New tools could catch disease outbreaks earlier - or predict them

A team at the Catalan Institution for Research and Advanced Studies is utilizing drones and weather stations to collect data on how mosquito breeding patterns are changing in response to climate shifts.
Every year, the villages which lie in the so-called ‘Nipah belt’— which stretches along the western border between Bangladesh and India, brace themselves for the latest outbreak. For since 1998, when Nipah virus—a form of hemorrhagic fever most common in Bangladesh—first spilled over into humans, it has been a grim annual visitor to the people of this region.
With a 70 percent fatality rate, no vaccine, and no known treatments, Nipah virus has been dubbed in the Western world as ‘the worst disease no one has ever heard of.’ Currently, outbreaks tend to be relatively contained because it is not very transmissible. The virus circulates throughout Asia in fruit eating bats, and only tends to be passed on to people who consume contaminated date palm sap, a sweet drink which is harvested across Bangladesh.
But as SARS-CoV-2 has shown the world, this can quickly change.
“Nipah virus is among what virologists call ‘the Big 10,’ along with things like Lassa fever and Crimean Congo hemorrhagic fever,” says Noam Ross, a disease ecologist at New York-based non-profit EcoHealth Alliance. “These are pretty dangerous viruses from a lethality perspective, which don’t currently have the capacity to spread into broader human populations. But that can evolve, and you could very well see a variant emerge that has human-human transmission capability.”
That’s not an overstatement. Surveys suggest that mammals harbour about 40,000 viruses, with roughly a quarter capable of infecting humans. The vast majority never get a chance to do so because we don’t encounter them, but climate change can alter that. Recent studies have found that as animals relocate to new habitats due to shifting environmental conditions, the coming decades will bring around 300,000 first encounters between species which normally don’t interact, especially in tropical Africa and southeast Asia. All these interactions will make it far more likely for hitherto unknown viruses to cross paths with humans.
That’s why for the last 16 years, EcoHealth Alliance has been conducting ongoing viral surveillance projects across Bangladesh. The goal is to understand why Nipah is so much more prevalent in the western part of the country, compared to the east, and keep a watchful eye out for new Nipah strains as well as other dangerous pathogens like Ebola.
"There are a lot of different infectious agents that are sensitive to climate change that don't have these sorts of software tools being developed for them," says Cat Lippi, medical geography researcher at the University of Florida.
Until very recently this kind of work has been hampered by the limitations of viral surveillance technology. The PREDICT project, a $200 million initiative funded by the United States Agency for International Development, which conducted surveillance across the Amazon Basin, Congo Basin and extensive parts of South and Southeast Asia, relied upon so-called nucleic acid assays which enabled scientists to search for the genetic material of viruses in animal samples.
However, the project came under criticism for being highly inefficient. “That approach requires a big sampling effort, because of the rarity of individual infections,” says Ross. “Any particular animal may be infected for a couple of weeks, maybe once or twice in its lifetime. So if you sample thousands and thousands of animals, you'll eventually get one that has an Ebola virus infection right now.”
Ross explains that there is now far more interest in serological sampling—the scientific term for the process of drawing blood for antibody testing. By searching for the presence of antibodies in the blood of humans and animals, scientists have a greater chance of detecting viruses which started circulating recently.
Despite the controversy surrounding EcoHealth Alliance’s involvement in so-called gain of function research—experiments that study whether viruses might mutate into deadlier strains—the organization’s separate efforts to stay one step ahead of pathogen evolution are key to stopping the next pandemic.
“Having really cheap and fast surveillance is really important,” says Ross. “Particularly in a place where there's persistent, low level, moderate infections that potentially have the ability to develop into more epidemic or pandemic situations. It means there’s a pathway that something more dangerous can come through."

Scientists are searching for the presence of antibodies in the blood of humans and animals in hopes to detect viruses that recently started circulating.
EcoHealth Alliance
In Bangladesh, EcoHealth Alliance is attempting to do this using a newer serological technology known as a multiplex Luminex assay, which tests samples against a panel of known antibodies against many different viruses. It collects what Ross describes as a ‘footprint of information,’ which allows scientists to tell whether the sample contains the presence of a known pathogen or something completely different and needs to be investigated further.
By using this technology to sample human and animal populations across the country, they hope to gain an idea of whether there are any novel Nipah virus variants or strains from the same family, as well as other deadly viral families like Ebola.
