Trading syphilis for malaria: How doctors treated one deadly disease by infecting patients with another

In the 1920s, doctors induced a high fever in patients - so called "fever therapy" - as a way to help them recover from syphilis, though it involved ethical problems.
If you had lived one hundred years ago, syphilis – a bacterial infection spread by sexual contact – would likely have been one of your worst nightmares. Even though syphilis still exists, it can now be detected early and cured quickly with a course of antibiotics. Back then, however, before antibiotics and without an easy way to detect the disease, syphilis was very often a death sentence.
To understand how feared syphilis once was, it’s important to understand exactly what it does if it’s allowed to progress: the infections start off as small, painless sores or even a single sore near the vagina, penis, anus, or mouth. The sores disappear around three to six weeks after the initial infection – but untreated, syphilis moves into a secondary stage, often presenting as a mild rash in various areas of the body (such as the palms of a person’s hands) or through other minor symptoms. The disease progresses from there, often quietly and without noticeable symptoms, sometimes for decades before it reaches its final stages, where it can cause blindness, organ damage, and even dementia. Research indicates, in fact, that as much as 10 percent of psychiatric admissions in the early 20th century were due to dementia caused by syphilis, also known as neurosyphilis.
Like any bacterial disease, syphilis can affect kids, too. Though it’s spread primarily through sexual contact, it can also be transmitted from mother to child during birth, causing lifelong disability.
The poet-physician Aldabert Bettman, who wrote fictionalized poems based on his experiences as a doctor in the 1930s, described the effect syphilis could have on an infant in his poem Daniel Healy:
I always got away clean
when I went out
With the boys.
The night before
I was married
I went out,—But was not so fortunate;
And I infected
My bride.
When little Daniel
Was born
His eyes discharged;
And I dared not tell
That because
I had seen too much
Little Daniel sees not at all
Given the horrors of untreated syphilis, it’s maybe not surprising that people would go to extremes to try and treat it. One of the earliest remedies for syphilis, dating back to 15th century Naples, was using mercury – either rubbing it on the skin where blisters appeared, or breathing it in as a vapor. (Not surprisingly, many people who underwent this type of “treatment” died of mercury poisoning.)
Other primitive treatments included using tinctures made of a flowering plant called guaiacum, as well as inducing “sweat baths” to eliminate the syphilitic toxins. In 1910, an arsenic-based drug called Salvarsan hit the market and was hailed as a “magic bullet” for its ability to target and destroy the syphilis-causing bacteria without harming the patient. However, while Salvarsan was effective in treating early-stage syphilis, it was largely ineffective by the time the infection progressed beyond the second stage. Tens of thousands of people each year continued to die of syphilis or were otherwise shipped off to psychiatric wards due to neurosyphilis.
It was in one of these psychiatric units in the early 20th century that Dr. Julius Wagner-Juaregg got the idea for a potential cure.
Wagner-Juaregg was an Austrian-born physician trained in “experimental pathology” at the University of Vienna. Wagner-Juaregg started his medical career conducting lab experiments on animals and then moved on to work at different psychiatric clinics in Vienna, despite having no training in psychiatry or neurology.
Wagner-Juaregg’s work was controversial to say the least. At the time, medicine – particularly psychiatric medicine – did not have anywhere near the same rigorous ethical standards that doctors, researchers, and other scientists are bound to today. Wagner-Juaregg would devise wild theories about the cause of their psychiatric ailments and then perform experimental procedures in an attempt to cure them. (As just one example, Wagner-Juaregg would sterilize his adolescent male patients, thinking “excessive masturbation” was the cause of their schizophrenia.)
But sometimes these wild theories paid off. In 1883, during his residency, Wagner-Juaregg noted that a female patient with mental illness who had contracted a skin infection and suffered a high fever experienced a sudden (and seemingly miraculous) remission from her psychosis symptoms after the fever had cleared. Wagner-Juaregg theorized that inducing a high fever in his patients with neurosyphilis could help them recover as well.
