New gene therapy helps patients with rare disease. One mother wouldn't have it any other way.
A biotech in Cambridge, Mass., is targeting a rare disease called cystinosis with gene therapy. It's been effective for five patients in a clinical trial that's still underway.
Three years ago, Jordan Janz of Consort, Alberta, knew his gene therapy treatment for cystinosis was working when his hair started to darken. Pigmentation or melanin production is just one part of the body damaged by cystinosis.
“When you have cystinosis, you’re either a redhead or a blonde, and you are very pale,” attests Janz, 23, who was diagnosed with the disease just eight months after he was born. “After I got my new stem cells, my hair came back dark, dirty blonde, then it lightened a little bit, but before it was white blonde, almost bleach blonde.”
According to Cystinosis United, about 500 to 600 people have the rare genetic disease in the U.S.; an estimated 20 new cases are diagnosed each year.
Located in Cambridge, Mass., AVROBIO is a gene therapy company that targets cystinosis and other lysosomal storage disorders, in which toxic materials build up in the cells. Janz is one of five patients in AVROBIO’s ongoing Phase 1/2 clinical trial of a gene therapy for cystinosis called AVR-RD-04.
Recently, AVROBIO compiled positive clinical data from this first and only gene therapy trial for the disease. The data show the potential of the therapy to genetically modify the patients’ own hematopoietic stem cells—a certain type of cell that’s capable of developing into all different types of blood cells—to express the functional protein they are deficient in. It stabilizes or reduces the impact of cystinosis on multiple tissues with a single dose.
Medical researchers have found that more than 80 different mutations to a gene called CTNS are responsible for causing cystinosis. The most common mutation results in a deficiency of the protein cystinosin. That protein functions as a transporter that regulates a lot metabolic processes in the cells.
“One of the first things we see in patients clinically is an accumulation of a particular amino acid called cystine, which grows toxic cystine crystals in the cells that cause serious complications,” explains Essra Rihda, chief medical officer for AVROBIO. “That happens in the cells across the tissues and organs of the body, so the disease affects many parts of the body.”

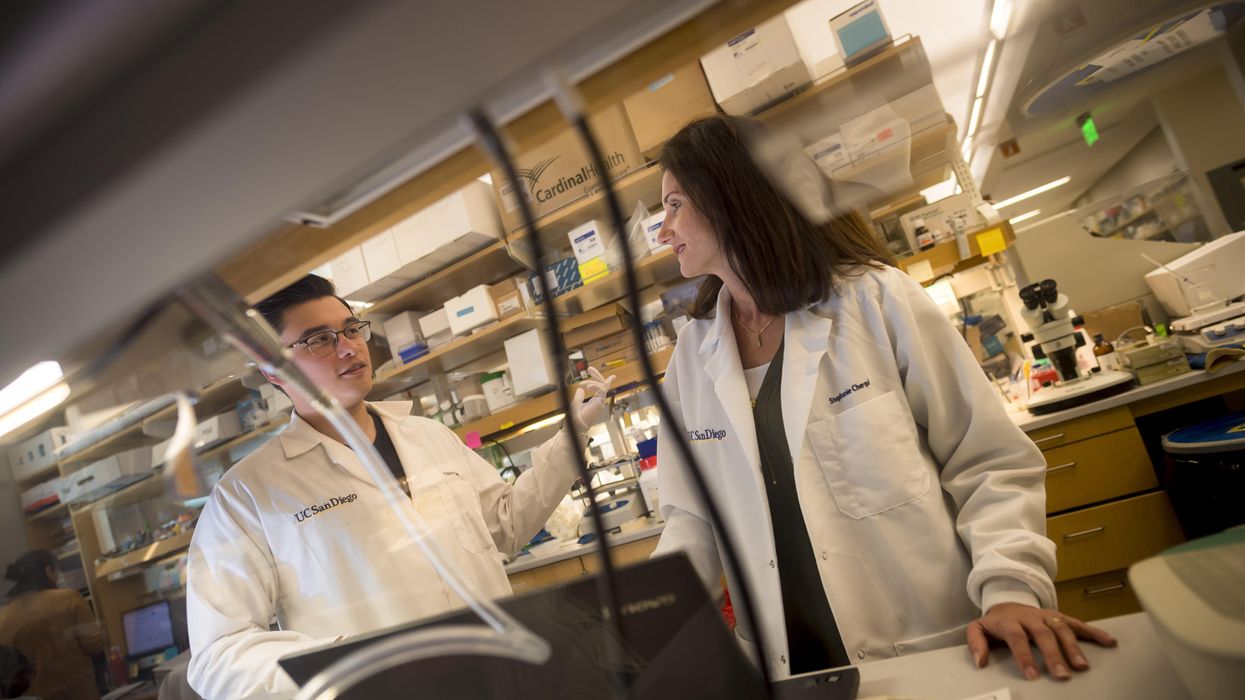
Jordan Janz, 23, meets Stephanie Cherqui, the principal investigator of his gene therapy trial, before the trial started in 2019.
