Trading syphilis for malaria: How doctors treated one deadly disease by infecting patients with another

In the 1920s, doctors induced a high fever in patients - so called "fever therapy" - as a way to help them recover from syphilis, though it involved ethical problems.
If you had lived one hundred years ago, syphilis – a bacterial infection spread by sexual contact – would likely have been one of your worst nightmares. Even though syphilis still exists, it can now be detected early and cured quickly with a course of antibiotics. Back then, however, before antibiotics and without an easy way to detect the disease, syphilis was very often a death sentence.
To understand how feared syphilis once was, it’s important to understand exactly what it does if it’s allowed to progress: the infections start off as small, painless sores or even a single sore near the vagina, penis, anus, or mouth. The sores disappear around three to six weeks after the initial infection – but untreated, syphilis moves into a secondary stage, often presenting as a mild rash in various areas of the body (such as the palms of a person’s hands) or through other minor symptoms. The disease progresses from there, often quietly and without noticeable symptoms, sometimes for decades before it reaches its final stages, where it can cause blindness, organ damage, and even dementia. Research indicates, in fact, that as much as 10 percent of psychiatric admissions in the early 20th century were due to dementia caused by syphilis, also known as neurosyphilis.
Like any bacterial disease, syphilis can affect kids, too. Though it’s spread primarily through sexual contact, it can also be transmitted from mother to child during birth, causing lifelong disability.
The poet-physician Aldabert Bettman, who wrote fictionalized poems based on his experiences as a doctor in the 1930s, described the effect syphilis could have on an infant in his poem Daniel Healy:
I always got away clean
when I went out
With the boys.
The night before
I was married
I went out,—But was not so fortunate;
And I infected
My bride.
When little Daniel
Was born
His eyes discharged;
And I dared not tell
That because
I had seen too much
Little Daniel sees not at all
Given the horrors of untreated syphilis, it’s maybe not surprising that people would go to extremes to try and treat it. One of the earliest remedies for syphilis, dating back to 15th century Naples, was using mercury – either rubbing it on the skin where blisters appeared, or breathing it in as a vapor. (Not surprisingly, many people who underwent this type of “treatment” died of mercury poisoning.)
Other primitive treatments included using tinctures made of a flowering plant called guaiacum, as well as inducing “sweat baths” to eliminate the syphilitic toxins. In 1910, an arsenic-based drug called Salvarsan hit the market and was hailed as a “magic bullet” for its ability to target and destroy the syphilis-causing bacteria without harming the patient. However, while Salvarsan was effective in treating early-stage syphilis, it was largely ineffective by the time the infection progressed beyond the second stage. Tens of thousands of people each year continued to die of syphilis or were otherwise shipped off to psychiatric wards due to neurosyphilis.
It was in one of these psychiatric units in the early 20th century that Dr. Julius Wagner-Juaregg got the idea for a potential cure.
Wagner-Juaregg was an Austrian-born physician trained in “experimental pathology” at the University of Vienna. Wagner-Juaregg started his medical career conducting lab experiments on animals and then moved on to work at different psychiatric clinics in Vienna, despite having no training in psychiatry or neurology.
Wagner-Juaregg’s work was controversial to say the least. At the time, medicine – particularly psychiatric medicine – did not have anywhere near the same rigorous ethical standards that doctors, researchers, and other scientists are bound to today. Wagner-Juaregg would devise wild theories about the cause of their psychiatric ailments and then perform experimental procedures in an attempt to cure them. (As just one example, Wagner-Juaregg would sterilize his adolescent male patients, thinking “excessive masturbation” was the cause of their schizophrenia.)
But sometimes these wild theories paid off. In 1883, during his residency, Wagner-Juaregg noted that a female patient with mental illness who had contracted a skin infection and suffered a high fever experienced a sudden (and seemingly miraculous) remission from her psychosis symptoms after the fever had cleared. Wagner-Juaregg theorized that inducing a high fever in his patients with neurosyphilis could help them recover as well.
Eventually, Wagner-Juaregg was able to put his theory to the test. Around 1890, Wagner-Juaregg got his hands on something called tuberculin, a therapeutic treatment created by the German microbiologist Robert Koch in order to cure tuberculosis. Tuberculin would later turn out to be completely ineffective for treating tuberculosis, often creating severe immune responses in patients – but for a short time, Wagner-Juaregg had some success in using tuberculin to help his dementia patients. Giving his patients tuberculin resulted in a high fever – and after completing the treatment, Wagner-Jauregg reported that his patient’s dementia was completely halted. The success was short-lived, however: Wagner-Juaregg eventually had to discontinue tuberculin as a treatment, as it began to be considered too toxic.
