New tools could catch disease outbreaks earlier - or predict them

A team at the Catalan Institution for Research and Advanced Studies is utilizing drones and weather stations to collect data on how mosquito breeding patterns are changing in response to climate shifts.
Every year, the villages which lie in the so-called ‘Nipah belt’— which stretches along the western border between Bangladesh and India, brace themselves for the latest outbreak. For since 1998, when Nipah virus—a form of hemorrhagic fever most common in Bangladesh—first spilled over into humans, it has been a grim annual visitor to the people of this region.
With a 70 percent fatality rate, no vaccine, and no known treatments, Nipah virus has been dubbed in the Western world as ‘the worst disease no one has ever heard of.’ Currently, outbreaks tend to be relatively contained because it is not very transmissible. The virus circulates throughout Asia in fruit eating bats, and only tends to be passed on to people who consume contaminated date palm sap, a sweet drink which is harvested across Bangladesh.
But as SARS-CoV-2 has shown the world, this can quickly change.
“Nipah virus is among what virologists call ‘the Big 10,’ along with things like Lassa fever and Crimean Congo hemorrhagic fever,” says Noam Ross, a disease ecologist at New York-based non-profit EcoHealth Alliance. “These are pretty dangerous viruses from a lethality perspective, which don’t currently have the capacity to spread into broader human populations. But that can evolve, and you could very well see a variant emerge that has human-human transmission capability.”
That’s not an overstatement. Surveys suggest that mammals harbour about 40,000 viruses, with roughly a quarter capable of infecting humans. The vast majority never get a chance to do so because we don’t encounter them, but climate change can alter that. Recent studies have found that as animals relocate to new habitats due to shifting environmental conditions, the coming decades will bring around 300,000 first encounters between species which normally don’t interact, especially in tropical Africa and southeast Asia. All these interactions will make it far more likely for hitherto unknown viruses to cross paths with humans.
That’s why for the last 16 years, EcoHealth Alliance has been conducting ongoing viral surveillance projects across Bangladesh. The goal is to understand why Nipah is so much more prevalent in the western part of the country, compared to the east, and keep a watchful eye out for new Nipah strains as well as other dangerous pathogens like Ebola.
"There are a lot of different infectious agents that are sensitive to climate change that don't have these sorts of software tools being developed for them," says Cat Lippi, medical geography researcher at the University of Florida.
Until very recently this kind of work has been hampered by the limitations of viral surveillance technology. The PREDICT project, a $200 million initiative funded by the United States Agency for International Development, which conducted surveillance across the Amazon Basin, Congo Basin and extensive parts of South and Southeast Asia, relied upon so-called nucleic acid assays which enabled scientists to search for the genetic material of viruses in animal samples.
However, the project came under criticism for being highly inefficient. “That approach requires a big sampling effort, because of the rarity of individual infections,” says Ross. “Any particular animal may be infected for a couple of weeks, maybe once or twice in its lifetime. So if you sample thousands and thousands of animals, you'll eventually get one that has an Ebola virus infection right now.”
Ross explains that there is now far more interest in serological sampling—the scientific term for the process of drawing blood for antibody testing. By searching for the presence of antibodies in the blood of humans and animals, scientists have a greater chance of detecting viruses which started circulating recently.
Despite the controversy surrounding EcoHealth Alliance’s involvement in so-called gain of function research—experiments that study whether viruses might mutate into deadlier strains—the organization’s separate efforts to stay one step ahead of pathogen evolution are key to stopping the next pandemic.
“Having really cheap and fast surveillance is really important,” says Ross. “Particularly in a place where there's persistent, low level, moderate infections that potentially have the ability to develop into more epidemic or pandemic situations. It means there’s a pathway that something more dangerous can come through."

Scientists are searching for the presence of antibodies in the blood of humans and animals in hopes to detect viruses that recently started circulating.
EcoHealth Alliance
In Bangladesh, EcoHealth Alliance is attempting to do this using a newer serological technology known as a multiplex Luminex assay, which tests samples against a panel of known antibodies against many different viruses. It collects what Ross describes as a ‘footprint of information,’ which allows scientists to tell whether the sample contains the presence of a known pathogen or something completely different and needs to be investigated further.