Eventually, Wagner-Juaregg was able to put his theory to the test. Around 1890, Wagner-Juaregg got his hands on something called tuberculin, a therapeutic treatment created by the German microbiologist Robert Koch in order to cure tuberculosis. Tuberculin would later turn out to be completely ineffective for treating tuberculosis, often creating severe immune responses in patients – but for a short time, Wagner-Juaregg had some success in using tuberculin to help his dementia patients. Giving his patients tuberculin resulted in a high fever – and after completing the treatment, Wagner-Jauregg reported that his patient’s dementia was completely halted. The success was short-lived, however: Wagner-Juaregg eventually had to discontinue tuberculin as a treatment, as it began to be considered too toxic.
By 1917, Wagner-Juaregg’s theory about syphilis and fevers was becoming more credible – and one day a new opportunity presented itself when a wounded soldier, stricken with malaria and a related fever, was accidentally admitted to his psychiatric unit.
When his findings were published in 1918, Wagner-Juaregg’s so-called “fever therapy” swept the globe.
What Wagner-Juaregg did next was ethically deplorable by any standard: Before he allowed the soldier any quinine (the standard treatment for malaria at the time), Wagner-Juaregg took a small sample of the soldier’s blood and inoculated three syphilis patients with the sample, rubbing the blood on their open syphilitic blisters.
It’s unclear how well the malaria treatment worked for those three specific patients – but Wagner-Juaregg’s records show that in the span of one year, he inoculated a total of nine patients with malaria, for the sole purpose of inducing fevers, and six of them made a full recovery. Wagner-Juaregg’s treatment was so successful, in fact, that one of his inoculated patients, an actor who was unable to work due to his dementia, was eventually able to find work again and return to the stage. Two additional patients – a military officer and a clerk – recovered from their once-terminal illnesses and returned to their former careers as well.
When his findings were published in 1918, Wagner-Juaregg’s so-called “fever therapy” swept the globe. The treatment was hailed as a breakthrough – but it still had risks. Malaria itself had a mortality rate of about 15 percent at the time. Many people considered that to be a gamble worth taking, compared to dying a painful, protracted death from syphilis.
Malaria could also be effectively treated much of the time with quinine, whereas other fever-causing illnesses were not so easily treated. Triggering a fever by way of malaria specifically, therefore, became the standard of care.
Tens of thousands of people with syphilitic dementia would go on to be treated with fever therapy until the early 1940s, when a combination of Salvarsan and penicillin caused syphilis infections to decline. Eventually, neurosyphilis became rare, and then nearly unheard of.
Despite his contributions to medicine, it’s important to note that Wagner-Juaregg was most definitely not a person to idolize. In fact, he was an outspoken anti-Semite and proponent of eugenics, arguing that Jews were more prone to mental illness and that people who were mentally ill should be forcibly sterilized. (Wagner-Juaregg later became a Nazi sympathizer during Hitler’s rise to power even though, bizarrely, his first wife was Jewish.) Another problematic issue was that his fever therapy involved experimental treatments on many who, due to their cognitive issues, could not give informed consent.
Lack of consent was also a fundamental problem with the syphilis study at Tuskegee, appalling research that began just 14 years after Wagner-Juaregg published his “fever therapy” findings.
Still, despite his outrageous views, Wagner-Juaregg was awarded the Nobel Prize in Medicine or Physiology in 1927 – and despite some egregious human rights abuses, the miraculous “fever therapy” was partly responsible for taming one of the deadliest plagues in human history.
Real-Time Monitoring of Your Health Is the Future of Medicine
Implantable sensors and other surveillance technologies offer tremendous health benefits -- and ethical challenges.
The same way that it's harder to lose 100 pounds than it is to not gain 100 pounds, it's easier to stop a disease before it happens than to treat an illness once it's developed.
In Morris' dream scenario "everyone will be implanted with a sensor" ("…the same way most people are vaccinated") and the sensor will alert people to go to the doctor if something is awry.
Bio-engineers working on the next generation of diagnostic tools say today's technology, such as colonoscopies or mammograms, are reactionary; that is, they tell a person they are sick often when it's too late to reverse course. Surveillance medicine — such as implanted sensors — will detect disease at its onset, in real time.