This is just one of several novel tools being used for viral discovery in surveillance projects around the globe. Multiple research groups are taking PREDICT’s approach of looking for novel viruses in animals in various hotspots. They collect environmental DNA—mucus, faeces or shed skin left behind in soil, sediment or water—which can then be genetically sequenced.
Five years ago, this would have been a painstaking work requiring bringing collected samples back to labs. Today, thanks to the vast amounts of money spent on new technologies during COVID-19, researchers now have portable sequencing tools they can take out into the field.
Christopher Jerde, a researcher at the UC Santa Barbara Marine Science Institute, points to the Oxford Nanopore MinION sequencer as one example. “I tried one of the early versions of it four years ago, and it was miserable,” he says. “But they’ve really improved, and what we’re going to be able to do in the next five to ten years will be amazing. Instead of having to carefully transport samples back to the lab, we're going to have cigar box-shaped sequencers that we take into the field, plug into a laptop, and do the whole sequencing of an organism.”
In the past, viral surveillance has had to be very targeted and focused on known families of viruses, potentially missing new, previously unknown zoonotic pathogens. Jerde says that the rise of portable sequencers will lead to what he describes as “true surveillance.”
“Before, this was just too complex,” he says. “It had to be very focused, for example, looking for SARS-type viruses. Now we’re able to say, ‘Tell us all the viruses that are here?’ And this will give us true surveillance – we’ll be able to see the diversity of all the pathogens which are in these spots and have an understanding of which ones are coming into the population and causing damage.”
But being able to discover more viruses also comes with certain challenges. Some scientists fear that the speed of viral discovery will soon outpace the human capacity to analyze them all and assess the threat that they pose to us.
“I think we're already there,” says Jason Ladner, assistant professor at Northern Arizona University’s Pathogen and Microbiome Institute. “If you look at all the papers on the expanding RNA virus sphere, there are all of these deposited partial or complete viral sequences in groups that we just don't know anything really about yet.” Bats, for example, carry a myriad of viruses, whose ability to infect human cells we understand very poorly.
Cultivating these viruses under laboratory conditions and testing them on organoids— miniature, simplified versions of organs created from stem cells—can help with these assessments, but it is a slow and painstaking work. One hope is that in the future, machine learning could help automate this process. The new SpillOver Viral Risk Ranking platform aims to assess the risk level of a given virus based on 31 different metrics, while other computer models have tried to do the same based on the similarity of a virus’s genomic sequence to known zoonotic threats.
However, Ladner says that these types of comparisons are still overly simplistic. For one thing, scientists are still only aware of a few hundred zoonotic viruses, which is a very limited data sample for accurately assessing a novel pathogen. Instead, he says that there is a need for virologists to develop models which can determine viral compatibility with human cells, based on genomic data.
“One thing which is really useful, but can be challenging to do, is understand the cell surface receptors that a given virus might use,” he says. “Understanding whether a virus is likely to be able to use proteins on the surface of human cells to gain entry can be very informative.”
As the Earth’s climate heats up, scientists also need to better model the so-called vector borne diseases such as dengue, Zika, chikungunya and yellow fever. Transmitted by the Aedes mosquito residing in humid climates, these blights currently disproportionally affect people in low-income nations. But predictions suggest that as the planet warms and the pests find new homes, an estimated one billion people who currently don’t encounter them might be threatened by their bites by 2080. “When it comes to mosquito-borne diseases we have to worry about shifts in suitable habitat,” says Cat Lippi, a medical geography researcher at the University of Florida. “As climate patterns change on these big scales, we expect to see shifts in where people will be at risk for contracting these diseases.”
Public health practitioners and government decision-makers need tools to make climate-informed decisions about the evolving threat of different infectious diseases. Some projects are already underway. An ongoing collaboration between the Catalan Institution for Research and Advanced Studies and researchers in Brazil and Peru is utilizing drones and weather stations to collect data on how mosquitoes change their breeding patterns in response to climate shifts. This information will then be fed into computer algorithms to predict the impact of mosquito-borne illnesses on different regions.

The team at the Catalan Institution for Research and Advanced Studies is using drones and weather stations to collect data on how mosquito breeding patterns change due to climate shifts.
Gabriel Carrasco
Lippi says that similar models are urgently needed to predict how changing climate patterns affect respiratory, foodborne, waterborne and soilborne illnesses. The UK-based Wellcome Trust has allocated significant assets to fund such projects, which should allow scientists to monitor the impact of climate on a much broader range of infections. “There are a lot of different infectious agents that are sensitive to climate change that don't have these sorts of software tools being developed for them,” she says.
