunotherapy or have an aversion to oral peanut, it has a use. So, essentially, the form of immunotherapy will have to be tailored to each patient.” Having different forms such as the Viaskin patch which is applied to the skin or pills that patients can swallow or dissolve under the tongue is helpful.
The hope is that the patch’s efficacy will increase over time. The team is currently running a follow-up trial, where the same patients continue using the patch.
“It is a very important study to show whether the benefit achieved after 12 months on the patch stays stable or hopefully continues to grow with longer duration,” says Kim, who is an investigator in this follow-up trial.
"My son now attends university in Massachusetts, lives on-campus, and eats dorm food. He has so much more freedom," Wong says.
The team is further ahead in the phase 3 follow-up trial for 4-to-11-year-olds. The initial phase 3 trial was not as successful as the trial for kids between one and three. The patch enabled patients to tolerate more peanuts but there was not a significant enough difference compared to the placebo group to be definitive. The follow-up trial showed greater potency. It suggests that the longer patients are on the patch, the stronger its effects.
They’re also testing if making the patch bigger, changing the shape and extending the minimum time it’s worn can improve its benefits in a trial for a new group of 4-to-11 year-olds.
The future
DBV Technologies is using the skin patch to treat cow’s milk allergies in children ages 1 to 17. They’re currently in phase 2 trials.
As for the peanut allergy trials in toddlers, the hope is to see more efficacy soon.
For Wong’s son who took part in the earlier phase 2 trial for 4-to-11-year-olds, the patch has transformed his life.
“My son continues to maintain his peanut tolerance and is not affected by peanut dust in the air or cross-contact,” Wong says. ”He attends university in Massachusetts, lives on-campus, and eats dorm food. He still carries an EpiPen but has so much more freedom than before his clinical trial. We will always be grateful.”
Scientists aim to preserve donkeys, one frozen embryo at a time
In Ethiopia, Samuna’s three donkeys help her transport produce to market and to collect the water essential to her family, neighbours and livestock. Donkeys are more endangered than people realize, experts say.
Every day for a week in 2022, Andres Gambini, a veterinarian and senior lecturer in animal science at the University of Queensland in Australia, walked into his lab—and headed straight to the video camera. Trained on an array of about 50 donkey embryos, all created by Gambini’s manual in vitro fertilization, or IVF, the camera kept an eye on their developmental progress. To eventually create a viable embryo that could be implanted into a female donkey, the embryos’ cells had to keep dividing, first in two, then in four and so on.
But the embryos weren’t cooperating. Some would start splitting up only to stop a day or two later, and others wouldn’t start at all. Every day he came in, Gambini saw fewer and fewer dividing embryos, so he was losing faith in the effort. “You see many failed attempts and get disappointed,” he says.
Gambini and his team, a group of Argentinian and Spanish researchers, were working to create these embryos because many donkey populations around the world are declining. It may sound counterintuitive that domesticated animals may need preservation, but out of 28 European donkey breeds, 20 are endangered and seven are in critical status. It is partly because of the inbreeding that happened over the course of many years and partly because in today’s Western world donkeys aren’t really used anymore.
“That's the reason why some breeds begin to disappear because humans were not really interested in having that specific breed anymore,” Gambini says. Nonetheless, in Africa, India and Latin America millions of rural families still rely on these hardy creatures for agriculture and transportation. And the only two wild donkey species—Equus africanus in Africa and Equus hemionus in Asia—are also dwindling, due to losing their habitats to human activities, diseases and slow reproduction rates. Gambini’s team wanted to create a way to preserve the animals for the future. “Donkeys are more endangered than people realize,” he says.
There’s much more to donkeys' trouble though. For the past 20 or so years, they have been facing a huge existential threat due to their hide gelatin, a compound derived from their skins by soaking and stewing. In Chinese traditional medicine, the compound, called ejiao, is believed to have a medicinal value, so it’s used in skin creams, added to food and taken in capsules. Centuries ago, ejiao was a very expensive luxury product available only for the emperor and his household. That changed in the 1990s when the Chinese economy boomed, and many people were suddenly able to afford it. “It went from a very elite product to a very popular product,” says Janneke Merkx, a campaign manager at The Donkey Sanctuary, a United Kingdom-based nonprofit organization that keeps tabs on the animals’ welfare worldwide. “It is a status symbol for gift giving.”
Having evolved in the harsh and arid mountainous terrains where food and water were scarce, donkeys are extremely adaptable and hardy. But the Donkey Sanctuary documented cases in which an entire village had their animals disappear overnight, finding them killed and skinned outside their settlement.
