New tools could catch disease outbreaks earlier - or predict them

A team at the Catalan Institution for Research and Advanced Studies is utilizing drones and weather stations to collect data on how mosquito breeding patterns are changing in response to climate shifts.
Every year, the villages which lie in the so-called ‘Nipah belt’— which stretches along the western border between Bangladesh and India, brace themselves for the latest outbreak. For since 1998, when Nipah virus—a form of hemorrhagic fever most common in Bangladesh—first spilled over into humans, it has been a grim annual visitor to the people of this region.
With a 70 percent fatality rate, no vaccine, and no known treatments, Nipah virus has been dubbed in the Western world as ‘the worst disease no one has ever heard of.’ Currently, outbreaks tend to be relatively contained because it is not very transmissible. The virus circulates throughout Asia in fruit eating bats, and only tends to be passed on to people who consume contaminated date palm sap, a sweet drink which is harvested across Bangladesh.
But as SARS-CoV-2 has shown the world, this can quickly change.
“Nipah virus is among what virologists call ‘the Big 10,’ along with things like Lassa fever and Crimean Congo hemorrhagic fever,” says Noam Ross, a disease ecologist at New York-based non-profit EcoHealth Alliance. “These are pretty dangerous viruses from a lethality perspective, which don’t currently have the capacity to spread into broader human populations. But that can evolve, and you could very well see a variant emerge that has human-human transmission capability.”
That’s not an overstatement. Surveys suggest that mammals harbour about 40,000 viruses, with roughly a quarter capable of infecting humans. The vast majority never get a chance to do so because we don’t encounter them, but climate change can alter that. Recent studies have found that as animals relocate to new habitats due to shifting environmental conditions, the coming decades will bring around 300,000 first encounters between species which normally don’t interact, especially in tropical Africa and southeast Asia. All these interactions will make it far more likely for hitherto unknown viruses to cross paths with humans.
That’s why for the last 16 years, EcoHealth Alliance has been conducting ongoing viral surveillance projects across Bangladesh. The goal is to understand why Nipah is so much more prevalent in the western part of the country, compared to the east, and keep a watchful eye out for new Nipah strains as well as other dangerous pathogens like Ebola.
"There are a lot of different infectious agents that are sensitive to climate change that don't have these sorts of software tools being developed for them," says Cat Lippi, medical geography researcher at the University of Florida.
Until very recently this kind of work has been hampered by the limitations of viral surveillance technology. The PREDICT project, a $200 million initiative funded by the United States Agency for International Development, which conducted surveillance across the Amazon Basin, Congo Basin and extensive parts of South and Southeast Asia, relied upon so-called nucleic acid assays which enabled scientists to search for the genetic material of viruses in animal samples.
However, the project came under criticism for being highly inefficient. “That approach requires a big sampling effort, because of the rarity of individual infections,” says Ross. “Any particular animal may be infected for a couple of weeks, maybe once or twice in its lifetime. So if you sample thousands and thousands of animals, you'll eventually get one that has an Ebola virus infection right now.”
Ross explains that there is now far more interest in serological sampling—the scientific term for the process of drawing blood for antibody testing. By searching for the presence of antibodies in the blood of humans and animals, scientists have a greater chance of detecting viruses which started circulating recently.
Despite the controversy surrounding EcoHealth Alliance’s involvement in so-called gain of function research—experiments that study whether viruses might mutate into deadlier strains—the organization’s separate efforts to stay one step ahead of pathogen evolution are key to stopping the next pandemic.
“Having really cheap and fast surveillance is really important,” says Ross. “Particularly in a place where there's persistent, low level, moderate infections that potentially have the ability to develop into more epidemic or pandemic situations. It means there’s a pathway that something more dangerous can come through."

Scientists are searching for the presence of antibodies in the blood of humans and animals in hopes to detect viruses that recently started circulating.
EcoHealth Alliance
In Bangladesh, EcoHealth Alliance is attempting to do this using a newer serological technology known as a multiplex Luminex assay, which tests samples against a panel of known antibodies against many different viruses. It collects what Ross describes as a ‘footprint of information,’ which allows scientists to tell whether the sample contains the presence of a known pathogen or something completely different and needs to be investigated further.