COVID-19’s havoc boosted funding for infectious disease research, but as its threats begin to fade from policymakers’ focus, the money may dry up. Meanwhile, scientists warn that another major infectious disease outbreak is inevitable, potentially within the next decade, so combing the planet for pathogens is vital. “Surveillance is ultimately a really boring thing that a lot of people don't want to put money into, until we have a wide scale pandemic,” Jerde says, but that vigilance is key to thwarting the next deadly horror. “It takes a lot of patience and perseverance to keep looking.”
This article originally appeared in One Health/One Planet, a single-issue magazine that explores how climate change and other environmental shifts are increasing vulnerabilities to infectious diseases by land and by sea. The magazine probes how scientists are making progress with leaders in other fields toward solutions that embrace diverse perspectives and the interconnectedness of all lifeforms and the planet.
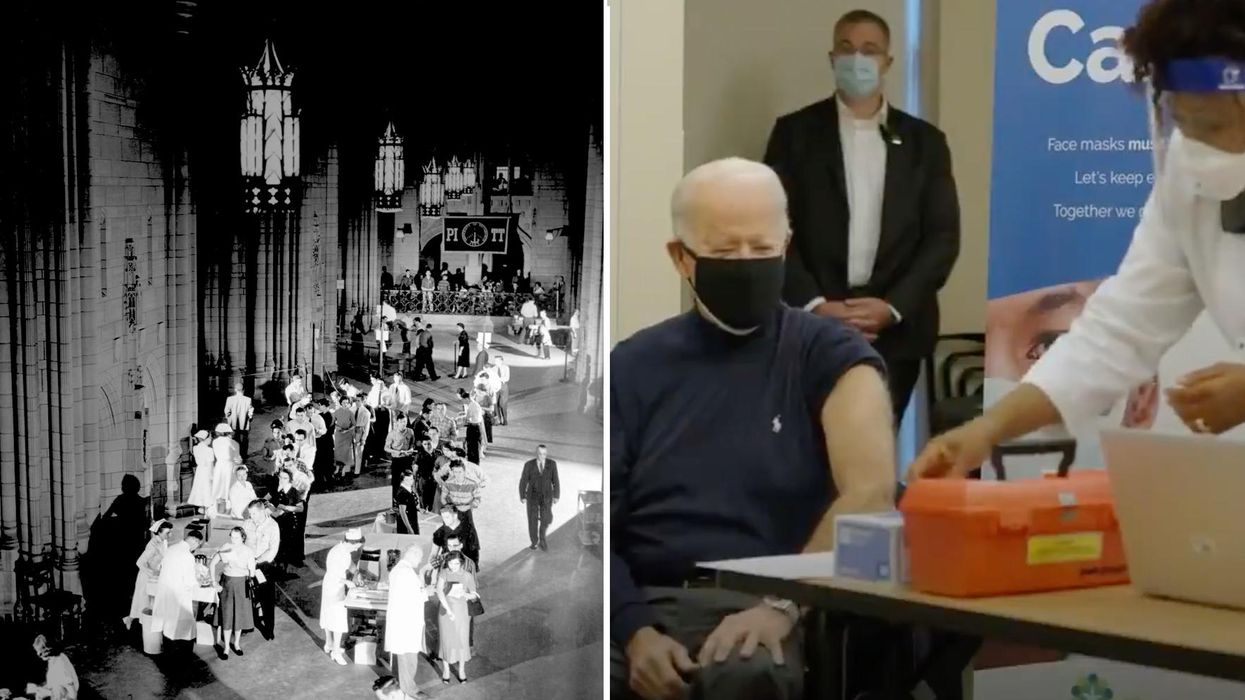
On left, people excitedly line up for Salk's polio vaccine in 1957; on right, Joe Biden gets one of the COVID vaccines on December 21, 2020.
On the morning of April 12, 1955, newsrooms across the United States inked headlines onto newsprint: the Salk Polio vaccine was "safe, effective, and potent." This was long-awaited news. Americans had limped through decades of fear, unaware of what caused polio or how to cure it, faced with the disease's terrifying, visible power to paralyze and kill, particularly children.
The announcement of the polio vaccine was celebrated with noisy jubilation: church bells rang, factory whistles sounded, people wept in the streets. Within weeks, mass inoculation began as the nation put its faith in a vaccine that would end polio.