Jordan Janz
According to Rihda, although cystinosis can occur in kids and adults, the most severe form of the disease affects infants and makes up about 95 percent of overall cases. Children typically appear healthy at birth, but around six to 18 months, they start to present for medical attention with failure to thrive.
Additionally, infants with cystinosis often urinate frequently, a sign of polyuria, and they are thirsty all the time, since the disease usually starts in the kidneys. Many develop chronic kidney disease that ultimately progresses to the point where the kidney no longer supports the body’s needs. At that stage, dialysis is required and then a transplant. From there the disease spreads to many other organs, including the eyes, muscles, heart, nervous system, etc.
“The gene for cystinosis is expressed in every single tissue we have, and the accumulation of this toxic buildup alters all of the organs of the patient, so little by little all of the organs start to fail,” says Stephanie Cherqui, principal investigator of Cherqui Lab, which is part of UC San Diego’s Department of Pediatrics.
Since the 1950s, a drug called cysteamine showed some therapeutic effect on cystinosis. It was approved by the FDA in 1994 to prevent damage that may be caused by the buildup of cystine crystals in organs. Prior to FDA approval, Cherqui says, children were dying of the disease before they were ten-years-old or after a kidney transplant. By taking oral cysteamine, they can live from 20 to 50 years longer. But it’s a challenging drug because it has to be taken every 6 or 12 hours, and there are serious gastric side effects such as nausea and diarrhea.
“With all of the complications they develop, the typical patient takes 40 to 60 pills a day around the clock,” Cherqui says. “They literally have a suitcase of medications they have to carry everywhere, and all of those medications don’t stop the progression of the disease, and they still die from it.”
Cherqui has been a proponent of gene therapy to treat children’s disorders since studying cystinosis while earning her doctorate in 2002. Today, her lab focuses on developing stem cell and gene therapy strategies for degenerative, hereditary disorders such as cystinosis that affect multiple systems of the body. “Because cystinosis expresses in every tissue in the body, I decided to use the blood-forming stem cells that we have in our bone marrow,” she explains. “These cells can migrate to anywhere in the body where the person has an injury from the disease.”
AVROBIO’s hematopoietic stem cell gene therapy approach collects stem cells from the patient’s bone marrow. They then genetically modify the stem cells to give the patient a copy of the healthy CTNS gene, which the person either doesn’t have or it’s defective.
The patient first undergoes apheresis, a medical procedure in which their blood is passed through an apparatus that separates out the diseased stem cells, and a process called conditioning is used to help eliminate the damaged cells so they can be replaced by the infusion of the patient’s genetically modified stem cells. Once they become engrafted into the patient’s bone marrow, they reproduce into a lot of daughter cells, and all of those daughter cells contain the CTNS gene. Those cells are able to express the healthy, functional, active protein throughout the body to correct the metabolic problem caused by cystinosis.
“What we’re seeing in the adult patients who have been dosed to date is the consistent and sustained engraftment of our genetically modified cells, 17 to 27 months post-gene therapy, so that’s very encouraging and positive,” says Rihda, the chief medical officer at AVROBIO.
When Janz was 11-years-old, his mother got him enrolled in the trial of a new form of cysteamine that would only need to be taken every 12 hours instead of every six. Two years later, she made sure he was the first person on the list for Cherqui’s current stem cell gene therapy trial.
AVROBIO researchers have also confirmed stabilization or improvement in motor coordination and visual perception in the trial participants, suggesting a potential impact on the neuropathology of the disease. Data from five dosed patients show strong safety and tolerability as well as reduced accumulation of cystine crystals in cells across multiple tissues in the first three patients. None of the five patients need to take oral cysteamine.
Janz’s mother, Barb Kulyk, whom he credits with always making him take his medications and keeping him hydrated, had been following Cherqui’s research since his early childhood. When Janz was 11-years-old, she got him enrolled in the trial of a new form of cysteamine that would only need to be taken every 12 hours instead of every six. When he was 17, the FDA approved that drug. Two years later, his mother made sure he was the first person on the list for Cherqui’s current stem cell gene therapy trial. He received his new stem cells on October 7th, 2019, went home in January 2020, and returned to working full time in February.

Jordan Janz, pictured here with his girlfriend, has a new lease on life, plus a new hair color.
Jordan Janz
He notes that his energy level is significantly better, and his mother has noticed much improvement in him and his daily functioning: He rarely vomits or gets nauseous in the morning, and he has more color in his face as well as his hair. Although he could finish his participation at any time, he recently decided to continue in the clinical trial.
