Is Carbon Dioxide the New Black? Yes, If These Fabric-Designing Scientists Have Their Way

The entrepreneurs Tawfiq Nasr Allah (left, standing) and Benoit Illy (right, sitting down) at Fairbrics' lab in Clichy, France.
Each year the world releases around 33 billion tons of carbon dioxide into the atmosphere. What if we could use this waste carbon dioxide to make shirts, dresses and hats? It sounds unbelievable. But two innovators are trying to tackle climate change in this truly unique way.
Chemist Tawfiq Nasr Allah set up Fairbrics with material scientist Benoît Illy in 2019. They're using waste carbon dioxide from industrial fumes as a raw material to create polyester, identical to the everyday polyester we use now. They want to take a new and very different approach to make the fashion industry more sustainable.
The Dark Side of Fast Fashion
The fashion industry is responsible for around 4% of global emissions. In a 2015 report, the MIT Materials Systems Laboratory predicted that the global impact of polyester fabric will grow from around 880 billion kg of CO2 in 2015 to 1.5 trillion kg of CO2 by 2030.
Professor Greg Peters, an expert in environmental science and sustainability, highlights the wide-ranging difficulties caused by the production of polyester. "Because it is made from petrochemical crude oil there is no real limit on how much polyester can be produced...You have to consider the ecological damage (oil spills, fracking etc.) caused by the oil and gas industry."
Many big-name brands have pledged to become carbon neutral by 2050. But nothing has really changed in the way polyester is produced.
Some companies are recycling plastic bottles into polyester. The plastic is melted into ultra-fine strands and then spun to create polyester. However, only a limited number of bottles are available. New materials must be added because of the amount of plastic degradation that takes place. Ultimately, recycling accounts for only a small percentage of the total amount of polyester produced.
Nasr Allah and Illy hope they can offer the solution the fashion industry is looking for. They are not just reducing the carbon emissions that are conventionally produced by making polyester. Their process actually goes much further. It's carbon negative and works by using up emissions from other industries.
"In a sense we imitate what nature does so well: plants capture CO2 and turn it into natural fibers using sunlight, we capture CO2 and turn it into synthetic fibers using electricity."
Experts in the field see a lot of promise. Dr Phil de Luna is an expert in carbon valorization -- the process of converting carbon dioxide into high-value chemicals. He leads a $57-million research program developing the technology to decarbonize Canada.
"I think the approach is great," he says. "Being able to take CO2 and then convert it into polymers or polyester is an excellent way to think about utilizing waste emissions and replacing fossil fuel-based materials. That is overall a net negative as compared to making polyester from fossil fuels."
From Harmful Waste to Useful Raw Material
It all started with Nasr Allah's academic research, primarily at the French Alternative Energies and Atomic Energy Commission (CEA). He spent almost 5 years investigating CO2 valorization. In essence, this involves breaking the bonds between the carbon and oxygen atoms in CO2 to create bonds with other elements.
Recycling carbon dioxide in this way requires extremely high temperatures and pressures. Catalysts are needed to break the strong bonds between the atoms. However, these are toxic, volatile and quickly lose their effectiveness over time. So, directly converting carbon dioxide into the raw material for making polyester fibers is very difficult.
Nasr Allah developed a process involving multiple simpler stages. His innovative approach involves converting carbon dioxide to intermediate chemicals. These chemicals can then be transformed into the raw material which is used in the production of polyester. After many experiments, Nasr Allah developed new processes and new catalysts that worked more effectively.
"We use a catalyst to transform CO2 into the chemicals that are used for polyester manufacturing," Illy says. "In a sense we imitate what nature does so well: plants capture CO2 and turn it into natural fibers using sunlight, we capture CO2 and turn it into synthetic fibers using electricity."
The Challenges Ahead
Nasr Allah met material scientist Illy through Entrepreneur First, a programme which pairs individuals looking to form technical start-ups. Together they set up Fairbrics and worked on converting Nasr Allah's lab findings into commercial applications and industrial success.
"The main challenge we faced was to scale up the process," Illy reveals. "[It had to be] consistent and safe to be carried out by a trained technician, not a specialist PhD as was the case in the beginning."
They recruited a team of scientists to help them develop a more effective and robust manufacturing process. Together, the team gained a more detailed theoretical understanding about what was happening at each stage of the chemical reactions. Eventually, they were able to fine tune the process and produce consistent batches of polyester.