Today, most of us are blissfully ignorant of child polio deaths, making it easier to believe that we have not personally benefited from the development of vaccines. According to Dr. Steven Pinker, cognitive psychologist and author of the bestselling book Enlightenment Now, we've become blasé to the gifts of science. "The default expectation is not that disease is part of life and science is a godsend, but that health is the default, and any disease is some outrage," he says.
We're now in the early stages of another vaccine rollout, one we hope will end the ravages of the COVID-19 pandemic. And yet, the Pfizer, Moderna, and AstraZeneca vaccines are met with far greater hesitancy and skepticism than the polio vaccine was in the 50s.
In 2021, concerns over the speed and safety of vaccine development and technology plague this heroic global effort, but the roots of vaccine hesitancy run far deeper. Vaccine hesitancy has always existed in the U.S., even in the polio era, motivated in part by fears around "living virus" in a bad batch of vaccines produced by Cutter Laboratories in 1955. But in the last half century, we've witnessed seismic cultural shifts—loss of public trust, a rise in misinformation, heightened racial and socioeconomic inequality, and political polarization have all intensified vaccine-related fears and resistance. Making sense of how we got here may help us understand how to move forward.
The Rise and Fall of Public Trust
When the polio vaccine was released in 1955, "we were nearing an all-time high point in public trust," says Matt Baum, Harvard Kennedy School professor and lead author of several reports measuring public trust and vaccine confidence. Baum explains that the U.S. was experiencing a post-war boom following the Allied triumph in WWII, a popular Roosevelt presidency, and the rapid innovation that elevated the country to an international superpower.
The 1950s witnessed the emergence of nuclear technology, a space program, and unprecedented medical breakthroughs, adds Emily Brunson, Texas State University anthropologist and co-chair of the Working Group on Readying Populations for COVID-19 Vaccine. "Antibiotics were a game changer," she states. While before, people got sick with pneumonia for a month, suddenly they had access to pills that accelerated recovery.
During this period, science seemed to hold all the answers; people embraced the idea that we could "come to know the world with an absolute truth," Brunson explains. Doctors were portrayed as unquestioned gods, so Americans were primed to trust experts who told them the polio vaccine was safe.
"The emotional tone of the news has gone downward since the 1940s, and journalists consider it a professional responsibility to cover the negative."
That blind acceptance eroded in the 1960s and 70s as people came to understand that science can be inherently political. "Getting to an absolute truth works out great for white men, but these things affect people socially in radically different ways," Brunson says. As the culture began questioning the white, patriarchal biases of science, doctors lost their god-like status and experts were pushed off their pedestals. This trend continues with greater intensity today, as President Trump has led a campaign against experts and waged a war on science that began long before the pandemic.
The Shift in How We Consume Information
In the 1950s, the media created an informational consensus. The fundamental ideas the public consumed about the state of the world were unified. "People argued about the best solutions, but didn't fundamentally disagree on the factual baseline," says Baum. Indeed, the messaging around the polio vaccine was centralized and consistent, led by President Roosevelt's successful March of Dimes crusade. People of lower socioeconomic status with limited access to this information were less likely to have confidence in the vaccine, but most people consumed media that assured them of the vaccine's safety and mobilized them to receive it.
Today, the information we consume is no longer centralized—in fact, just the opposite. "When you take that away, it's hard for people to know what to trust and what not to trust," Baum explains. We've witnessed an increase in polarization and the technology that makes it easier to give people what they want to hear, reinforcing the human tendencies to vilify the other side and reinforce our preexisting ideas. When information is engineered to further an agenda, each choice and risk calculation made while navigating the COVID-19 pandemic is deeply politicized.
This polarization maps onto a rise in socioeconomic inequality and economic uncertainty. These factors, associated with a sense of lost control, prime people to embrace misinformation, explains Baum, especially when the situation is difficult to comprehend. "The beauty of conspiratorial thinking is that it provides answers to all these questions," he says. Today's insidious fragmentation of news media accelerates the circulation of mis- and disinformation, reaching more people faster, regardless of veracity or motivation. In the case of vaccines, skepticism around their origin, safety, and motivation is intensified.