What Is Possible?
Ever since the Human Genome Project — which concluded in 2003 after mapping the DNA sequence of all 30,000 human genes — modern medicine has shifted to "personalized medicine." Also called, "precision health," 21st-century doctors can in some cases assess a person's risk for specific diseases from his or her DNA. The information enables women with a BRCA gene mutation, for example, to undergo more frequent screenings for breast cancer or to pro-actively choose to remove their breasts, as a "just in case" measure.
But your DNA is not always enough to determine your risk of illness. Not all genetic mutations are harmful, for example, and people can get sick without a genetic cause, such as with an infection. Hence the need for a more "real-time" way to monitor health.
Aaron Morris, a postdoctoral researcher in the Department of Biomedical Engineering at the University of Michigan, wants doctors to be able to predict illness with pinpoint accuracy well before symptoms show up. Working in the lab of Dr. Lonnie Shea, the team is building "a tiny diagnostic lab" that can live under a person's skin and monitor for illness, 24/7. Currently being tested in mice, the Michigan team's porous biodegradable implant becomes part of the body as "cells move right in," says Morris, allowing engineered tissue to be biopsied and analyzed for diseases. The information collected by the sensors will enable doctors to predict disease flareups, such as for cancer relapses, so that therapies can begin well before a person comes out of remission. The technology will also measure the effectiveness of those therapies in real time.
In Morris' dream scenario "everyone will be implanted with a sensor" ("…the same way most people are vaccinated") and the sensor will alert people to go to the doctor if something is awry.
While it may be four or five decades before Morris' sensor becomes mainstream, "the age of surveillance medicine is here," says Jamie Metzl, a technology and healthcare futurist who penned Hacking Darwin: Genetic Engineering and the Future of Humanity. "It will get more effective and sophisticated and less obtrusive over time," says Metzl.
Already, Google compiles public health data about disease hotspots by amalgamating individual searches for medical symptoms; pill technology can digitally track when and how much medication a patient takes; and, the Apple watch heart app can predict with 85-percent accuracy if an individual using the wrist device has Atrial Fibrulation (AFib) — a condition that causes stroke, blood clots and heart failure, and goes undiagnosed in 700,000 people each year in the U.S.
"We'll never be able to predict everything," says Metzl. "But we will always be able to predict and prevent more and more; that is the future of healthcare and medicine."
Morris believes that within ten years there will be surveillance tools that can predict if an individual has contracted the flu well before symptoms develop.
At City College of New York, Ryan Williams, assistant professor of biomedical engineering, has built an implantable nano-sensor that works with a florescent wand to scope out if cancer cells are growing at the implant site. "Instead of having the ovary or breast removed, the patient could just have this [surveillance] device that can say 'hey we're monitoring for this' in real-time… [to] measure whether the cancer is maybe coming back,' as opposed to having biopsy tests or undergoing treatments or invasive procedures."
Not all surveillance technologies that are being developed need to be implanted. At Case Western, Colin Drummond, PhD, MBA, a data scientist and assistant department chair of the Department of Biomedical Engineering, is building a "surroundable." He describes it as an Alexa-style surveillance system (he's named her Regina) that will "tell" the user, if a need arises for medication, how much to take and when.
Bioethical Red Flags
"Everyone should be extremely excited about our move toward what I call predictive and preventive health care and health," says Metzl. "We should also be worried about it. Because all of these technologies can be used well and they can [also] be abused." The concerns are many layered:
Discriminatory practices
For years now, bioethicists have expressed concerns about employee-sponsored wellness programs that encourage fitness while also tracking employee health data."Getting access to your health data can change the way your employer thinks about your employability," says Keisha Ray, assistant professor at the University of Texas Health Science Center at Houston (UTHealth). Such access can lead to discriminatory practices against employees that are less fit. "Surveillance medicine only heightens those risks," says Ray.
Who owns the data?