By 1917, Wagner-Juaregg’s theory about syphilis and fevers was becoming more credible – and one day a new opportunity presented itself when a wounded soldier, stricken with malaria and a related fever, was accidentally admitted to his psychiatric unit.
When his findings were published in 1918, Wagner-Juaregg’s so-called “fever therapy” swept the globe.
What Wagner-Juaregg did next was ethically deplorable by any standard: Before he allowed the soldier any quinine (the standard treatment for malaria at the time), Wagner-Juaregg took a small sample of the soldier’s blood and inoculated three syphilis patients with the sample, rubbing the blood on their open syphilitic blisters.
It’s unclear how well the malaria treatment worked for those three specific patients – but Wagner-Juaregg’s records show that in the span of one year, he inoculated a total of nine patients with malaria, for the sole purpose of inducing fevers, and six of them made a full recovery. Wagner-Juaregg’s treatment was so successful, in fact, that one of his inoculated patients, an actor who was unable to work due to his dementia, was eventually able to find work again and return to the stage. Two additional patients – a military officer and a clerk – recovered from their once-terminal illnesses and returned to their former careers as well.
When his findings were published in 1918, Wagner-Juaregg’s so-called “fever therapy” swept the globe. The treatment was hailed as a breakthrough – but it still had risks. Malaria itself had a mortality rate of about 15 percent at the time. Many people considered that to be a gamble worth taking, compared to dying a painful, protracted death from syphilis.
Malaria could also be effectively treated much of the time with quinine, whereas other fever-causing illnesses were not so easily treated. Triggering a fever by way of malaria specifically, therefore, became the standard of care.
Tens of thousands of people with syphilitic dementia would go on to be treated with fever therapy until the early 1940s, when a combination of Salvarsan and penicillin caused syphilis infections to decline. Eventually, neurosyphilis became rare, and then nearly unheard of.
Despite his contributions to medicine, it’s important to note that Wagner-Juaregg was most definitely not a person to idolize. In fact, he was an outspoken anti-Semite and proponent of eugenics, arguing that Jews were more prone to mental illness and that people who were mentally ill should be forcibly sterilized. (Wagner-Juaregg later became a Nazi sympathizer during Hitler’s rise to power even though, bizarrely, his first wife was Jewish.) Another problematic issue was that his fever therapy involved experimental treatments on many who, due to their cognitive issues, could not give informed consent.
Lack of consent was also a fundamental problem with the syphilis study at Tuskegee, appalling research that began just 14 years after Wagner-Juaregg published his “fever therapy” findings.
Still, despite his outrageous views, Wagner-Juaregg was awarded the Nobel Prize in Medicine or Physiology in 1927 – and despite some egregious human rights abuses, the miraculous “fever therapy” was partly responsible for taming one of the deadliest plagues in human history.
A Rare Disease Just "Messed with the Wrong Mother." Now She's Fighting to Beat It Once and For All.
Amber Freed and Maxwell near their home in Denver, Colorado.
Amber Freed felt she was the happiest mother on earth when she gave birth to twins in March 2017. But that euphoric feeling began to fade over the next few months, as she realized her son wasn't making the same developmental milestones as his sister. "I had a perfect benchmark because they were twins, and I saw that Maxwell was floppy—he didn't have muscle tone and couldn't hold his neck up," she recalls. At first doctors placated her with statements that boys sometimes develop slower than girls, but the difference was just too drastic. At 10 month old, Maxwell had never reached to grab a toy. In fact, he had never even used his hands.
Thinking that perhaps Maxwell couldn't see well, Freed took him to an ophthalmologist who was the first to confirm her worst fears. He didn't find Maxwell to have vision problems, but he thought there was something wrong with the boy's brain. He had seen similar cases before and they always turned out to be rare disorders, and always fatal. "Start preparing yourself for your child not to live," he had said.
Getting the diagnosis took months of painful, invasive procedures, as well as fighting with the health insurance to get the genetic testing approved. Finally, in June 2018, doctors at the Children's Hospital Colorado gave the Freeds their son's diagnosis—a genetic mutation so rare it didn't even have a name, just a bunch of letters jammed together into a word SLC6A1—same as the name of the mutated gene. The mutation, with only 40 cases known worldwide at the time, caused developmental disabilities, movement and speech disorders, and a debilitating form of epilepsy.
