The First Cloned Monkeys Provoked More Shrugs Than Shocks

Zhong Zhong and Hua Hua, the two cloned macaques.
A few months ago, it was announced that not one, but two healthy long-tailed macaque monkeys were cloned—a first for primates of any kind. The cells were sourced from aborted monkey fetuses and the DNA transferred into eggs whose nuclei had been removed, the same method that was used in 1996 to clone "Dolly the Sheep." Two live births, females named Zhong Zhong and Hua Hua, resulted from 60 surrogate mothers. Inefficient, it's true. But over time, the methods are likely to be improved.
The scientist who supervised the project predicts that cloning, along with gene editing, will result in "ideal primate models" for studying disease mechanisms and drug screening.
Dr. Gerald Schatten, a famous would-be monkey cloner, authored a controversial paper in 2003 describing the formidable challenges to cloning monkeys and humans, speculating that the feat might never be accomplished. Now, some 15 years later, that prediction, insofar as it relates to monkeys, has blown away.
Zhong Zhong and Hua Hua were created at the Chinese Academy of Science's Institute of Neuroscience in Shanghai. The Institute founded in 1999 boasts 32 laboratories, expanding to 50 labs in 2020. It maintains two non-human primate research facilities.
The founder and director, Dr. Mu-ming Poo, supervised the project. Poo is an extremely accomplished senior researcher at the pinnacle of his field, a distinguished professor emeritus in Biology at UC Berkeley. In 2016, he was awarded the prestigious $500,000 Gruber Neuroscience Prize. At that time, Poo's experiments were described by a colleague as being "innovative and very often ingenious."
Poo maintains the reputation of studying some of the most important questions in cellular neuroscience.
But is society ready to accept cloned primates for medical research without the attendant hysteria about fears of cloned humans?
By Western standards, use of non-human primates in research focuses on the welfare of the animal subjects. As PETA reminds us, there is a dreadful and sad history of mistreatment. Dr. Poo assures us that his cloned monkeys are treated ethically and that the Institute is compliant with the highest regulatory standards, as promulgated by the U.S. National Institutes of Health.
He presents the noblest justifications for the research. He predicts that cloning, along with gene editing, will result in "ideal primate models" for studying disease mechanisms and drug screening. He declares that this will eventually help to solve Parkinson's, Huntington's and Alzheimer's disease.
But is society ready to accept cloned primates for medical research without the attendant hysteria about fears of cloned humans? It appears so.
While much of the news coverage expressed this predictable worry, my overall impression is that the societal response was muted. Where was the expected outrage? Then again, we've come a long way since Dolly the Sheep in terms of both the science and the cultural acceptance of cloning. Perhaps my unique vantage point can provide perspective on how much attitudes have evolved.
Perhaps my unique vantage point can provide perspective on how much attitudes have evolved.
I sometimes joke that I am the world's only human cloning lawyer—a great gig but there are still no clients.
I first crashed into the cloning scene in 2002 when I sued the so-called human cloning company "Clonaid" and asked in court to have a temporary guardian appointed for the alleged first human clone "Baby Eve." The claim needed to be tested, and mine was the first case ever aiming to protect the rights of a human clone. My legal basis was child welfare law, protecting minors from abuse, negligence, and exploitation.
The case had me on back-to-back global television broadcasts around the world; there was live news and "breathless" coverage at the courthouse emblazoned in headlines in every language on the planet. Cloning was, after all, perceived as a species-altering event: asexual reproduction. The controversy dominated world headlines for month until Clonaid's claim was busted as the "fakest" of fake news.
Fresh off the cloning case, the scientific community reached out to me, seeing me as the defender of legitimate science, an opponent of cloning human babies but a proponent of using cloning techniques to accelerate ethical regenerative medicine and embryonic stem cell research in general.
The years 2003 to 2006 were the era of the "stem cell wars" and a dominant issue was human cloning. Social conservative lawmakers around the world were seeking bans or criminalization not only of cloning babies but also the cloning of cells to match the donor's genetics. Scientists were being threatened with fines and imprisonment. Human cloning was being challenged in the United Nations with the United States backing a global treaty to ban and morally condemn all cloning -- including the technique that was crucial for research.
Scientists and patients were touting the cloning technique as a major biomedical breakthrough because cells could be created as direct genetic matches from a specific donor.