By using this technology to sample human and animal populations across the country, they hope to gain an idea of whether there are any novel Nipah virus variants or strains from the same family, as well as other deadly viral families like Ebola.
This is just one of several novel tools being used for viral discovery in surveillance projects around the globe. Multiple research groups are taking PREDICT’s approach of looking for novel viruses in animals in various hotspots. They collect environmental DNA—mucus, faeces or shed skin left behind in soil, sediment or water—which can then be genetically sequenced.
Five years ago, this would have been a painstaking work requiring bringing collected samples back to labs. Today, thanks to the vast amounts of money spent on new technologies during COVID-19, researchers now have portable sequencing tools they can take out into the field.
Christopher Jerde, a researcher at the UC Santa Barbara Marine Science Institute, points to the Oxford Nanopore MinION sequencer as one example. “I tried one of the early versions of it four years ago, and it was miserable,” he says. “But they’ve really improved, and what we’re going to be able to do in the next five to ten years will be amazing. Instead of having to carefully transport samples back to the lab, we're going to have cigar box-shaped sequencers that we take into the field, plug into a laptop, and do the whole sequencing of an organism.”
In the past, viral surveillance has had to be very targeted and focused on known families of viruses, potentially missing new, previously unknown zoonotic pathogens. Jerde says that the rise of portable sequencers will lead to what he describes as “true surveillance.”
“Before, this was just too complex,” he says. “It had to be very focused, for example, looking for SARS-type viruses. Now we’re able to say, ‘Tell us all the viruses that are here?’ And this will give us true surveillance – we’ll be able to see the diversity of all the pathogens which are in these spots and have an understanding of which ones are coming into the population and causing damage.”
But being able to discover more viruses also comes with certain challenges. Some scientists fear that the speed of viral discovery will soon outpace the human capacity to analyze them all and assess the threat that they pose to us.
“I think we're already there,” says Jason Ladner, assistant professor at Northern Arizona University’s Pathogen and Microbiome Institute. “If you look at all the papers on the expanding RNA virus sphere, there are all of these deposited partial or complete viral sequences in groups that we just don't know anything really about yet.” Bats, for example, carry a myriad of viruses, whose ability to infect human cells we understand very poorly.
Cultivating these viruses under laboratory conditions and testing them on organoids— miniature, simplified versions of organs created from stem cells—can help with these assessments, but it is a slow and painstaking work. One hope is that in the future, machine learning could help automate this process. The new SpillOver Viral Risk Ranking platform aims to assess the risk level of a given virus based on 31 different metrics, while other computer models have tried to do the same based on the similarity of a virus’s genomic sequence to known zoonotic threats.
However, Ladner says that these types of comparisons are still overly simplistic. For one thing, scientists are still only aware of a few hundred zoonotic viruses, which is a very limited data sample for accurately assessing a novel pathogen. Instead, he says that there is a need for virologists to develop models which can determine viral compatibility with human cells, based on genomic data.
“One thing which is really useful, but can be challenging to do, is understand the cell surface receptors that a given virus might use,” he says. “Understanding whether a virus is likely to be able to use proteins on the surface of human cells to gain entry can be very informative.”
As the Earth’s climate heats up, scientists also need to better model the so-called vector borne diseases such as dengue, Zika, chikungunya and yellow fever. Transmitted by the Aedes mosquito residing in humid climates, these blights currently disproportionally affect people in low-income nations. But predictions suggest that as the planet warms and the pests find new homes, an estimated one billion people who currently don’t encounter them might be threatened by their bites by 2080. “When it comes to mosquito-borne diseases we have to worry about shifts in suitable habitat,” says Cat Lippi, a medical geography researcher at the University of Florida. “As climate patterns change on these big scales, we expect to see shifts in where people will be at risk for contracting these diseases.”
Public health practitioners and government decision-makers need tools to make climate-informed decisions about the evolving threat of different infectious diseases. Some projects are already underway. An ongoing collaboration between the Catalan Institution for Research and Advanced Studies and researchers in Brazil and Peru is utilizing drones and weather stations to collect data on how mosquitoes change their breeding patterns in response to climate shifts. This information will then be fed into computer algorithms to predict the impact of mosquito-borne illnesses on different regions.

The team at the Catalan Institution for Research and Advanced Studies is using drones and weather stations to collect data on how mosquito breeding patterns change due to climate shifts.