They're making significant progress. They've produced their first samples and signed their first commercial contract to make polyester, which will then be both fabricated into clothes and sold by partner companies.
Currently, one of the largest challenges is financial. "We need to raise a fair amount to buy the equipment we need to produce at a large scale," Illy explains.
How to Power the Process?
At the moment, their main scientific focus is getting the process working reliably so they can begin commercialization. In order to remain sustainable and economically viable once they start producing polyester on a large scale, they need to consider the amount of energy they use for carbon valorization and the emissions they produce.
The more they optimize the way their catalyst works, the easier it will be to transform the CO2. The whole process can then become more cost effective and energy efficient.
De Luna explains: "My concern is...whether their process will be economical at scale. The problem is the energy cost to take carbon dioxide and transform it into these other products and that's where the science and innovation has to happen. [Whether they can scale up economically] depends on the performance of their catalyst."
They don't just need to think about the amount of energy they use to produce polyester; they also have to consider where this energy comes from.
"They need access to cheap renewable energy," De Luna says, "...so they're not using or emitting CO2 to do the conversion." If the energy they use to transform CO2 into polyester actually ends up producing more CO2, this will end up cancelling out their positive environmental impact.
Based in France, they're well located to address this issue. France has a clean electricity system, with only about 10% of their electric power coming from fossil fuels due to their reliance on nuclear energy and renewables.
Where Do They Get the Carbon Dioxide?
As they scale up, they also need to be able to access a source of CO2. They intend to obtain this from the steel industry, the cement industry, and hydrogen production.
The technology to purify and capture waste carbon dioxide from these industries is available on a large scale. However, there are only around 20 commercial operations in the world. The high cost of carbon capture means that development continues to be slow. There are a growing number of startups capturing carbon dioxide straight from the air, but this is even more costly.
One major problem is that storing captured carbon dioxide is expensive. "There are somewhat limited options for permanently storing captured CO2, so innovations like this are important,'' says T. Reed Miller, a researcher at the Yale University Center for Industrial Ecology.
Illy says: "The challenge is now to decrease the cost [of carbon capture]. By using CO2 as a raw material, we can try to increase the number of industries that capture CO2. Our goal is to turn CO2 from a waste into a valuable product."
Beyond Fashion
For Nasr Allah and Illy, fashion is just the beginning. There are many markets they can potentially break into. Next, they hope to use the polyester they've created in the packaging industry. Today, a lot of polyester is consumed to make bottles and jars. Illy believes that eventually they can produce many different chemicals from CO2. These chemicals could then be used to make paints, adhesives, and even plastics.
The Fairbrics scientists are providing a vital alternative to fossil fuels and showcasing the real potential of carbon dioxide to become a worthy resource instead of a harmful polluter.
Illy believes they can make a real difference through innovation: "We can have a significant impact in reducing climate change."
Kirstie Ennis, an Afghanistan veteran who survived a helicopter crash but lost a limb, pictured in May 2021 at Two Rivers Park in Colorado.
In June 2012, Kirstie Ennis was six months into her second deployment to Afghanistan and recently promoted to sergeant. The helicopter gunner and seven others were three hours into a routine mission of combat resupplies and troop transport when their CH-53D helicopter went down hard.
Miraculously, all eight people onboard survived, but Ennis' injuries were many and severe. She had a torn rotator cuff, torn labrum, crushed cervical discs, facial fractures, deep lacerations and traumatic brain injury. Despite a severely fractured ankle, doctors managed to save her foot, for a while at least.
In November 2015, after three years of constant pain and too many surgeries to count, Ennis relented. She elected to undergo a lower leg amputation but only after she completed the 1,000-mile, 72-day Walking with the Wounded journey across the UK.
On Veteran's Day of that year, on the other side of the country, orthopedic surgeon Cato Laurencin announced a moonshot challenge he was setting out to achieve on behalf of wounded warriors like Ennis: the Hartford Engineering A Limb (HEAL) Project.
Laurencin, who is a University of Connecticut professor of chemical, materials and biomedical engineering, teamed up with experts in tissue bioengineering and regenerative medicine from Harvard, Columbia, UC Irvine and SASTRA University in India. Laurencin and his colleagues at the Connecticut Convergence Institute for Translation in Regenerative Engineering made a bold commitment to regenerate an entire limb within 15 years – by the year 2030.