At the same time, scientists and patients were touting the cloning technique as a major biomedical breakthrough because cells could be created as direct genetic matches from a specific donor.
So my organization organized a conference at UN headquarters to defend research cloning and all the big names in stem cell research were there. We organized petitions to the UN and faxed 35,000 signatures to the country mission. These ongoing public policy battles were exacerbated in part because of the growing fear that cloning babies was just around the corner.
Then in 2005, the first cloned dog stunned the world, an Afghan hound named Snuppy. I met him when I visited the laboratories of Professor Woo Suk Hwang in Korea. His minders let me hold his leash -- TIME magazine's scientific breakthrough of the year. He didn't lick me or even wag his tail; I figured he must not like lawyers.
Tragically, soon thereafter, I witnessed firsthand Dr. Hwang's fall from grace when his human stem cell cloning breakthroughs proved false. The massive scientific misconduct rocked the nation of Korea, stem cell science in general, and provoked terrible news coverage.
Nevertheless, by 2007, the proposed bans lost steam, overridden by the advent of a Japanese researcher's Nobel Prize winning formula for reprogramming human cells to create genetically matched cell lines, not requiring the destruction of human embryos.
After years of panic, none of the recent cloning headlines has caused much of a stir.
Five years later, when two American scientists accomplished therapeutic human cloned stem cell lines, their news was accepted without hysteria. Perhaps enough time had passed since Hwang and the drama was drained.
In the just past 30 days we have seen more cloning headlines. Another cultural icon, Barbara Streisand, revealed she owns two cloned Coton de Tulear puppies. The other weekend, the television news show "60 Minutes" devoted close to an hour on the cloned ponies used at the top level of professional polo. And in India, scientists just cloned the first Assamese buffalo.
And you know what? After years of panic, none of this has caused much of a stir. It's as if the future described by Alvin Toffler in "Future Shock" has arrived and we are just living with it. A couple of cloned monkeys barely move the needle.
Perhaps it is the advent of the Internet and the overall dilution of wonder and outrage. Or maybe the muted response is rooted in popular culture. From Orphan Black to the plotlines of dozens of shows and books, cloning is just old news. The hand-wringing discussions about "human dignity" and "slippery slopes" have taken a backseat to the AI apocalypse and Martian missions.
We humans are enduring plagues of dementia and Alzheimer's, and we will need more monkeys. I will take mine cloned, if it will speed progress.
Personally, I still believe that cloned children should not be an option. Child welfare laws might be the best deterrent.
The same does not hold for cloning monkey research subjects. Squeamishness aside, I think Zhong Zhong and Hua Hua will soon be joined by a legion of cloned macaques and probably marmosets.
We humans are enduring plagues of dementia and Alzheimer's, and we will need more monkeys. I will take mine cloned, if it will speed the mending of these consciousness-destroying afflictions.
Scientific revolutions once took centuries, then decades, and now seem to bombard us daily. The convergence of technologies has accelerated the future. To Zhong Zhong and Hua Hua, my best wishes with the hope that their sacrifices will contribute to the health of all primates -- not just humans.
Recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen as soon as 18 months from now
Like all those whose kidneys have failed, Scott Burton’s life revolves around dialysis. For nearly two decades, Burton has been hooked up (or, since 2020, has hooked himself up at home) to a dialysis machine that performs the job his kidneys normally would. The process is arduous, time-consuming, and expensive. Except for a brief window before his body rejected a kidney transplant, Burton has depended on machines to take the place of his kidneys since he was 12-years-old. His whole life, the 39-year-old says, revolves around dialysis.
“Whenever I try to plan anything, I also have to plan my dialysis,” says Burton says, who works as a freelance videographer and editor. “It’s a full-time job in itself.”
Many of those on dialysis are in line for a kidney transplant that would allow them to trade thrice-weekly dialysis and strict dietary limits for a lifetime of immunosuppressants. Burton’s previous transplant means that his body will likely reject another donated kidney unless it matches perfectly—something he’s not counting on. It’s why he’s enthusiastic about the development of artificial kidneys, small wearable or implantable devices that would do the job of a healthy kidney while giving users like Burton more flexibility for traveling, working, and more.
Still, the devices aren’t ready for testing in humans—yet. But recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen as soon as 18 months from now, according to Jonathan Himmelfarb, a nephrologist at the University of Washington.
“It would liberate people with kidney failure,” Himmelfarb says.