Gabriel Carrasco
Lippi says that similar models are urgently needed to predict how changing climate patterns affect respiratory, foodborne, waterborne and soilborne illnesses. The UK-based Wellcome Trust has allocated significant assets to fund such projects, which should allow scientists to monitor the impact of climate on a much broader range of infections. “There are a lot of different infectious agents that are sensitive to climate change that don't have these sorts of software tools being developed for them,” she says.
COVID-19’s havoc boosted funding for infectious disease research, but as its threats begin to fade from policymakers’ focus, the money may dry up. Meanwhile, scientists warn that another major infectious disease outbreak is inevitable, potentially within the next decade, so combing the planet for pathogens is vital. “Surveillance is ultimately a really boring thing that a lot of people don't want to put money into, until we have a wide scale pandemic,” Jerde says, but that vigilance is key to thwarting the next deadly horror. “It takes a lot of patience and perseverance to keep looking.”
This article originally appeared in One Health/One Planet, a single-issue magazine that explores how climate change and other environmental shifts are increasing vulnerabilities to infectious diseases by land and by sea. The magazine probes how scientists are making progress with leaders in other fields toward solutions that embrace diverse perspectives and the interconnectedness of all lifeforms and the planet.
Announcing "The Future of Science in America: The Election Issue"
This special magazine explores what's at stake for science & policy over the next four years.
As reviewed in The Washington Post, "Tomorrow's challenges in science and politics: Magazine offers in-depth takes on these U.S. issues":
"Is it time for a new way to help make adults more science-literate? What should the next president know about science? Could science help strengthen American democracy? "The Future of Science in America: The Election Issue" has answers. The free, online magazine is packed with interesting takes on how science can serve the common good. And just in time. This year has challenged leaders, researchers and the public with thorny scientific questions, from the coronavirus pandemic to widespread misinformation on scientific issues. The magazine is a collaboration of the Aspen Institute, a think tank that brings together a variety of public figures and private individuals to tackle thorny social issues, the digital science magazine Leapsmag and GOOD, a social impact company. It's packed with 15 in-depth articles about science with a view toward our campaign year."
The Future of Science in America: The Election Issue offers wide-ranging perspectives on challenges and opportunities for science as we elect our next national and local leaders. The fast-striking COVID-19 pandemic and the more slowly moving pandemic of climate change have brought into sharp focus how reliant we will be on science and public policy to work together to rescue us from crisis. Doing so will require cooperation between both political parties, as well as significant public trust in science as a beacon to light the path forward.
In spite of its unfortunate emergence as a flash point between two warring parties, we believe that science is the driving force for universal progress. No endeavor is more noble than the quest to rigorously understand our world and apply that knowledge to further human flourishing. This magazine aspires to promote roadmaps for science as a tool for health, a vehicle for progress, and a unifier of our nation.
This special issue is a collaboration among LeapsMag, the Aspen Institute Science & Society Program, and GOOD, with support from the Gordon and Betty Moore Foundation and the Rita Allen Foundation.
It is available as a free, beautifully designed digital magazine for both desktop and mobile.