Surveillance medicine may help "democratize healthcare" which could be a good thing, says Anita Ho, an associate professor in bioethics at both the University of California, San Francisco and at the University of British Columbia. It would enable easier access by patients to their health data, delivered to smart phones, for example, rather than waiting for a call from the doctor. But, she also wonders who will own the data collected and if that owner has the right to share it or sell it. "A direct-to-consumer device is where the lines get a little blurry," says Ho. Currently, health data collected by Apple Watch is owned by Apple. "So we have to ask bigger ethical questions in terms of what consent should be required" by users.
Insurance coverage
"Consumers of these products deserve some sort of assurance that using a product that will predict future needs won't in any way jeopardize their ability to access care for those needs," says Hastings Center bioethicist Carolyn Neuhaus. She is urging lawmakers to begin tackling policy issues created by surveillance medicine, now, well ahead of the technology becoming mainstream, not unlike GINA, the Genetic Information Nondiscrimination Act of 2008 -- a federal law designed to prevent discrimination in health insurance on the basis of genetic information.
And, because not all Americans have insurance, Ho wants to know, who's going to pay for this technology and how much will it cost?
Trusting our guts
Some bioethicists are concerned that surveillance technology will reduce individuals to their "risk profiles," leaving health care systems to perceive them as nothing more than a "bundle of health and security risks." And further, in our quest to predict and prevent ailments, Neuhaus wonders if an over-reliance on data could damage the ability of future generations to trust their gut and tune into their own bodies?
It "sounds kind of hippy-dippy and feel-goodie," she admits. But in our culture of medicine where efficiency is highly valued, there's "a tendency to not value and appreciate what one feels inside of their own body … [because] it's easier to look at data than to listen to people's really messy stories of how they 'felt weird' the other day. It takes a lot less time to look at a sheet, to read out what the sensor implanted inside your body or planted around your house says."
Ho, too, worries about lost narratives. "For surveillance medicine to actually work we have to think about how we educate clinicians about the utility of these devices and how to how to interpret the data in the broader context of patients' lives."
Over-diagnosing
While one of the goals of surveillance medicine is to cut down on doctor visits, Ho wonders if the technology will have the opposite effect. "People may be going to the doctor more for things that actually are benign and are really not of concern yet," says Ho. She is also concerned that surveillance tools could make healthcare almost "recreational" and underscores the importance of making sure that the goals of surveillance medicine are met before the technology is unleashed.
"We can't just assume that any of these technologies are inherently technologies of liberation."
AI doesn't fix existing healthcare problems
"Knowing that you're going to have a fall or going to relapse or have a disease isn't all that helpful if you have no access to the follow-up care and you can't afford it and you can't afford the prescription medication that's going to ward off the onset," says Neuhaus. "It may still be worth knowing … but we can't fool ourselves into thinking that this technology is going to reshape medicine in America if we don't pay attention to … the infrastructure that we don't currently have."
Race-based medicine
How surveillances devices are tested before being approved for human use is a major concern for Ho. In recent years, alerts have been raised about the homogeneity of study group participants — too white and too male. Ho wonders if the devices will be able to "accurately predict the disease progression for people whose data has not been used in developing the technology?" COVID-19 has killed Black people at a rate 2.5 time greater than white people, for example, and new, virtual clinical research is focused on recruiting more people of color.
The Biggest Question
"We can't just assume that any of these technologies are inherently technologies of liberation," says Metzl.
Especially because we haven't yet asked the 64-thousand dollar question: Would patients even want to know?
Jenny Ahlstrom is an IT professional who was diagnosed at 43 with multiple myeloma, a blood cancer that typically attacks people in their late 60s and 70s and for which there is no cure. She believes that most people won't want to know about their declining health in real time. People like to live "optimistically in denial most of the time. If they don't have a problem, they don't want to really think they have a problem until they have [it]," especially when there is no cure. "Psychologically? That would be hard to know."
Ahlstrom says there's also the issue of trust, something she experienced first-hand when she launched her non-profit, HealthTree, a crowdsourcing tool to help myeloma patients "find their genetic twin" and learn what therapies may or may not work. "People want to share their story, not their data," says Ahlstrom. "We have been so conditioned as a nation to believe that our medical data is so valuable."