The doctors didn't know much about the disorder, but they said that Maxwell would also regress in his development when he turned three or four. They couldn't tell how long he would live. "Hopefully you would become an expert and educate us about it," they said, as they gave Freed a five-page paper on the SLC6A1 and told her to start calling scientists if she wanted to help her son in any way. When she Googled the name, nothing came up. She felt horrified. "Our disease was too rare to care."
Freed's husband, a 6'2'' college football player broke down in sobs and she realized that if anything could be done to help Maxwell, she'd have be the one to do it. "I understood that I had to fight like a mother," she says. "And a determined mother can do a lot of things."

The Freed family.
Courtesy Amber Freed
She quit her job as an equity analyst the day of the diagnosis and became a full-time SLC6A1 citizen scientist looking for researchers studying mutations of this gene. In the wee hours of the morning, she called scientists in Europe. As the day progressed, she called researchers on the East Coast, followed by the West in the afternoon. In the evening, she switched to Asia and Australia. She asked them the same question. "Can you help explain my gene and how do we fix it?"
Scientists need money to do research, so Freed launched Milestones for Maxwell fundraising campaign, and a SLC6A1 Connect patient advocacy nonprofit, dedicated to improving the lives of children and families battling this rare condition. And then it became clear that the mutation wasn't as rare as it seemed. As other parents began to discover her nonprofit, the number of known cases rose from 40 to 100, and later to 400, Freed says. "The disease is only rare until it messes with the wrong mother."
It took one mother to find another to start looking into what's happening inside Maxwell's brain. Freed came across Jeanne Paz, a Gladstone Institutes researcher who studies epilepsy with particular interest in absence or silent seizures—those that don't manifest by convulsions, but rather make patients absently stare into space—and that's one type of seizures Maxwell has. "It's like a brief period of silence in the brain during which the person doesn't pay attention to what's happening, and as soon as they come out of the seizure they are back to life," Paz explains. "It's like a pause button on consciousness." She was working to understand the underlying biology.
To understand how seizures begin, spread and stop, Paz uses optogenetics in mice. From words "genetic" and "optikós," which means visible in Greek, the optogenetics technique involves two steps. First, scientists introduce a light-sensitive gene into a specific brain cell type—for example into excitatory neurons that release glutamate, a neurotransmitter, which activates other cells in the brain. Then they implant a very thin optical fiber into the brain area where they forged these light-sensitive neurons. As they shine the light through the optical fiber, researchers can make excitatory neurons to release glutamate—or instead tell them to stop being active and "shut up". The ability to control what these neurons of interest do, quite literally sheds light onto where seizures start, how they propagate and what cells are involved in stopping them.
"Let's say a seizure started and we shine the light that reduces the activity of specific neurons," Paz explains. "If that stops the seizure, we know that activating those cells was necessary to maintain the seizure." Likewise, shutting down their activity will make the seizure stop.
Freed reached out to Paz in 2019 and the two women had an instant connection. They were both passionate about brain and seizures research, even if for different reasons. Freed asked Paz if she would study her son's seizures and Paz agreed.
To do that, Paz needed mice that carried the SLC6A1 mutation, so Freed found a company in China that created them to specs. The company replaced a mouse SLC6A1 gene with a human mutated one and shipped them over to Paz's lab. "We call them Maxwell mice," Paz says, "and we are now implanting electrodes into them to see which brain regions generate seizures." That would help them understand what goes wrong and what brain cells are malfunctioning in the SLC6A1 mice—and help scientists better understand what might cause seizures in children.
