Trading syphilis for malaria: How doctors treated one deadly disease by infecting patients with another

In the 1920s, doctors induced a high fever in patients - so called "fever therapy" - as a way to help them recover from syphilis, though it involved ethical problems.
If you had lived one hundred years ago, syphilis – a bacterial infection spread by sexual contact – would likely have been one of your worst nightmares. Even though syphilis still exists, it can now be detected early and cured quickly with a course of antibiotics. Back then, however, before antibiotics and without an easy way to detect the disease, syphilis was very often a death sentence.
To understand how feared syphilis once was, it’s important to understand exactly what it does if it’s allowed to progress: the infections start off as small, painless sores or even a single sore near the vagina, penis, anus, or mouth. The sores disappear around three to six weeks after the initial infection – but untreated, syphilis moves into a secondary stage, often presenting as a mild rash in various areas of the body (such as the palms of a person’s hands) or through other minor symptoms. The disease progresses from there, often quietly and without noticeable symptoms, sometimes for decades before it reaches its final stages, where it can cause blindness, organ damage, and even dementia. Research indicates, in fact, that as much as 10 percent of psychiatric admissions in the early 20th century were due to dementia caused by syphilis, also known as neurosyphilis.
Like any bacterial disease, syphilis can affect kids, too. Though it’s spread primarily through sexual contact, it can also be transmitted from mother to child during birth, causing lifelong disability.
The poet-physician Aldabert Bettman, who wrote fictionalized poems based on his experiences as a doctor in the 1930s, described the effect syphilis could have on an infant in his poem Daniel Healy:
I always got away clean
when I went out
With the boys.
The night before
I was married
I went out,—But was not so fortunate;
And I infected
My bride.
When little Daniel
Was born
His eyes discharged;
And I dared not tell
That because
I had seen too much
Little Daniel sees not at all
Given the horrors of untreated syphilis, it’s maybe not surprising that people would go to extremes to try and treat it. One of the earliest remedies for syphilis, dating back to 15th century Naples, was using mercury – either rubbing it on the skin where blisters appeared, or breathing it in as a vapor. (Not surprisingly, many people who underwent this type of “treatment” died of mercury poisoning.)
Other primitive treatments included using tinctures made of a flowering plant called guaiacum, as well as inducing “sweat baths” to eliminate the syphilitic toxins. In 1910, an arsenic-based drug called Salvarsan hit the market and was hailed as a “magic bullet” for its ability to target and destroy the syphilis-causing bacteria without harming the patient. However, while Salvarsan was effective in treating early-stage syphilis, it was largely ineffective by the time the infection progressed beyond the second stage. Tens of thousands of people each year continued to die of syphilis or were otherwise shipped off to psychiatric wards due to neurosyphilis.
It was in one of these psychiatric units in the early 20th century that Dr. Julius Wagner-Juaregg got the idea for a potential cure.
Wagner-Juaregg was an Austrian-born physician trained in “experimental pathology” at the University of Vienna. Wagner-Juaregg started his medical career conducting lab experiments on animals and then moved on to work at different psychiatric clinics in Vienna, despite having no training in psychiatry or neurology.
Wagner-Juaregg’s work was controversial to say the least. At the time, medicine – particularly psychiatric medicine – did not have anywhere near the same rigorous ethical standards that doctors, researchers, and other scientists are bound to today. Wagner-Juaregg would devise wild theories about the cause of their psychiatric ailments and then perform experimental procedures in an attempt to cure them. (As just one example, Wagner-Juaregg would sterilize his adolescent male patients, thinking “excessive masturbation” was the cause of their schizophrenia.)
But sometimes these wild theories paid off. In 1883, during his residency, Wagner-Juaregg noted that a female patient with mental illness who had contracted a skin infection and suffered a high fever experienced a sudden (and seemingly miraculous) remission from her psychosis symptoms after the fever had cleared. Wagner-Juaregg theorized that inducing a high fever in his patients with neurosyphilis could help them recover as well.
Eventually, Wagner-Juaregg was able to put his theory to the test. Around 1890, Wagner-Juaregg got his hands on something called tuberculin, a therapeutic treatment created by the German microbiologist Robert Koch in order to cure tuberculosis. Tuberculin would later turn out to be completely ineffective for treating tuberculosis, often creating severe immune responses in patients – but for a short time, Wagner-Juaregg had some success in using tuberculin to help his dementia patients. Giving his patients tuberculin resulted in a high fever – and after completing the treatment, Wagner-Jauregg reported that his patient’s dementia was completely halted. The success was short-lived, however: Wagner-Juaregg eventually had to discontinue tuberculin as a treatment, as it began to be considered too toxic.
By 1917, Wagner-Juaregg’s theory about syphilis and fevers was becoming more credible – and one day a new opportunity presented itself when a wounded soldier, stricken with malaria and a related fever, was accidentally admitted to his psychiatric unit.