By using this technology to sample human and animal populations across the country, they hope to gain an idea of whether there are any novel Nipah virus variants or strains from the same family, as well as other deadly viral families like Ebola.
This is just one of several novel tools being used for viral discovery in surveillance projects around the globe. Multiple research groups are taking PREDICT’s approach of looking for novel viruses in animals in various hotspots. They collect environmental DNA—mucus, faeces or shed skin left behind in soil, sediment or water—which can then be genetically sequenced.
Five years ago, this would have been a painstaking work requiring bringing collected samples back to labs. Today, thanks to the vast amounts of money spent on new technologies during COVID-19, researchers now have portable sequencing tools they can take out into the field.
Christopher Jerde, a researcher at the UC Santa Barbara Marine Science Institute, points to the Oxford Nanopore MinION sequencer as one example. “I tried one of the early versions of it four years ago, and it was miserable,” he says. “But they’ve really improved, and what we’re going to be able to do in the next five to ten years will be amazing. Instead of having to carefully transport samples back to the lab, we're going to have cigar box-shaped sequencers that we take into the field, plug into a laptop, and do the whole sequencing of an organism.”
In the past, viral surveillance has had to be very targeted and focused on known families of viruses, potentially missing new, previously unknown zoonotic pathogens. Jerde says that the rise of portable sequencers will lead to what he describes as “true surveillance.”
“Before, this was just too complex,” he says. “It had to be very focused, for example, looking for SARS-type viruses. Now we’re able to say, ‘Tell us all the viruses that are here?’ And this will give us true surveillance – we’ll be able to see the diversity of all the pathogens which are in these spots and have an understanding of which ones are coming into the population and causing damage.”
But being able to discover more viruses also comes with certain challenges. Some scientists fear that the speed of viral discovery will soon outpace the human capacity to analyze them all and assess the threat that they pose to us.
“I think we're already there,” says Jason Ladner, assistant professor at Northern Arizona University’s Pathogen and Microbiome Institute. “If you look at all the papers on the expanding RNA virus sphere, there are all of these deposited partial or complete viral sequences in groups that we just don't know anything really about yet.” Bats, for example, carry a myriad of viruses, whose ability to infect human cells we understand very poorly.
Cultivating these viruses under laboratory conditions and testing them on organoids— miniature, simplified versions of organs created from stem cells—can help with these assessments, but it is a slow and painstaking work. One hope is that in the future, machine learning could help automate this process. The new SpillOver Viral Risk Ranking platform aims to assess the risk level of a given virus based on 31 different metrics, while other computer models have tried to do the same based on the similarity of a virus’s genomic sequence to known zoonotic threats.
However, Ladner says that these types of comparisons are still overly simplistic. For one thing, scientists are still only aware of a few hundred zoonotic viruses, which is a very limited data sample for accurately assessing a novel pathogen. Instead, he says that there is a need for virologists to develop models which can determine viral compatibility with human cells, based on genomic data.
“One thing which is really useful, but can be challenging to do, is understand the cell surface receptors that a given virus might use,” he says. “Understanding whether a virus is likely to be able to use proteins on the surface of human cells to gain entry can be very informative.”
As the Earth’s climate heats up, scientists also need to better model the so-called vector borne diseases such as dengue, Zika, chikungunya and yellow fever. Transmitted by the Aedes mosquito residing in humid climates, these blights currently disproportionally affect people in low-income nations. But predictions suggest that as the planet warms and the pests find new homes, an estimated one billion people who currently don’t encounter them might be threatened by their bites by 2080. “When it comes to mosquito-borne diseases we have to worry about shifts in suitable habitat,” says Cat Lippi, a medical geography researcher at the University of Florida. “As climate patterns change on these big scales, we expect to see shifts in where people will be at risk for contracting these diseases.”
Public health practitioners and government decision-makers need tools to make climate-informed decisions about the evolving threat of different infectious diseases. Some projects are already underway. An ongoing collaboration between the Catalan Institution for Research and Advanced Studies and researchers in Brazil and Peru is utilizing drones and weather stations to collect data on how mosquitoes change their breeding patterns in response to climate shifts. This information will then be fed into computer algorithms to predict the impact of mosquito-borne illnesses on different regions.