Before the trial, Janz was taking 56 pills daily. He is completely off all of those medications and only takes pills to keep his kidneys working. Because of the damage caused by cystinosis over the course of his life, he’s down to about 20 percent kidney function and will eventually need a transplant.
“Some day, though, thanks to Dr. Cherqui’s team and AVROBIO’s work, when I get a new kidney, cystinosis won’t destroy it,” he concludes.
Here's how one doctor overcame extraordinary odds to help create the birth control pill
Dr. Percy Julian had so many personal and professional obstacles throughout his life, it’s amazing he was able to accomplish anything at all. But this hidden figure not only overcame these incredible obstacles, he also laid the foundation for the creation of the birth control pill.
Julian’s first obstacle was growing up in the Jim Crow-era south in the early part of the twentieth century, where racial segregation kept many African-Americans out of schools, libraries, parks, restaurants, and more. Despite limited opportunities and education, Julian was accepted to DePauw University in Indiana, where he majored in chemistry. But in college, Julian encountered another obstacle: he wasn’t allowed to stay in DePauw’s student housing because of segregation. Julian found lodging in an off-campus boarding house that refused to serve him meals. To pay for his room, board, and food, Julian waited tables and fired furnaces while he studied chemistry full-time. Incredibly, he graduated in 1920 as valedictorian of his class.
After graduation, Julian landed a fellowship at Harvard University to study chemistry—but here, Julian ran into yet another obstacle. Harvard thought that white students would resent being taught by Julian, an African-American man, so they withdrew his teaching assistantship. Julian instead decided to complete his PhD at the University of Vienna in Austria. When he did, he became one of the first African Americans to ever receive a PhD in chemistry.
Julian received offers for professorships, fellowships, and jobs throughout the 1930s, due to his impressive qualifications—but these offers were almost always revoked when schools or potential employers found out Julian was black. In one instance, Julian was offered a job at the Institute of Paper Chemistory in Appleton, Wisconsin—but Appleton, like many cities in the United States at the time, was known as a “sundown town,” which meant that black people weren’t allowed to be there after dark. As a result, Julian lost the job.
During this time, Julian became an expert at synthesis, which is the process of turning one substance into another through a series of planned chemical reactions. Julian synthesized a plant compound called physostigmine, which would later become a treatment for an eye disease called glaucoma.
In 1936, Julian was finally able to land—and keep—a job at Glidden, and there he found a way to extract soybean protein. This was used to produce a fire-retardant foam used in fire extinguishers to smother oil and gasoline fires aboard ships and aircraft carriers, and it ended up saving the lives of thousands of soldiers during World War II.
At Glidden, Julian found a way to synthesize human sex hormones such as progesterone, estrogen, and testosterone, from plants. This was a hugely profitable discovery for his company—but it also meant that clinicians now had huge quantities of these hormones, making hormone therapy cheaper and easier to come by. His work also laid the foundation for the creation of hormonal birth control: Without the ability to synthesize these hormones, hormonal birth control would not exist.
Julian left Glidden in the 1950s and formed his own company, called Julian Laboratories, outside of Chicago, where he manufactured steroids and conducted his own research. The company turned profitable within a year, but even so Julian’s obstacles weren’t over. In 1950 and 1951, Julian’s home was firebombed and attacked with dynamite, with his family inside. Julian often had to sit out on the front porch of his home with a shotgun to protect his family from violence.
But despite years of racism and violence, Julian’s story has a happy ending. Julian’s family was eventually welcomed into the neighborhood and protected from future attacks (Julian’s daughter lives there to this day). Julian then became one of the country’s first black millionaires when he sold his company in the 1960s.
When Julian passed away at the age of 76, he had more than 130 chemical patents to his name and left behind a body of work that benefits people to this day.
Therapies for Healthy Aging with Dr. Alexandra Bause
My guest today is Dr. Alexandra Bause, a biologist who has dedicated her career to advancing health, medicine and healthier human lifespans. Dr. Bause co-founded a company called Apollo Health Ventures in 2017. Currently a venture partner at Apollo, she's immersed in the discoveries underway in Apollo’s Venture Lab while the company focuses on assembling a team of investors to support progress. Dr. Bause and Apollo Health Ventures say that biotech is at “an inflection point” and is set to become a driver of important change and economic value.
Previously, Dr. Bause worked at the Boston Consulting Group in its healthcare practice specializing in biopharma strategy, among other priorities
She did her PhD studies at Harvard Medical School focusing on molecular mechanisms that contribute to cellular aging, and she’s also a trained pharmacist
In the episode, we talk about the present and future of therapeutics that could increase people’s spans of health, the benefits of certain lifestyle practice, the best use of electronic wearables for these purposes, and much more.
Dr. Bause is at the forefront of developing interventions that target the aging process with the aim of ensuring that all of us can have healthier, more productive lifespans.