When his findings were published in 1918, Wagner-Juaregg’s so-called “fever therapy” swept the globe.
What Wagner-Juaregg did next was ethically deplorable by any standard: Before he allowed the soldier any quinine (the standard treatment for malaria at the time), Wagner-Juaregg took a small sample of the soldier’s blood and inoculated three syphilis patients with the sample, rubbing the blood on their open syphilitic blisters.
It’s unclear how well the malaria treatment worked for those three specific patients – but Wagner-Juaregg’s records show that in the span of one year, he inoculated a total of nine patients with malaria, for the sole purpose of inducing fevers, and six of them made a full recovery. Wagner-Juaregg’s treatment was so successful, in fact, that one of his inoculated patients, an actor who was unable to work due to his dementia, was eventually able to find work again and return to the stage. Two additional patients – a military officer and a clerk – recovered from their once-terminal illnesses and returned to their former careers as well.
When his findings were published in 1918, Wagner-Juaregg’s so-called “fever therapy” swept the globe. The treatment was hailed as a breakthrough – but it still had risks. Malaria itself had a mortality rate of about 15 percent at the time. Many people considered that to be a gamble worth taking, compared to dying a painful, protracted death from syphilis.
Malaria could also be effectively treated much of the time with quinine, whereas other fever-causing illnesses were not so easily treated. Triggering a fever by way of malaria specifically, therefore, became the standard of care.
Tens of thousands of people with syphilitic dementia would go on to be treated with fever therapy until the early 1940s, when a combination of Salvarsan and penicillin caused syphilis infections to decline. Eventually, neurosyphilis became rare, and then nearly unheard of.
Despite his contributions to medicine, it’s important to note that Wagner-Juaregg was most definitely not a person to idolize. In fact, he was an outspoken anti-Semite and proponent of eugenics, arguing that Jews were more prone to mental illness and that people who were mentally ill should be forcibly sterilized. (Wagner-Juaregg later became a Nazi sympathizer during Hitler’s rise to power even though, bizarrely, his first wife was Jewish.) Another problematic issue was that his fever therapy involved experimental treatments on many who, due to their cognitive issues, could not give informed consent.
Lack of consent was also a fundamental problem with the syphilis study at Tuskegee, appalling research that began just 14 years after Wagner-Juaregg published his “fever therapy” findings.
Still, despite his outrageous views, Wagner-Juaregg was awarded the Nobel Prize in Medicine or Physiology in 1927 – and despite some egregious human rights abuses, the miraculous “fever therapy” was partly responsible for taming one of the deadliest plagues in human history.
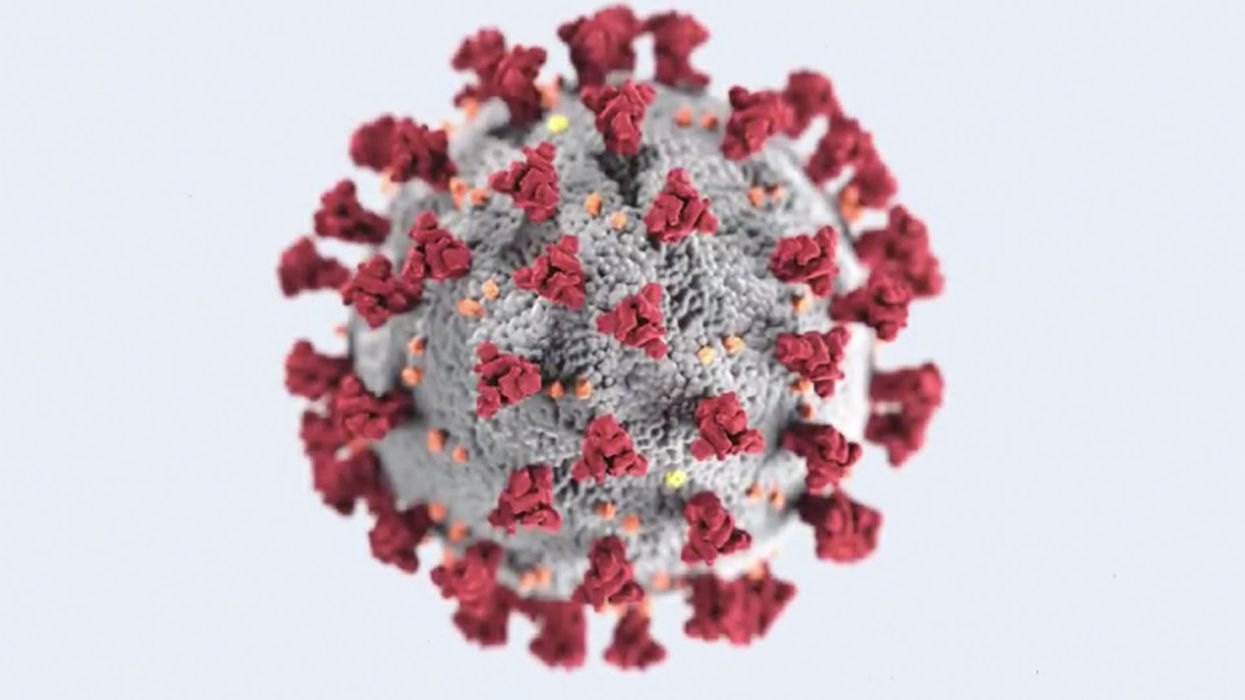
Blood Donated from Recovered Coronavirus Patients May Soon Yield a Stopgap Treatment
Antibodies from the blood of recovered patients is being tested as a stopgap treatment.