The team at the Catalan Institution for Research and Advanced Studies is using drones and weather stations to collect data on how mosquito breeding patterns change due to climate shifts.
Gabriel Carrasco
Lippi says that similar models are urgently needed to predict how changing climate patterns affect respiratory, foodborne, waterborne and soilborne illnesses. The UK-based Wellcome Trust has allocated significant assets to fund such projects, which should allow scientists to monitor the impact of climate on a much broader range of infections. “There are a lot of different infectious agents that are sensitive to climate change that don't have these sorts of software tools being developed for them,” she says.
COVID-19’s havoc boosted funding for infectious disease research, but as its threats begin to fade from policymakers’ focus, the money may dry up. Meanwhile, scientists warn that another major infectious disease outbreak is inevitable, potentially within the next decade, so combing the planet for pathogens is vital. “Surveillance is ultimately a really boring thing that a lot of people don't want to put money into, until we have a wide scale pandemic,” Jerde says, but that vigilance is key to thwarting the next deadly horror. “It takes a lot of patience and perseverance to keep looking.”
This article originally appeared in One Health/One Planet, a single-issue magazine that explores how climate change and other environmental shifts are increasing vulnerabilities to infectious diseases by land and by sea. The magazine probes how scientists are making progress with leaders in other fields toward solutions that embrace diverse perspectives and the interconnectedness of all lifeforms and the planet.
Vanessa Colimorio (left) and Sharon Kochlany (right) at a farm with their four-year-old twin daughters and one-year-old son. The kids share the same sperm donor.
Sharon Kochlany and Vanessa Colimorio's four-year-old twin girls had a classic school assignment recently: make a family tree. They drew themselves and their one-year-old brother branching off from their moms, with aunts, uncles, and grandparents forking off to the sides.
The recently-gained sovereignty of queer families stands to be lost if a consumer DNA test brings a stranger's identity out of the woodwork.
What you don't see in the invisible space between Kochlany and Colimorio, however, is the sperm donor they used to conceive all three children.
To look at a family tree like this is to see in its purest form that kinship can supersede biology—the boundaries of where this family starts and stops are clear to everyone in it, in spite of a third party's genetic involvement. This kind of self-definition has always been synonymous with LGBTQ families, especially those that rely on donor gametes (sperm or eggs) to exist.
But the world around them has changed quite suddenly: The recent consumer DNA testing boom has made it more complicated than ever for families built through reproductive technology—openly, not secretively—to maintain the strong sense of autonomy and privacy that can be crucial for their emotional security. Prospective parents and cryobanks are now mulling how best to bring a new generation of donor-conceived people into this world in a way that leaves open the choice to know more about their ancestry without obliterating an equally important choice: the right not to know about biological relatives.
For queer parents who have long fought for social acceptance, having a biological relationship to their children has been revolutionary, and using an unknown donor as a means to this end especially so. Getting help from a friend often comes with the expectation that the friend will also have social involvement in the family, which some people are comfortable with, but being able to access sperm from an unknown donor—which queer parents have only been able to openly do since the early 1980s—grants them the reproductive autonomy to create families seemingly on their own. That recently-gained sovereignty stands to be lost if a consumer DNA test brings a stranger's identity out of the woodwork.
At the same time, it's natural for donor-conceived people to want to know more about where they come from ethnically, even if they don't want to know the identity of their donor. As a donor-conceived person myself, I know my donor's self-reported ethnicity, but have often wondered how accurate it is.
Opening the Pandora's box of a consumer DNA test as a way to find out has always felt profoundly unappealing to me, however. Many people have accidentally learned they're donor-conceived by unwittingly using these tools, but I already know that about myself going in, and subsequently know I'll be connected to a large web of people whose existence I'm not interested in learning about. In addition to possibly identifying my anonymous donor, his family could also show up, along with any donor-siblings—other people with whom I share a donor. My single lesbian mom is enough for me, and the trade off to learn more about my ethnic ancestry has never seemed worth it.
In 1992, when I was born, no one was planning for how consumer DNA tests might upend or illuminate one's sense of self. But the donor community has always had to stay nimble with balancing privacy concerns and psychological well-being, so it should come as no surprise that figuring out how to do so in 2020 includes finding a way to offer ancestry insight while circumventing consumer DNA tests.