Alongside the rise in polarization, Pinker says "the emotional tone of the news has gone downward since the 1940s, and journalists consider it a professional responsibility to cover the negative." Relentless focus on everything that goes wrong further erodes public trust and paints a picture of the world getting worse. "Life saved is not a news story," says Pinker, but perhaps it should be, he continues. "If people were more aware of how much better life was generally, they might be more receptive to improvements that will continue to make life better. These improvements don't happen by themselves."
The Future Depends on Vaccine Confidence
So far, the U.S. has been unable to mitigate the catastrophic effects of the pandemic through social distancing, testing, and contact tracing. President Trump has downplayed the effects and threat of the virus, censored experts and scientists, given up on containing the spread, and mobilized his base to protest masks. The Trump Administration failed to devise a national plan, so our national plan has defaulted to hoping for the "miracle" of a vaccine. And they are "something of a miracle," Pinker says, describing vaccines as "the most benevolent invention in the history of our species." In record-breaking time, three vaccines have arrived. But their impact will be weakened unless we achieve mass vaccination. As Brunson notes, "The technology isn't the fix; it's people taking the technology."
Significant challenges remain, including facilitating widespread access and supporting on-the-ground efforts to allay concerns and build trust with specific populations with historic reasons for distrust, says Brunson. Baum predicts continuing delays as well as deaths from other causes that will be linked to the vaccine.
Still, there's every reason for hope. The new administration "has its eyes wide open to these challenges. These are the kind of problems that are amenable to policy solutions if we have the will," Baum says. He forecasts widespread vaccination by late summer and a bounce back from the economic damage, a "Good News Story" that will bolster vaccine acceptance in the future. And Pinker reminds us that science, medicine, and public health have greatly extended our lives in the last few decades, a trend that can only continue if we're willing to roll up our sleeves.
Scientists Are Working to Develop a Clever Nasal Spray That Tricks the Coronavirus Out of the Body
Biochemist Longxing Cao is working with colleagues at the University of Washington on promising research to disable infectious coronavirus in a person's nose.
Imagine this scenario: you get an annoying cough and a bit of a fever. When you wake up the next morning you lose your sense of taste and smell. That sounds familiar, so you head to a doctor's office for a Covid test, which comes back positive.
Your next step? An anti-Covid nasal spray of course, a "trickster drug" that will clear the once-dangerous and deadly virus out of the body. The drug works by tricking the coronavirus with decoy receptors that appear to be just like those on the surface of our own cells. The virus latches onto the drug's molecules "thinking" it is breaking into human cells, but instead it flushes out of your system before it can cause any serious damage.
This may sounds like science fiction, but several research groups are already working on such trickster coronavirus drugs, with some candidates close to clinical trials and possibly even becoming available late this year. The teams began working on them when the pandemic arrived, and continued in lockdown.
This may sounds like science fiction, but several research groups are already working on such trickster coronavirus drugs, with some candidates close to clinical trials and possibly even becoming available late this year. The teams began working on them when the pandemic arrived, and continued in lockdown.
When the pandemic first hit and the state of California issued a lockdown order on March 16, postdoctoral researchers Anum and Jeff Glasgow found themselves stuck at home with nothing to do. The two scientists who study bioengineering felt that they were well equipped to research molecular ways of disabling coronavirus's cell-penetrating spike protein, but they could no longer come to their labs at the University of California San Francisco.
"We were upset that no one put us in the game," says Anum Glasgow. "We have a lot of experience between us doing these types of projects so we wanted to contribute." But they still had computers so they began modeling the potential virus-disabling proteins in silico using Robetta, special software for designing and modeling protein structures, developed and maintained by University of Washington biochemist David Baker and his lab.
"We saw some imperfections in that lock and key and we created something better. We made a 10 times tighter adhesive."
The SARS-CoV-2 virus that causes Covid-19 uses its surface spike protein to bind on to a specific receptor on human cells called ACE2. Unfortunately for humans, the spike protein's molecular shape fits the ACE2 receptor like a well-cut key, making it very successful at breaking into our cells. But if one could design a molecular ACE2-mimic to "trick" the virus into latching onto it instead, the virus would no longer be able to enter cells. Scientists call such mimics receptor traps or inhibitors, or blockers. "It would block the adhesive part of the virus that binds to human cells," explains Jim Wells, professor of pharmaceutical chemistry at UCSF, whose lab took part in designing the ACE2-receptor mimic, working with the Glasgows and other colleagues.