In October 1918, Lieutenant L.W. McGuire of the United States Navy sent a report to the American Journal of Public Health detailing a promising therapy that had already saved the lives of a number of officers suffering from pneumonia complications due to the Spanish influenza outbreak.
"These antibodies then become essentially drugs."
McGuire described how transfusions of blood from recovered patients – an idea which had first been trialed during a polio epidemic in 1916 – had led to rapid recovery in a series of severe pneumonia cases at a Naval Hospital in Massachusetts. "It is believed the serum has a decided influence in shortening the course of the disease, and lowering the mortality," he wrote.
Now more than a century on, this treatment – long forgotten in the western world - is once again coming to the fore during the current COVID-19 pandemic. With fatalities continuing to rise, and no vaccine expected for many months, experts are urging medical centers across the U.S. and Europe to initiate collaborations between critical care and transfusion services to offer this as an emergency treatment for those who need it most.
As of March 20, there are more than 90,000 individuals globally who have recovered from the disease. Some scientists believe that the blood of many of these people contains high levels of neutralizing antibodies that can kill the virus.
"These antibodies then become essentially drugs," said Arturo Casadevall, professor of Molecular Microbiology & Immunology at John Hopkins Bloomberg School of Public Health, who is currently co-ordinating a clinical trial of convalescent serum for COVID-19 involving 20 institutions across the US.
"We're talking about preparing a therapy right out of the serum of those that have recovered. It could also be used in patients who are already sick, but have not progressed to respiratory failure, to treat them before they enter intensive care units. That will provide a lot of support because there's a limited number of respirators and resources."
The first conclusive data on how the blood of recovered patients can help tackle COVID-19 is set to come out of China, where it was also used as an emergency treatment during the SARS and MERS outbreaks. On February 9, a severely ill patient in Wuhan was treated with convalescent serum and since then, hospitals across China have used the therapy on a total of 245 patients, with 91 reportedly showing an improvement in symptoms.
In China alone, more than 58,000 patients have now recovered from COVID-19. Casadevall said that last week the country shipped 90 tons of serum and plasma from these patients to Italy – the center of the pandemic in Europe – for emergency use.
Some of the first people to be treated are likely to be doctors and nurses in hospitals who are most at risk of exposure.
A current challenge, however, is that the blood donation from the recovered patients must be precisely timed in order to maximize the number of antibodies a future patient receives. Doctors in China say that obtaining the necessary blood samples at the right time is one of the major barriers to applying the treatment on a larger scale.
"It's difficult to get the donations," said Dr. Yuan Shi of Chongqing Medical University. "When patients have recovered from the disease, we would like to collect their blood two to four weeks afterwards. We try our best to call back the patients, but it's sometimes difficult to get them to come back within that time period."
Because of such hurdles, Japan's largest drugmaker, Takeda Pharmaceuticals, is now working to turn neutralizing antibodies from recovered COVID-19 patients into a standardized drug product. They hope to launch a clinical trial for this in the next few months.
In the U.S., Casadevall hopes blood transfusions from recovered patients can become clinically available as a therapy within the next four weeks, once regulatory approval has been received. Some of the first people to be treated are likely to be doctors and nurses in hospitals who are most at risk of exposure, to provide a protective boost in their immunity.
"A lot of healthcare workers in the U.S. have already been asked to quarantine, and you can imagine what effect that's going to have on the healthcare system," he said. "It can't take large numbers of people staying home; there's not the capacity."
But not all medical experts are convinced it's the way to go, especially when it comes to the most severe cases of COVID-19. "There's no knowing whether that treatment would be useful or not," warned Dr. Andrew Freedman, head of Cardiff University's School of Medicine in the U.K.
"There are going to be better things available in a few months, but we are facing, 'What do you do now?'"
However, Casadevall says that the treatment is not envisioned as a panacea to treating coronavirus, but simply a temporary measure which could give doctors some options until stronger options such as vaccines or new drugs are available.
"This is a stopgap option," he said. "There are going to be better things available in a few months, but we are facing, 'What do you do now?' The only thing we can offer severely ill people at the moment is respiratory support and oxygen, and we don't have anything to prevent those exposed from going on and getting ill."
Social distancing is a critical part of the strategy to defeat the novel coronavirus.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.