A New Paradigm
This is the rationale behind unprecedented industry news that LeapsMag can exclusively break: Within the next few weeks, California Cryobank, the largest cryobank in the country, will begin offering genetically-verified ancestry information on the free public part of every donor's anonymous profile in its database, something no other cryobanks yet offer (an exact launch date was not available at the time of publication). Currently, California Cryobank's donor profiles include a short self-reported list that might merely say, "Ancestry: German, Lebanese, Scottish."
The new information will be a report in pie chart form that details exactly what percentages of a donor's DNA come from up to 26 ethnicities—it's analogous to, but on a smaller scale than, the format offered by consumer DNA testing companies, and uses the same base technology that looks for single nucleotide polymorphisms in DNA that are associated with specific ethnicities. But crucially, because the donor takes the DNA test through California Cryobank, not a consumer-facing service, the information is not connected in a network to anyone else's DNA test. It's also taken before any offspring exist so there's no chance of revealing a donor-conceived person's identity this way.
Later, when a donor-conceived person is born, grows up, and wants information about their ethnicity from the donor side, all they need is their donor's anonymous ID number to look it up. The donor-conceived person never takes a genetic test, and therefore also can't accidentally find donor siblings this way. People who want to be connected to donor siblings can use a sibling registry where other people who want to be found share donor ID numbers and look for matches (this is something that's been available for decades, and remains so).
"With genetic testing, you have no control over who reaches out to you, and at what point in your life."
California Cryobank will require all new donors to consent to this extra level of genetic testing, setting a new standard for what information prospective parents and donor-conceived people can expect to have. In the immediate, this information will be most useful for prospective parents looking for donors with specific backgrounds, possibly ones similar to their own.
It's a solution that was actually hiding in plain sight. Two years ago, California Cryobank's partner Sema4, the company handling the genetic carrier testing that's used to screen for heritable diseases, started analyzing ethnic data in its samples. That extra information was being collected because it can help calculate a more accurate assessment of genetic risks that run in certain populations—like Ashkenazi Jews and Tay Sachs disease—than relying on oral family histories. Shortly after a plan to start collecting these extra data, Jamie Shamonki, chief medical officer of California Cryobank, realized the companies would be sitting on a goldmine for a different reason.
"I didn't want to use one of these genetic testing companies like Ancestry to accomplish this," says Shamonki. "The whole thing we're trying to accomplish is also privacy."
Consumer-facing DNA testing companies are not HIPAA compliant (whereas Sema4, which isn't direct-to-consumer, is HIPAA compliant), which means there are no legal privacy protections covering people who add their DNA to these databases. Although some companies, like 23andMe, allow users to opt-out of being connected with genetic relatives, the language can be confusing to navigate, requires a high level of knowledge and self-advocacy on the user's part, and, as an opt-out system, is not set up to protect the user from unwanted information by default; many unwittingly walk right into such information as a result.
Additionally, because consumer-facing DNA testing companies operate outside the legal purview that applies to other health care entities, like hospitals, even a person who does opt-out of being linked to genetic relatives is not protected in perpetuity from being re-identified in the future by a change in company policy. The safest option for people with privacy concerns is to stay out of these databases altogether.
For California Cryobank, the new information about donor heritage won't retroactively be added to older profiles in the system, so donor-conceived people who already exist won't benefit from the ancestry tool, but it'll be the new standard going forward. The company has about 500 available donors right now, many of which have been in their registry for a while; about 100 of those donors, all new, will have this ancestry data on their profiles.
Shamonki says it has taken about two years to get to the point of publicly including ancestry information on a donor's profile because it takes about nine months of medical and psychological screening for a donor to go from walking through the door to being added to their registry. The company wanted to wait to launch until it could offer this information for a significant number of donors. As more new donors come online under the new protocol, the number with ancestry information on their profiles will go up.
For Parents: An Unexpected Complication
While this change will no doubt be welcome progress for LGBTQ families contemplating parenthood, it'll never be possible to put this entire new order back in the box. What are such families who already have donor-conceived children losing in today's world of widespread consumer genetic testing?