Metzl acknowledges that adoption of new technologies will be uneven. But he also believes that "over time, it will be abundantly clear that it's much, much cheaper to predict and prevent disease than it is to treat disease once it's already emerged."
Beyond cost, the tremendous potential of these technologies to help us live healthier and longer lives is a game-changer, he says, as long as we find ways "to ultimately navigate this terrain and put systems in place ... to minimize any potential harms."
How Smallpox Was Wiped Off the Planet By a Vaccine and Global Cooperation
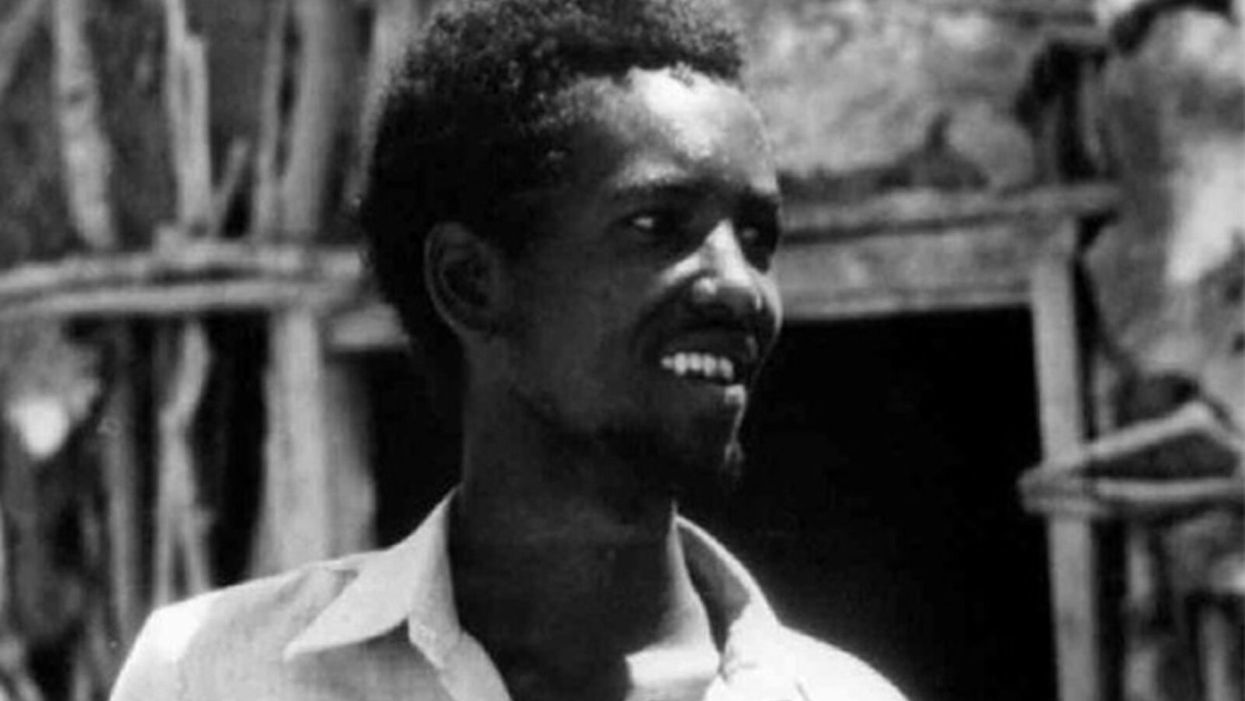
The world's last recorded case of endemic smallpox was in Ali Maow Maalin, of Merka, Somalia, in October 1977. He made a full recovery.
For 3000 years, civilizations all over the world were brutalized by smallpox, an infectious and deadly virus characterized by fever and a rash of painful, oozing sores.
Doctors had to contend with wars, floods, and language barriers to make their campaign a success.
Smallpox was merciless, killing one third of people it infected and leaving many survivors permanently pockmarked and blind. Although smallpox was more common during the 18th and 19th centuries, it was still a leading cause of death even up until the early 1950s, killing an estimated 50 million people annually.