TABLE OF CONTENTS:
- SCIENTISTS:
Award-Winning Scientists Offer Advice to the Next President of the United States - PUBLIC OPINION:
National Survey Reveals Americans' Most Important Scientific Priorities - GOVERNMENT:
The Nation's Science and Health Agencies Face a Credibility Crisis: Can Their Reputations Be Restored? - TELEVISION:
To Make Science Engaging, We Need a Sesame Street for Adults - IMMIGRATION:
Immigrant Scientists—and America's Edge—Face a Moment of Truth This Election - RACIAL JUSTICE:
Democratize the White Coat by Honoring Black, Indigenous, and People of Color in Science - EDUCATION:
I'm a Black, Genderqueer Medical Student: Here's My Hard-Won Wisdom for Students and Educational Institutions - TECHNOLOGY:
"Deep Fake" Video Technology Is Advancing Faster Than Our Policies Can Keep Up - VOTERS:
Mind the (Vote) Gap: Can We Get More STEM Students to the Polls? - EXPERTS:
Who Qualifies as an "Expert" and How Can We Decide Who Is Trustworthy? - SOCIAL MEDIA:
Why Your Brain Falls for Misinformation—And How to Avoid It - YOUTH:
Youth Climate Activists Expand Their Focus and Collaborate to Get Out the Vote - SUPREME COURT:
Abortions Before Fetal Viability Are Legal: Might Science and a Change on the Supreme Court Undermine That? - NAVAJO NATION:
An Environmental Scientist and an Educator Highlight Navajo Efforts to Balance Tradition with Scientific Priorities - CIVIC SCIENCE:
Want to Strengthen American Democracy? The Science of Collaboration Can Help
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Scientists Envision a Universal Coronavirus Vaccine
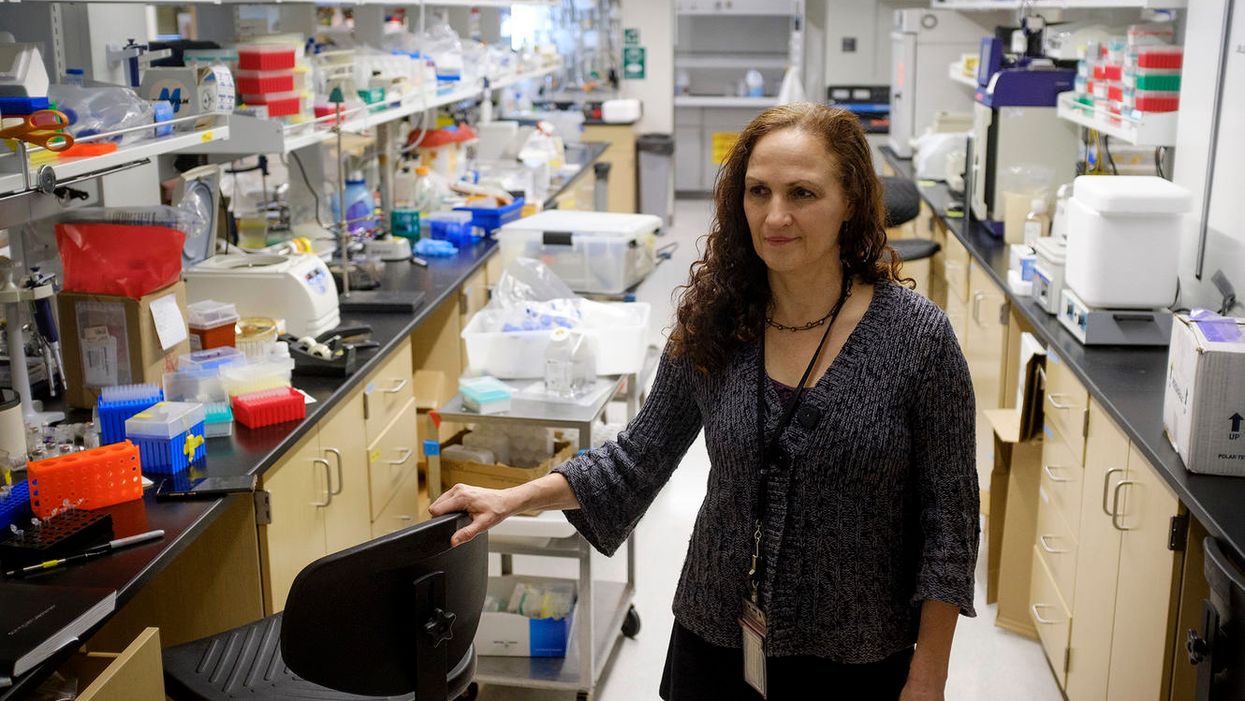
Dr. Deborah Fuller, a professor of microbiology at the Washington University School of Medicine, in her lab.
With several companies progressing through Phase III clinical trials, the much-awaited coronavirus vaccines may finally become reality within a few months.
But some scientists question whether these vaccines will produce a strong and long-lasting immunity, especially if they aren't efficient at mobilizing T-cells, the body's defense soldiers.
"When I look at those vaccines there are pitfalls in every one of them," says Deborah Fuller, professor of microbiology at the Washington University School of Medicine. "Some may induce only transient antibodies, some may not be very good at inducing T-cell responses, and others may not immunize the elderly very well."