Kochlany and Colimorio's twins aren't themselves much older than the moment at-home DNA testing really started to take off. They were born in 2015, and two years later the industry saw its most significant spike. By now, more than 26 million people's DNA is in databases like 23andMe and Ancestry; as a result, it's estimated that within a year, 90 percent of Americans of European descent will be identifiable through these consumer databases, by way of genetic third cousins, even if they didn't want to be found and never took the test themselves. This was the principle behind solving the Golden State Killer cold case.
The waning of privacy through consumer DNA testing fundamentally clashes with the priorities of the cyrobank industry, which has long sought to protect the privacy of donor-conceived people, even as open identification became standard. Since the 1980s, donors have been able to allow their identity to be released to any offspring who is at least 18 and wants the information. Lesbian moms pushed for this option early on so their children—who would obviously know they couldn't possibly be the biological product of both parents—would never feel cut off from the chance to know more about themselves. But importantly, the openness is not a two-way street: the donors can't ever ask for the identities of their offspring. It's the latter that consumer DNA testing really puts at stake.
"23andMe basically created the possibility that there will be donors who will have contact with their donor-conceived children, and that's not something that I think the donor community is comfortable with," says I. Glenn Cohen, director of Harvard Law School's Center for Health Law Policy, Biotechnology & Bioethics. "That's about the donor's autonomy, not the rearing parents' autonomy, or the donor-conceived child's autonomy."
Kochlany and Colimorio have an open identification donor and fully support their children reaching out to California Cryobank to get more information about him if they want to when they're 18, but having a singular name revealed isn't the same thing as having contact, nor is it the same thing as revealing a web of dozens of extended genetic relations. Their concern now is that if their kids participate in genetic testing, a stranger—someone they're careful to refer to as only "the donor" and never "dad"—will reach out to the children to begin some kind of relationship. They know other people who are contemplating giving their children DNA tests, and feel staunchly that it wouldn't be right for their family.
"With genetic testing, you have no control over who reaches out to you, and at what point in your life," Kochlany says. "[People] reaching out and trying to say, 'Hey I know who your dad is' throws a curveball. It's like, 'Wait, I never thought I had a dad.' It might put insecurities in their minds."
"We want them to have the opportunity to choose whether or not they want to reach out," Colimorio adds.
Kochlany says that when their twins are old enough to start asking questions, she and Colimorio plan to frame it like this: "The donor was kind of like a technology that helped us make you a person, and make sure that you exist," she says, role playing a conversation with their kids. "But it's not necessarily that you're looking to this person [for] support or love, or because you're missing a piece."
It's a line in the sand that's present even for couples still far off from conceiving. When Mallory Schwartz, a film and TV producer in Los Angeles, and Lauren Pietra, a marriage and family therapy associate (and Shamonki's step-daughter), talk about getting married someday, it's a package deal with talking about how they'll approach having kids. They feel there are too many variables and choices to make around family planning as a same-sex couple these days to not have those conversations simultaneously. Consumer DNA databases are already on their minds.
"It frustrates me that the DNA databases are just totally unregulated," says Schwartz. "I hope they are by the time we do this. I think everyone deserves a right to privacy when making your family [using a sperm donor]."
"I wouldn't want to create a world where people who are donor-conceived feel like they can't participate in this technology because they're trying to shut out [other] information."
On the prospect of having a donor relation pop up non-consensually for a future child, Pietra says, "I don't like it. It would be really disappointing if the child didn't want [contact], and unfortunately they're on the receiving end."
You can see how important preserving the right to keep this door closed is when you look at what's going on at The Sperm Bank of California. This pioneering cryobank was the first in the world to openly serve LGBTQ people and single women, and also the first to offer the open identification option when it opened in 1982, but not as many people are asking for their donor's identity as expected.
"We're finding a third of young people are coming forward for their donor's identity," says Alice Ruby, executive director. "We thought it would be a higher number." Viewed the other way, two-thirds of the donor-conceived people who could ethically get their donor's identity through The Sperm Bank of California are not asking the cryobank for it.
Ruby says that part of what historically made an open identification program appealing, rather than invasive or nerve-wracking, is how rigidly it's always been formatted around mutual consent, and protects against surprises for all parties. Those [donor-conceived people] who wanted more information were never barred from it, while those who wanted to remain in the dark could. No one group's wish eclipsed the other's. The potential breakdown of a system built around consent, expectations, and respect for privacy is why unregulated consumer DNA testing is most concerning to her as a path for connecting with genetic relatives.