The Chinese donkey population was quickly decimated. Unlike many other farm animals, donkeys are finicky breeders. When stressed and unhappy, they don’t procreate, so growing them in large industrial settings isn’t possible. “Donkeys are notoriously slow breeders and really very difficult to farm,” says Merkx. “They are not the same as other livestock like sheep and pigs and cattle.” Within years the, the donkey numbers in China dropped precipitously. “China used to have the largest donkey population in the world in the 1990s. They had 11 million donkeys, and it's now down to less than 3 million, and they just can't keep up with the demand.”
To keep the ejiao conveyor going, some producers turned to the illegal wildlife trade. Poachers began to steal and slaughter donkeys from rural villages in Africa. The Donkey Sanctuary documented cases in which an entire village had their animals disappear overnight, finding them killed and skinned outside their settlement. Exactly how many creatures were lost to the skin trade to-date isn’t possible to calculate, says Faith Burden, the Donkey Sanctuary’s director of equine operations. Traditionally a poor people’s beast of burden, donkey counts are hard to keep track of. “When an animal doesn't produce meat, milk or eggs or whatever edible product, they're often less likely to be acknowledged in a government population census,” Burden says. “So reliable statistics are hard to come by.” The nonprofit estimates that about 4.8 million are slaughtered annually.
During their six to seven thousand years of domestication, donkeys rarely got the full appreciation for their services. They are often compared to horses, which doesn’t do them justice. They’re entirely different animals, Burden says. Built for speed, horses respond to predators and other dangers by running as fast as they can. Donkeys, which originate from the rocky, mountainous regions of Africa where running is dangerous, react to threats by freezing and assessing the situation for the best response. “Those so-called stubborn donkeys that won’t move as you want, they are actually thinking ‘what’s the best approach,’” Burden says. They may even choose to fight the predators rather than flee, she adds. “In some parts of the world, people use them as guard animals against things like coyotes and wolves.”
Scientists believe that domestic donkeys take their origin from Equus africanus or African wild ass, originally roaming where Kenya, Ethiopia and Eritrea are today. Having evolved in the harsh and arid mountainous terrains where food and water were scarce, they are extremely adaptable and hardy. Research finds that they can go without water for 72 hours and then drink their fill without any negative consequences. Their big jaws let them chew tough desert shrubs, which horses can’t exist on. Their large ears help dissipate heat. Their little upright hooves are a perfect fit for the uneven rocky or other dangerous grounds. Accustomed to the mountain desert climate with hot days and cold nights, they don’t mind temperature flux.
“The donkey is the most supremely adapted animal to deal with hostile conditions,” Burden says. “They can survive on much lower nutritional quality food than a cow, sheep or horse. That’s why communities living in some of the most inhospitable places will often have donkeys with them.” And that’s why losing a donkey to an illegal skin trade can devastate a family in places like Eritrea. Suddenly everything from water to firewood to produce must be carried by family members—and often women.

Workers unloading donkeys at the Shinyanga slaughterhouse in Tanzania. Fearing a future in which donkeys go extinct, scientists have found ways to cryopreserve a donkey embryo in liquid nitrogen.
TAHUCHA
One can imagine a time when worldwide donkey populations may dwindle to the point that they would need to be restored. That includes their genetic variability too. That’s where the frozen embryos may come in handy. We may be able to use them to increase the genetic variability of donkeys, which will be especially important if they get closer to extinction, Gambini says. His team had already created frozen embryos for horses and zebras, an idea similar to a seed bank. “We call this concept the Frozen Zoo.”
Creating donkey embryos proved much harder than those of zebras and horses. To improve chances of fertilization, Gambini used the intracytoplasmic sperm injection or ICSI, in which he employed a tiny needle called a micropipette to inject a donkey sperm into an egg. That was a step above the traditional IVF method, in which the egg and a sperm are left floating in a test tube together. The injection took, but during the incubating week, one after the other, the embryos stopped dividing. Finally, on day seven, Gambini finally spotted the exact sight he was hoping to see. One of the embryos developed into a burgeoning ball of cells.
“That stage is called a blastocyst,” Gambini says. The clump of cells had a lot of fluids mixed within them, which indicated that they were finally developing into a viable embryo. “When we see a blastocyst, we know we can transfer that into a female.” He was so excited he immediately called all his collaborators to tell them the good news, which they later published in the journal of Theriogenology.
The one and only embryo to reach that stage, the blastocyst was cryopreserved in liquid nitrogen. The team is waiting for the next breeding season to see if a female donkey may carry it to term and give birth to a healthy foal. Gambini’s team is hoping to polish the process and create more embryos. “It’s our weapon in the conservation ass-enal,” he says.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.