A Primitive Cure
Sometime during the 10th century, Chinese physicians figured out that exposing people to a tiny bit of smallpox would sometimes result in a milder infection and immunity to the disease afterward (if the person survived). Desperate for a cure, people would huff powders made of smallpox scabs or insert smallpox pus into their skin, all in the hopes of getting immunity without having to get too sick. However, this method – called inoculation – didn't always work. People could still catch the full-blown disease, spread it to others, or even catch another infectious disease like syphilis in the process.
A Breakthrough Treatment
For centuries, inoculation – however imperfect – was the only protection the world had against smallpox. But in the late 18th century, an English physician named Edward Jenner created a more effective method. Jenner discovered that inoculating a person with cowpox – a much milder relative of the smallpox virus – would make that person immune to smallpox as well, but this time without the possibility of actually catching or transmitting smallpox. His breakthrough became the world's first vaccine against a contagious disease. Other researchers, like Louis Pasteur, would use these same principles to make vaccines for global killers like anthrax and rabies. Vaccination was considered a miracle, conferring all of the rewards of having gotten sick (immunity) without the risk of death or blindness.
Scaling the Cure
As vaccination became more widespread, the number of global smallpox deaths began to drop, particularly in Europe and the United States. But even as late as 1967, smallpox was still killing anywhere from 10 to 15 million people in poorer parts of the globe. The World Health Assembly (a decision-making body of the World Health Organization) decided that year to launch the first coordinated effort to eradicate smallpox from the planet completely, aiming for 80 percent vaccine coverage in every country in which the disease was endemic – a total of 33 countries.
But officials knew that eradicating smallpox would be easier said than done. Doctors had to contend with wars, floods, and language barriers to make their campaign a success. The vaccination initiative in Bangladesh proved the most challenging, due to its population density and the prevalence of the disease, writes journalist Laurie Garrett in her book, The Coming Plague.
In one instance, French physician Daniel Tarantola on assignment in Bangladesh confronted a murderous gang that was thought to be spreading smallpox throughout the countryside during their crime sprees. Without police protection, Tarantola confronted the gang and "faced down guns" in order to immunize them, protecting the villagers from repeated outbreaks.
Because not enough vaccines existed to vaccinate everyone in a given country, doctors utilized a strategy called "ring vaccination," which meant locating individual outbreaks and vaccinating all known and possible contacts to stop an outbreak at its source. Fewer than 50 percent of the population in Nigeria received a vaccine, for example, but thanks to ring vaccination, it was eradicated in that country nonetheless. Doctors worked tirelessly for the next eleven years to immunize as many people as possible.
The World Health Organization declared smallpox officially eradicated on May 8, 1980.
A Resounding Success
In November 1975, officials discovered a case of variola major — the more virulent strain of the smallpox virus — in a three-year-old Bangladeshi girl named Rahima Banu. Banu was forcibly quarantined in her family's home with armed guards until the risk of transmission had passed, while officials went door-to-door vaccinating everyone within a five-mile radius. Two years later, the last case of variola major in human history was reported in Somalia. When no new community-acquired cases appeared after that, the World Health Organization declared smallpox officially eradicated on May 8, 1980.
Because of smallpox, we now know it's possible to completely eliminate a disease. But is it likely to happen again with other diseases, like COVID-19? Some scientists aren't so sure. As dangerous as smallpox was, it had a few characteristics that made eradication possibly easier than for other diseases. Smallpox, for instance, has no animal reservoir, meaning that it could not circulate in animals and resurge in a human population at a later date. Additionally, a person who had smallpox once was guaranteed immunity from the disease thereafter — which is not the case for COVID-19.
In The Coming Plague, Japanese physician Isao Arita, who led the WHO's Smallpox Eradication Unit, admitted to routinely defying orders from the WHO, mobilizing to parts of the world without official approval and sometimes even vaccinating people against their will. "If we hadn't broken every single WHO rule many times over, we would have never defeated smallpox," Arita said. "Never."
Still, thanks to the life-saving technology of vaccines – and the tireless efforts of doctors and scientists across the globe – a once-lethal disease is now a thing of the past.