For the last few decades in cryobanks around the world, the largest cohort of people seeking out donor sperm has been lesbian couples, followed by single women. For infertile heterosexual couples, the smallest client demographic, Ruby says donor sperm offers a solution to a medical problem, but in contrast, it historically "provided the ability for [lesbian] couples and single moms to have some reproductive autonomy." Yes, it was still a solution to a biological problem, but it was also a solution to a social one.
The Sperm Bank of California updated its registration forms to include language urging parents, donor-conceived people, and donors not to use consumer DNA tests, and to go through the cryobank if they, understandably, want to learn more about who they're connected to. But truthfully, there's not much else cryobanks can do to protect clients on any side of the donor transaction from surprise contact right now—especially not from relatives of the donor who may not even know someone in their family has donated sperm.
A Tricky Position
Personally, I've known I was donor-conceived from day one. It has never been a source of confusion, angst, or curiosity, and in fact has never loomed particularly large for me in any way. I see it merely as a type of reproductive technology—on par with in vitro fertilization—that enabled me to exist, and, now that I do exist, is irrelevant. Being confronted with my donor's identity or any donor siblings would make this fact of my conception bigger than I need it to be, as an adult with a full-blown identity derived from all of my other life experiences. But I still wonder about the minutiae of my ethnicity in much the same way as anyone else who wonders, and feel there's no safe way for me to find out without relinquishing some of my existential independence.
"People obviously want to participate in 23andMe and Ancestry because they're interested in knowing more about themselves," says Shamonki. "I wouldn't want to create a world where people who are donor-conceived feel like they can't participate in this technology because they're trying to shut out [other] information."
After all, it was the allure of that exact conceit—knowing more about oneself—that seemed to magnetically draw in millions of people to these tools in the first place. It's an experience that clearly taps into a population-wide psychic need, even—perhaps especially—if one's origins are a mystery.
As We Wait for a Vaccine, Scientists Work to Scale Up the Best COVID-19 Antibodies to Give New Patients
In this illustration of immune defense, Y-shaped proteins called antibodies attack a virus.
When we get sick, our immune system sends its soldier cells to the battlefield. Called B-cells, they "examine" the foreign particles that shouldn't be in our bloodstream—and start producing the antibodies, the proteins to neutralize the invaders.
To screen the antibodies, scientists have developed a proprietary way to make the effective ones glow – like a literal "lightbulb" moment.
The better these antibodies are at neutralizing the pathogen, the faster we recover.
The antibodies acquired from COVID-19 survivors already showed promise in treating other patients, but because they must be obtained from people, generating a regular supply is not feasible. To close the gap, researchers are trying to identify the B-cells that make the best antibodies—and then farm them in laboratories at scale.
Scientists at Berkley Lights, a biotechnology company in California, have been screening B-cells from recovered patients and testing the antibodies they release for virus-neutralizing abilities. To screen the antibodies, scientists there have developed a proprietary way to make the effective ones glow – like a literal "lightbulb" moment.
So how does it work? First, the individual B-cells are placed into microscopic chambers called nano-pens, where they secrete the antibodies. Once released, the antibodies are flushed over tiny beads that have bits of the viral particles attached to them, along with special molecules that can emit fluorescent light.
"When an antibody binds to the bead, we see a bright light on the bead," explains John Proctor, the company's senior vice president of antibody therapeutics. "So we can identify which cells are making the antibodies."
Then the antibodies are tested for their ability to counteract the coronavirus's spike proteins, which the virus uses to break into our cells. Not all antibodies are equally good at this crucial defense move—some can block only parts of the virus's machinery, while others can neutralize it completely. Proctor and his colleagues are looking for the latter.
Once scientists identify the best performing B-cells, they crack the cells open—or in scientific terms "lyse" them—and extract the genetic instructions for making the antibodies. As it turns out, B-cells aren't very efficient at pumping out massive amounts of antibodies, so scientists insert these genetic instructions into a different, more prolific type of cell.
Named Chinese Hamster Ovary Cells or CHO, these cells are commonly used in the pharmaceutical industry because they can generate therapeutic proteins en masse. Under the right nutrient conditions, which include a lot of sugar, CHO cells can keep making the antibodies at commercial levels. "They are engineered to operate in very large bioreactors," Proctor explains.