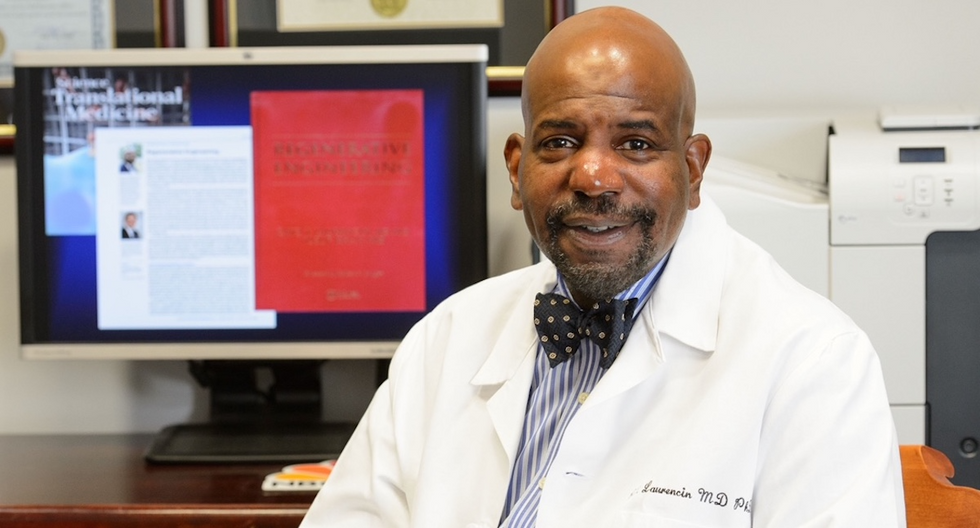
Dr. Cato Laurencin pictured in his office at UConn.
Photo Credit: UConn
Regenerative Engineering -- A Whole New Field
Limb regeneration in humans has been a medical and scientific fascination for decades, with little to show for the effort. However, Laurencin believes that if we are to reach the next level of 21st century medical advances, this puzzle must be solved.
An estimated 185,000 people undergo upper or lower limb amputation every year. Despite the significant advances in electromechanical prosthetics, these individuals still lack the ability to perform complex functions such as sensation for tactile input, normal gait and movement feedback. As far as Laurencin is concerned, the only clinical answer that makes sense is to regenerate a whole functional limb.
Laurencin feels other regeneration efforts were hampered by their siloed research methods with chemists, surgeons, engineers all working separately. Success, he argues, requires a paradigm shift to a trans-disciplinary approach that brings together cutting-edge technologies from disparate fields such as biology, material sciences, physical, chemical and engineering sciences.
As the only surgeon ever inducted into the academies of Science, Medicine and Innovation, Laurencin is uniquely suited for the challenge. He is regarded as the founder of Regenerative Engineering, defined as the convergence of advanced materials sciences, stem cell sciences, physics, developmental biology and clinical translation for the regeneration of complex tissues and organ systems.
But none of this is achievable without early clinician participation across scientific fields to develop new technologies and a deeper understanding of how to harness the body's innate regenerative capabilities. "When I perform a surgical procedure or something is torn or needs to be repaired, I count on the body being involved in regenerating tissue," he says. "So, understanding how the body works to regenerate itself and harnessing that ability is an important factor for the regeneration process."
The Birth of the Vision
Laurencin's passion for regeneration began when he was a sports medicine fellow at Cornell University Medical Center in the early 1990s. There he saw a significant number of injuries to the anterior cruciate ligament (ACL), the major ligament that stabilizes the knee. He believed he could develop a better way to address those injuries using biomaterials to regenerate the ligament. He sketched out a preliminary drawing on a napkin one night over dinner. He has spent the next 30 years regenerating tissues, including the patented L-C ligament.
As chair of Orthopaedic Surgery at the University of Virginia during the peak of the wars in Iraq and Afghanistan, Laurencin treated military personnel who survived because of improved helmets, body armor and battlefield medicine but were left with more devastating injuries, including traumatic brain injuries and limb loss.
"I was so honored to care for them and I so admired their steadfast courage that I became determined to do something big for them," says Laurencin.