Generally, vaccines work by introducing an antigen into the body—either a dead or attenuated pathogen that can't replicate, or parts of the pathogen or its proteins, which the body will recognize as foreign. The pathogens or its parts are usually discovered by cells that chew up the intruders and present them to the immune system fighters, B- and T-cells—like a trespasser's mug shot to the police. In response, B-cells make antibodies to neutralize the virus, and a specialized "crew" called memory B-cells will remember the antigen. Meanwhile, an army of various T-cells attacks the pathogens as well as the cells these pathogens already infected. Special helper T-cells help stimulate B-cells to secrete antibodies and activate cytotoxic T-cells that release chemicals called inflammatory cytokines that kill pathogens and cells they infected.
"Each of these components of the immune system are important and orchestrated to talk to each other," says professor Larry Corey, who studies vaccines and infectious disease at Fred Hutch, a non-profit scientific research organization. "They optimize the assault of the human immune system on the complexity of the viral, bacterial, fungal and parasitic infections that live on our planet, to which we get exposed."
Despite their variety, coronaviruses share certain common proteins and other structural elements, Fuller explains, which the immune system can be trained to identify.
The current frontrunner vaccines aim to train our body to generate a sufficient amount of antibodies to neutralize the virus by shutting off its spike proteins before it enters our cells and begins to replicate. But a truly robust vaccine should also engender a strong response from T-cells, Fuller believes.
"Everyone focuses on the antibodies which block the virus, but it's not always 100 percent effective," she explains. "For example, if there are not enough titers or the antibody starts to wane, and the virus does get into the cells, the cells will become infected. At that point, the body needs to mount a robust T-cytotoxic response. The T-cells should find and recognize cells infected with the virus and eliminate these cells, and the virus with them."
Some of the frontrunner vaccine makers including Moderna, AstraZeneca and CanSino reported that they observed T-cell responses in their trials. Another company, BioNTech, based in Germany, also reported that their vaccine produced T-cell responses.
Fuller and her team are working on their own version of a coronavirus vaccine. In their recent study, the team managed to trigger a strong antibody and T-cell response in mice and primates. Moreover, the aging animals also produced a robust response, which would be important for the human elderly population.
But Fuller's team wants to engage T-cells further. She wants to try training T-cells to recognize not only SARV-CoV-2, but a range of different coronaviruses. Wild hosts, such as bats, carry many different types of coronaviruses, which may spill over onto humans, just like SARS, MERS and SARV-CoV-2 have. There are also four coronaviruses already endemic to humans. Cryptically named 229E, NL63, OC43, and HKU1, they were identified in the 1960s. And while they cause common colds and aren't considered particularly dangerous, the next coronavirus that jumps species may prove deadlier than the previous ones.
Despite their variety, coronaviruses share certain common proteins and other structural elements, Fuller explains, which the immune system can be trained to identify. "T-cells can recognize these shared sequences across multiple different types of coronaviruses," she explains, "so we have this vision for a universal coronavirus vaccine."
Paul Offit at Children's Hospitals in Philadelphia, who specializes in infectious diseases and vaccines, thinks it's a far shot at the moment. "I don't see that as something that is likely to happen, certainly not very soon," he says, adding that a universal flu vaccine has been tried for decades but is not available yet. We still don't know how the current frontrunner vaccines will perform. And until we know how efficient they are, wearing masks and keeping social distance are still important, he notes.
Corey says that while the universal coronavirus vaccine is not impossible, it is certainly not an easy feat. "It is a reasonably scientific hypothesis," he says, but one big challenge is that there are still many unknown coronaviruses so anticipating their structural elements is difficult. The structure of new viruses, particularly the recombinant ones that leap from wild hosts and carry bits and pieces of animal and human genetic material, can be hard to predict. "So whether you can make a vaccine that has universal T-cells to every coronavirus is also difficult to predict," Corey says. But, he adds, "I'm not being negative. I'm just saying that it's a formidable task."
Fuller is certainly up to the task and thinks it's worth the effort. "T-cells can cross-recognize different viruses within the same family," she says, so increasing their abilities to home in on a broader range of coronaviruses would help prevent future pandemics. "If that works, you're just going to take one [vaccine] and you'll have lifetime immunity," she says. "Not just against this coronavirus, but any future pandemic by a coronavirus."
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.