The idea of disabling infectious or inflammatory agents by tricking them into binding to the targets' molecular look-alikes is something scientists have tried with other diseases. The anti-inflammatory drugs commonly used to treat autoimmune conditions, including rheumatoid arthritis, Crohn's disease and ulcerative colitis, rely on conceptually similar molecular mechanisms. Called TNF blockers, these drugs block the activity of the inflammatory cytokines, molecules that promote inflammation. "One of the biggest selling drugs in the world is a receptor trap," says Jeff Glasgow. "It acts as a receptor decoy. There's a TNF receptor that traps the cytokine."
In the recent past, scientists also pondered a similar look-alike approach to treating urinary tract infections, which are often caused by a pathogenic strain of Escherichia coli. An E. coli bacterium resembles a squid with protruding filaments equipped with proteins that can change their shape to form hooks, used to hang onto specific sugar molecules called ligands, which are present on the surface of the epithelial cells lining the urinary tract.
A recent study found that a sugar-like compound that's structurally similar to that ligand can play a similar trick on the E. Coli. When administered in in sufficient amounts, the compound hooks the bacteria on, which is then excreted out of the body with urine. The "trickster" method had been also tried against the HIV virus, but it wasn't very effective because HIV has a high mutation rate and multiple ways of entering human cells.
But the coronavirus spike protein's shape is more stable. And while it has a strong affinity for the ACE2 receptors, its natural binding to these receptors isn't perfect, which allowed the UCSF researchers to design a mimic with a better grip. "We saw some imperfections in that lock and key and we created something better," says Wells. "We made a 10 times tighter adhesive." The team demonstrated that their traps neutralized SARS-CoV-2 in lab experiments and published their study in the Proceedings of the National Academy of Sciences.
Baker, who is the director of the Institute for Protein Design at the University of Washington, was also devising ACE2 look-alikes with his team. Only unlike the UCSF team, they didn't perfect the virus-receptor lock and key combo, but instead designed their mimics from scratch. Using Robetta, they digitally modeled over two million proteins, zeroed-in on over 100,000 potential candidates and identified a handful with a strong promise of blocking SARS-CoV-2, testing them against the virus in human cells. Their design of the miniprotein inhibitors was published in the journal Science.

Biochemist David Baker, pictured in his lab at the University of Washington.
UW
The concept of the ACE2 receptor mimics is somewhat similar to the antibody plasma, but better, the teams explain. Antibodies don't always coat all of the virus's spike proteins and sometimes don't bind perfectly. By contrast, the ACE2 mimics directly compete with the virus's entry mechanism. ACE2 mimics are also easier and cheaper to make, researchers say.
Antibodies, which are long protein chains, must be grown inside mammalian cells, which is a slow and costly process. As drugs, antibody cocktails must be kept refrigerated. On the contrary, proteins that mimic ACE2 receptors are smaller and can be produced by bacteria easily and inexpensively. Designed to specs, these proteins don't need refrigeration and are easy to store. "We designed them to be very stable," says Baker. "Our computation design tries to come up with the stable proteins that have the desired functions."
That stability may allow the team to create an inhaler drug rather than an intravenous one, which would be another advantage over the antibody plasma, given via an IV. The team envisions people spraying the miniprotein solution into their nose, creating a protecting coating that would disable the inhaled virus. "The infection starts from your respiratory system, from your nose," explains Longxing Cao, the study's co-author—so a nasal spray would be a natural way to administer it. "So that you can have it like a layer, similar to a mask."
As the virus evolves, new variants are arising. But the teams think that their ACE2 protein mimics should work on the new variants too for several reasons. "Since the new SARS-CoV-2 variants still use ACE2 for their cell entry, they will likely still be susceptible to ACE2-based traps," Glasgow says.
Cao explains that their approach should work too because most of the mutations happen outside the ACE2 binding region. Plus, they are building multiple binders that can bind to an array of the coronavirus variants. "Our binder can still bind with most of the variants and we are trying to make one protein that could inhibit all the future escape variants," he says.
Baker and Cao hope that their miniproteins may be available to patients later this year. But besides getting the medicine out to patients, this approach will allow researchers to test the computer-modeled mimics end-to-end with an unprecedented speed. That would give humans a leg up in future pandemics or zoonotic disease outbreaks, which remain an increasingly pressing threat due to human activity and climate change.
"That's what we are focused on right now—understanding what we have learned from this pandemic to improve our design methods," says Baker. "So that we should be able to obtain binders like these very quickly when a new pandemic threat is identified."
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.