When he tells people about his plans to regrow a limb, he gets a lot of eye rolls, which he finds amusing but not discouraging. Growing bone cells was relatively new when he was first focused on regenerating bone in 1987 at MIT; in 2007 he was well on his way to regenerating ligaments at UVA when many still doubted that ligaments could even be reconstructed. He and his team have already regenerated torn rotator cuff tendons and ACL ligaments using a nano-textured fabric seeded with stem cells.
Even as a finalist for the $4 million NIH Pioneer Award for high-risk/high-reward research, he faced a skeptical scientific audience in 2014. "They said, 'Well what do you plan to do?' I said 'I plan to regenerate a whole limb in people.' There was a lot of incredulousness. They stared at me and asked a lot of questions. About three days later, I received probably the best score I've ever gotten on an NIH grant."
In the Thick of the Science
Humans are born with regenerative abilities--two-year-olds have regrown fingertips--but lose that ability with age. Salamanders are the only vertebrates that can regenerate lost body parts as adults; axolotl, the rare Mexican salamander, can grow extra limbs.
The axolotl is important as a model organism because it is a four-footed vertebrate with a similar body plan to humans. Mapping the axolotl genome in 2018 enhanced scientists' genetic understanding of their evolution, development, and regeneration. Being easy to breed in captivity allowed the HEAL team to closely study these amphibians and discover a new cell type they believe may shed light on how to mimic the process in humans.
"Whenever limb regeneration takes place in the salamander, there is a huge amount of something called heparan sulfate around that area," explains Laurencin. "We thought, 'What if this heparan sulfate is the key ingredient to allowing regeneration to take place?' We found these groups of cells that were interspersed in tissues during the time of regeneration that seemed to have connections to each other that expressed this heparan sulfate."
Called GRID (Groups that are Regenerative, Interspersed and Dendritic), these cells were also recently discovered in mice. While GRID cells don't regenerate as well in mice as in salamanders, finding them in mammals was significant.
"If they're found in mice. we might be able to find these in humans in some form," Laurencin says. "We think maybe it will help us figure out regeneration or we can create cells that mimic what grid cells do and create an artificial grid cell."
What Comes Next?
Laurencin and his team have individually engineered and made every single tissue in the lower limb, including bone, cartilage, ligament, skin, nerve, blood vessels. Regenerating joints and joint tissue is the next big mile marker, which Laurencin sees as essential to regenerating a limb that functions and performs in the way he envisions.
"Using stem cells and amnion tissue, we can regenerate joints that are damaged, and have severe arthritis," he says. "We're making progress on all fronts, and making discoveries we believe are going to be helping people along the way."
That focus and advancement is vital to Ennis. After laboring over the decision to have her leg amputated below the knee, she contracted MRSA two weeks post-surgery. In less than a month, she went from a below-the-knee-amputee to a through-the-knee amputee to an above-the-knee amputee.
"A below-the-knee amputation is night-and-day from above-the-knee," she said. "You have to relearn everything. You're basically a toddler."

Kirstie Ennis pictured in July 2020.
Photo Credit: Ennis' Instagram
The clock is ticking on the timeline Laurencin set for himself. Nine years might seem like forever if you're doing time but it might appear fleeting when you're trying to create something that's never been done before. But Laurencin isn't worried. He's convinced time is on his side.
"Every week, I receive an email or a call from someone, maybe a mother whose child has lost a finger or I'm in communication with a disabled American veteran who wants to know how the progress is going. That energizes me to continue to work hard to try to create these sorts of solutions because we're talking about people and their lives."
He devotes about 60 hours a week to the project and the roughly 100 students, faculty and staff who make up the HEAL team at the Convergence Institute seem acutely aware of what's at stake and appear equally dedicated.
"We're in the thick of the science in terms of making this happen," says Laurencin. "We've moved from making the impossible possible to making the possible a reality. That's what science is all about."
7 Reasons Why We Should Not Need Boosters for COVID-19
A top infectious disease physician explains why immunity derived from natural infection and the vaccines should be long-lasting.
There are at least 7 reasons why immunity after vaccination or infection with COVID-19 should likely be long-lived. If durable, I do not think boosters will be necessary in the future, despite CEOs of pharmaceutical companies (who stand to profit from boosters) messaging that they may and readying such boosters. To explain these reasons, let's orient ourselves to the main components of the immune system.