While traditional antibody screening can take three months, the Beacon System can do it in less than 24 hours.
Berkeley Lights' technology has already been used to screen the antibodies of recovered patients from Vanderbilt University Medical Center. In another example, a biotech company GenScript ProBio used the platform to screen mice engineered to have human antibodies for the coronavirus.
In addition to its small, lab-on-a-chip size, Berkeley Lights' system allows scientists to greatly speed up the screening process. While traditional antibody screening can take three months, the Beacon System can do it in less than 24 hours. "We only need one B-cell per pen and a couple of beads to see that fluorescent signal," Proctor says. "It is a more advanced way to process and analyze cells, and that level of sensitivity is unique to our technology."
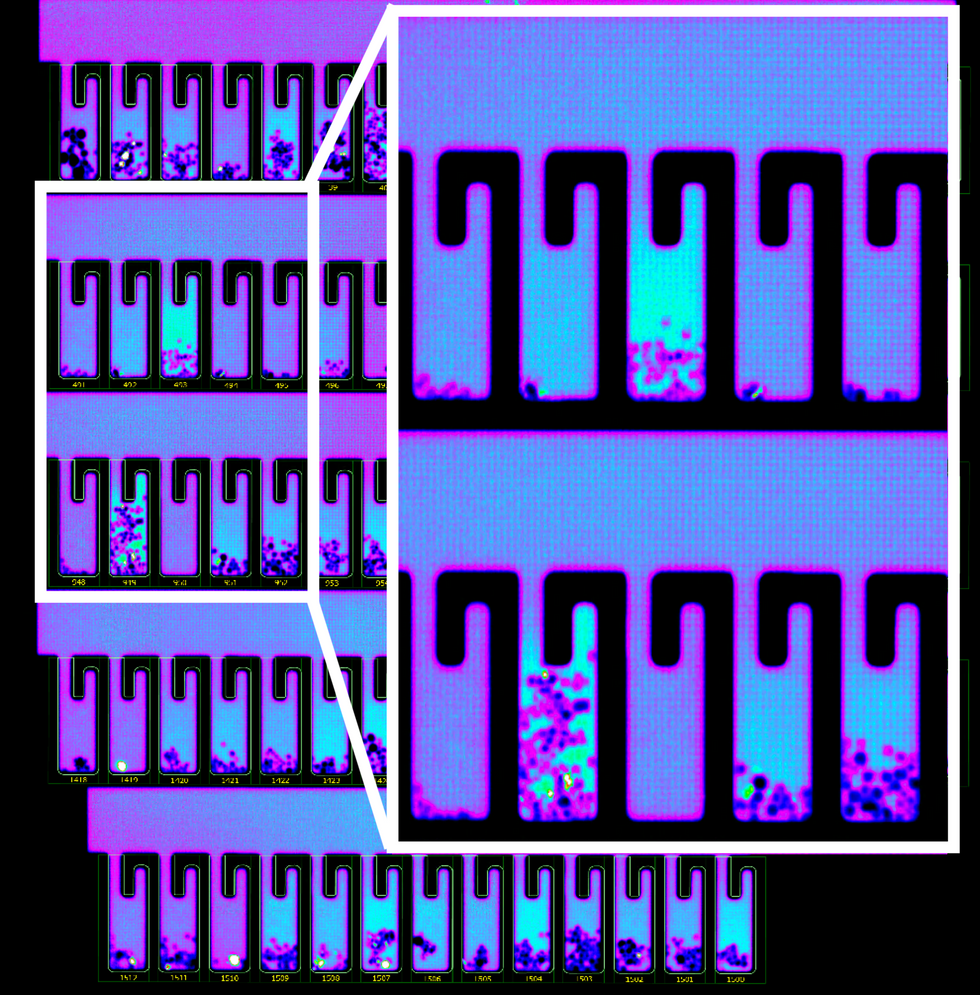
B-cells secreting antibodies inside the Berkeley Lights Beacon System Nano-Pens.
While vaccines are likely to take months to develop and test, antibodies might arrive to the battleground sooner. With the extremely limited treatment options for COVID-19, antibody-based therapeutics can potentially bridge this gap.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.