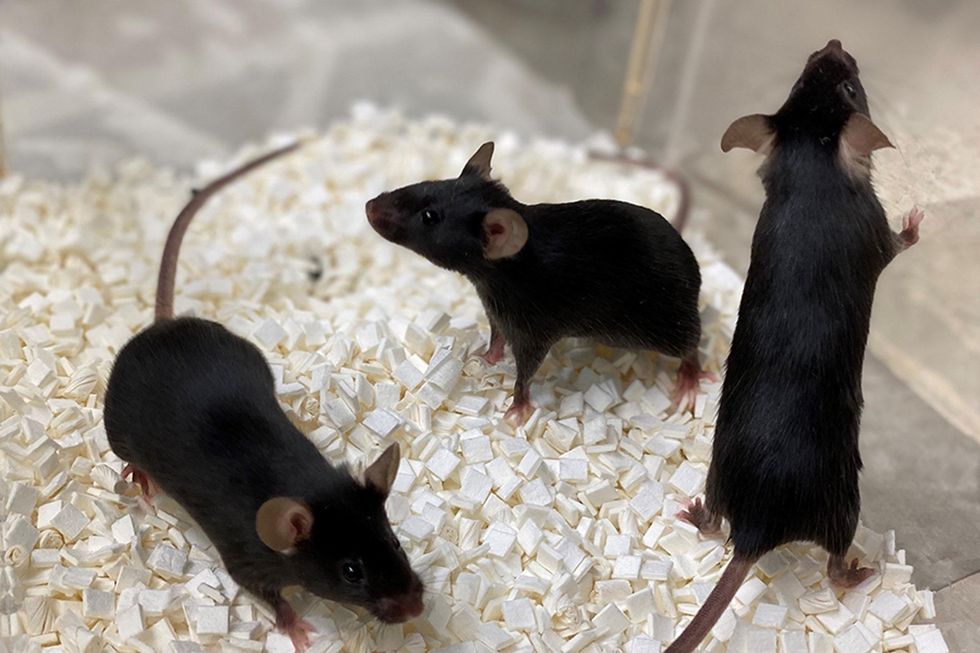
Bred to carry SLC6A1 mutation, these "Maxwell mice" will help better understand this debilitating genetic disease. (These mice are from Vanderbilt University, where researchers are also studying SLC6A1.)
Courtesy Amber Freed
This information—along with other research Amber is funding in other institutions—will inform the development of a novel genetic treatment, in which scientists would deploy a harmless virus to deliver a healthy, working copy of the SLC6A1 gene into the mice brains. They would likely deliver the therapeutic via a spinal tap infusion, and if it works and doesn't produce side effects in mice, the human trials will follow.
In the meantime, Freed is raising money to fund other research of various stop-gap measures. On April 22, 2021, she updated her Milestone for Maxwell page with a post that her nonprofit is funding yet another effort. It is a trial at Weill Cornell Medicine in New York City, in which doctors will use an already FDA-approved drug, which was recently repurposed for the SLC6A1 condition to treat epilepsy in these children. "It will buy us time," Freed says—while the gene therapy effort progresses.
Freed is determined to beat SLC6A1 before it beats down her family. She hopes to put an end to this disease—and similar genetic diseases—once and for all. Her goal is not only to have scientists create a remedy, but also to add the mutation to a newborn screening panel. That way, children born with this condition in the future would receive gene therapy before they even leave the hospital.
"I don't want there to be another Maxwell Freed," she says, "and that's why I am fighting like a mother." The gene therapy trial still might be a few years away, but the Weill Cornell one aims to launch very soon—possibly around Mother's Day. This is yet another milestone for Maxwell, another baby step forward—and the best gift a mother can get.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
On May 13th, scientific and medical experts will discuss and answer questions about the vaccine for those under 16.
This virtual event convened leading scientific and medical experts to address the public's questions and concerns about Covid-19 vaccines in kids and teens. Highlight video below.
DATE:
Thursday, May 13th, 2021
12:30 p.m. - 1:45 p.m. EDT
Dr. H. Dele Davies, M.D., MHCM

Senior Vice Chancellor for Academic Affairs and Dean for Graduate Studies at the University of Nebraska Medical (UNMC). He is an internationally recognized expert in pediatric infectious diseases and a leader in community health.
Dr. Emily Oster, Ph.D.

Professor of Economics at Brown University. She is a best-selling author and parenting guru who has pioneered a method of assessing school safety.
Dr. Tina Q. Tan, M.D.

Professor of Pediatrics at the Feinberg School of Medicine, Northwestern University. She has been involved in several vaccine survey studies that examine the awareness, acceptance, barriers and utilization of recommended preventative vaccines.
Dr. Inci Yildirim, M.D., Ph.D., M.Sc.

Associate Professor of Pediatrics (Infectious Disease); Medical Director, Transplant Infectious Diseases at Yale School of Medicine; Associate Professor of Global Health, Yale Institute for Global Health. She is an investigator for the multi-institutional COVID-19 Prevention Network's (CoVPN) Moderna mRNA-1273 clinical trial for children 6 months to 12 years of age.
About the Event Series
This event is the second of a four-part series co-hosted by Leaps.org, the Aspen Institute Science & Society Program, and the Sabin–Aspen Vaccine Science & Policy Group, with generous support from the Gordon and Betty Moore Foundation and the Howard Hughes Medical Institute.
:
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