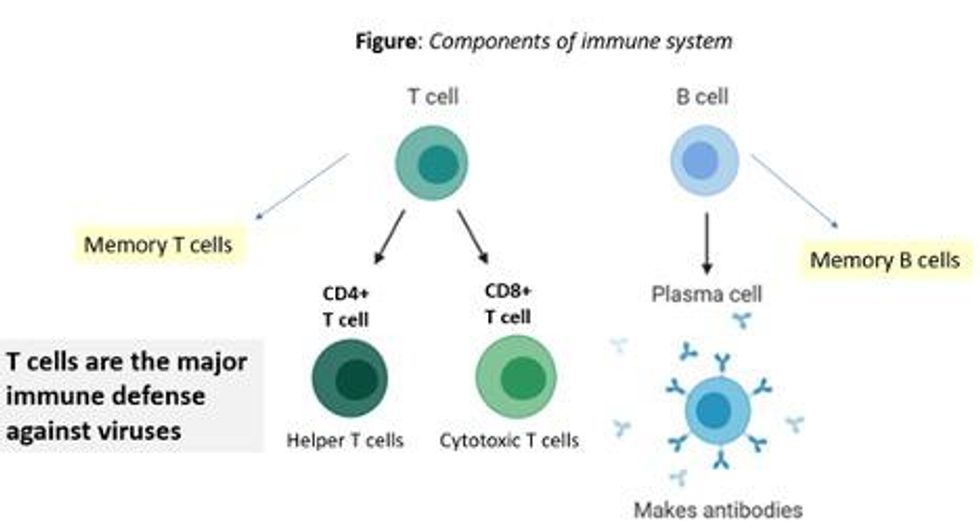
There are two major arms of the immune system: B cells (which produce antibodies) and T cells (which are formed specifically to attack and kill pathogens). T cells are divided into two types, CD4 cells ("helper" T cells) and CD8 cells ("cytotoxic" T cells).
Each arm, once stimulated by infection or vaccine, should hopefully make "memory" banks. So if the body sees the pathogen in the future, these defenses should come roaring back to attack the virus and protect you from getting sick. Plenty of research in COVID-19 indicates a likely long-lasting response to the vaccine or infection. Here are seven of the most compelling reasons:
REASON 1: Memory B Cells Are Produced By Vaccines and Natural Infection
In one study, 12 volunteers who had never had Covid-19--and were fully vaccinated with two Pfizer/BioNTech shots-- underwent biopsies of their lymph nodes. This is where memory B cells are stored in places called "germinal centers". The biopsies were performed three, four, six, and seven weeks after the first mRNA vaccine shot, and were stained to reveal that germinal center memory B cells in the lymph nodes increased in concentration over time.
Natural infection also generates memory B cells. Even after antibody levels wane over time, strong memory B cells were detected in the blood of individuals six and eight months after infection in different studies. Indeed, the half-lives of the memory B cells seen in the study examining patients 8 months after COVID-19 led the authors to conclude that "B cell memory to SARS-CoV-2 was robust and is likely long-lasting." Reason #2 tells us that memory B cells can be active for a very long time indeed.
REASON #2: Memory B Cells Can Produce Neutralizing Antibodies If They See Infection Again Decades Later
Demonstrated production of memory B cells after vaccination or natural infection with COVID-19 is so important because memory B cells, once generated, can be activated to produce high levels of neutralizing antibodies against the pathogen even if encountered many years after the initial exposure. In one amazing study (published in 2008), researchers isolated memory B cells against the 1918 flu strain from the blood of 32 individuals aged 91-101 years. These people had been born on or before 1915 and had survived that pandemic.
Their memory B cells, when exposed to the 1918 flu strain in a test tube, generated high levels of neutralizing antibodies against the virus -- antibodies that then protected mice from lethal infection with this deadly strain. The ability of memory B cells to produce complex antibody responses against an infection nine decades after exposure speaks to their durability.
REASON #3: Vaccines or Natural Infection Trigger Strong Memory T Cell Immunity
All of the trials of the major COVID-19 vaccine candidates measured strong T cell immunity following vaccination, most often assessed by measuring SARS-CoV-2 specific T cells in the phase I/II safety and immunogenicity studies. There are a number of studies that demonstrate the production of strong T cell immunity to COVID-19 after natural infection as well, even when the infection was mild or asymptomatic.
The same study that showed us robust memory B cell production 8 months after natural infection also demonstrated strong and sustained memory T cell production. In fact, the half-lives of the memory T cells in this cohort were long (~125-225 days for CD8+ and ~94-153 days for CD4+ T cells), comparable to the 123-day half-life observed for memory CD8+ T cells after yellow fever immunization (a vaccine usually given once over a lifetime).
A recent study of individuals recovered from COVID-19 show that the initial T cells generated by natural infection mature and differentiate over time into memory T cells that will be "put in the bank" for sustained periods.
REASON #4: T Cell Immunity Following Vaccinations for Other Infections Is Long-Lasting
Last year, we were fortunate to be able to measure how T cell immunity is generated by COVID-19 vaccines, which was not possible in earlier eras when vaccine trials were done for other infections (such as measles, mumps, rubella, pertussis, diphtheria). Antibodies are just the "tip of the iceberg" when assessing the response to vaccination, but were the only arm of the immune response that could be measured following vaccination in the past.
Measuring pathogen-specific T cell responses takes sophisticated technology. However, T cell responses, when assessed years after vaccination for other pathogens, has been shown to be long-lasting. For example, in one study of 56 volunteers who had undergone measles vaccination when they were much younger, strong CD8 and CD4 cell responses to vaccination could be detected up to 34 years later.
REASON #5: T Cell Immunity to Related Coronaviruses That Caused Severe Disease is Long-Lasting
SARS-CoV-2 is a coronavirus that causes severe disease, unlike coronaviruses that cause the common cold. Two other coronaviruses in the recent past caused severe disease, specifically Severely Acute Respiratory Distress Syndrome (SARS) in late 2002-2003 and Middle East Respiratory Syndrome (MERS) in 2011.
A study performed in 2020 demonstrated that the blood of 23 recovered SARS patients possess long-lasting memory T cells that were still reactive to SARS 17 years after the outbreak in 2003. Many scientists expect that T cell immunity to SARS-CoV-2 will be equally durable to that of its cousin.
REASON #6: T Cell Responses from Vaccination and Natural Infection With the Ancestral Strain of COVID-19 Are Robust Against Variants
Even though antibody responses from vaccination may be slightly lower against various COVID-19 variants of concern that have emerged in recent months, T cell immunity after vaccination has been shown to be unperturbed by mutations in the spike protein (in the variants). For instance, T cell responses after mRNA vaccines maintained strong activity against different variants (including P.1 Brazil variant, B.1.1.7 UK variant, B.1.351 South Africa variant and the CA.20.C California variant) in a recent study.
Another study showed that the vaccines generated robust T cell immunity that was unfazed by different variants, including B.1.351 and B.1.1.7. The CD4 and CD8 responses generated after natural infection are equally robust, showing activity against multiple "epitopes" (little segments) of the spike protein of the virus. For instance, CD8 cells responds to 52 epitopes and CD4 cells respond to 57 epitopes across the spike protein, so that a few mutations in the variants cannot knock out such a robust and in-breadth T cell response. Indeed, a recent paper showed that mRNA vaccines were 97.4 percent effective against severe COVID-19 disease in Qatar, even when the majority of circulating virus there was from variants of concern (B.1.351 and B.1.1.7).
REASON #7: Coronaviruses Don't Mutate Quickly Like Influenza, Which Requires Annual Booster Shots
Coronaviruses are RNA viruses, like influenza and HIV (which is actually a retrovirus), but do not mutate as quickly as either one. The reason that coronaviruses don't mutate very rapidly is that their replicating mechanism (polymerase) has a strong proofreading mechanism: If the virus mutates, it usually goes back and self-corrects. Mutations can arise with high rates of replication when transmission is very frequent -- as has been seen in recent months with the emergence of SARS-CoV-2 variants during surges. However, the COVID-19 virus will not be mutating like this when we tamp down transmission with mass vaccination.
In conclusion, I and many of my infectious disease colleagues expect the immunity from natural infection or vaccination to COVID-19 to be durable. Let's put discussion of boosters aside and work hard on global vaccine equity and distribution since the pandemic is not over until it is over for us all.