An engineering marvel
Compared to the heart or the brain, the kidney doesn’t get as much respect from the medical profession, but its job is far more complex. “It does hundreds of different things,” says UCLA’s Ira Kurtz.
Kurtz would know. He’s worked as a nephrologist for 37 years, devoting his career to helping those with kidney disease. While his colleagues in cardiology and endocrinology have seen major advances in the development of artificial hearts and insulin pumps, little has changed for patients on hemodialysis. The machines remain bulky and require large volumes of a liquid called dialysate to remove toxins from a patient’s blood, along with gallons of purified water. A kidney transplant is the next best thing to someone’s own, functioning organ, but with over 600,000 Americans on dialysis and only about 100,000 kidney transplants each year, most of those in kidney failure are stuck on dialysis.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. Each of the 45 different cell types in the kidney do something different.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. To build an artificial heart, Kurtz says, you basically need to engineer a pump. An artificial pancreas needs to balance blood sugar levels with insulin secretion. While neither of these tasks is simple, they are fairly straightforward. The kidney, on the other hand, does more than get rid of waste products like urea and other toxins. Each of the 45 different cell types in the kidney do something different, helping to regulate electrolytes like sodium, potassium, and phosphorous; maintaining blood pressure and water balance; guiding the body’s hormonal and inflammatory responses; and aiding in the formation of red blood cells.
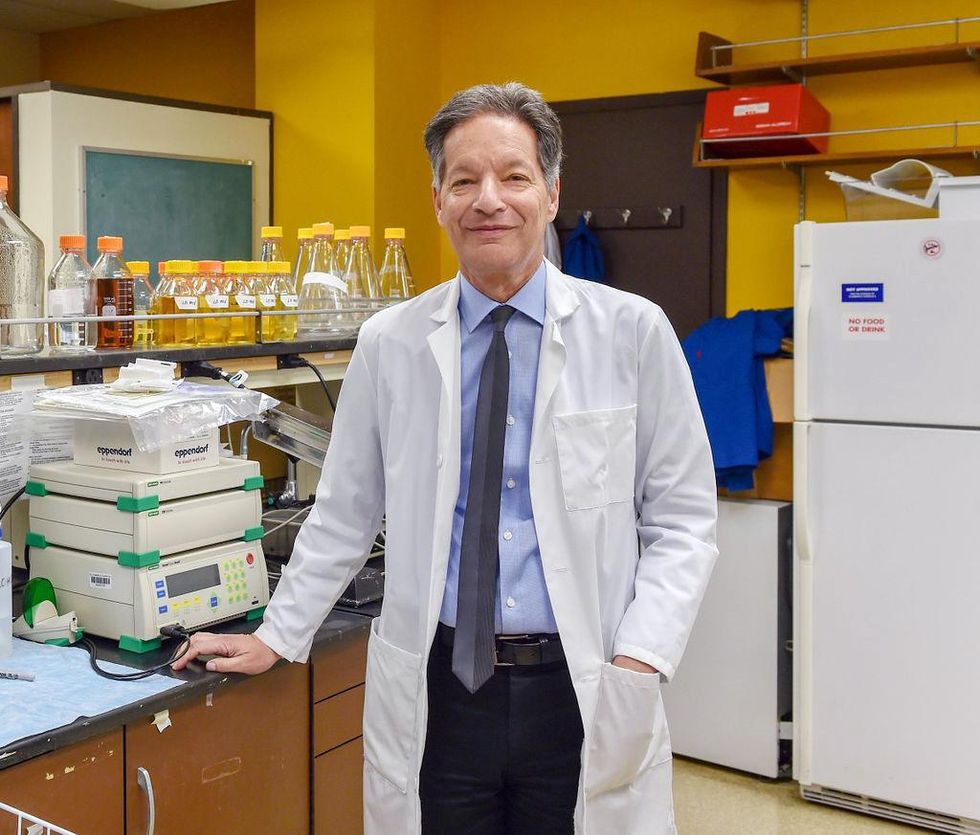
There's been little progress for patients during Ira Kurtz's 37 years as a nephrologist. Artificial kidneys would change that.
UCLA
Dialysis primarily filters waste, and does so well enough to keep someone alive, but it isn’t a true artificial kidney because it doesn’t perform the kidney’s other jobs, according to Kurtz, such as sensing levels of toxins, wastes, and electrolytes in the blood. Due to the size and water requirements of existing dialysis machines, the equipment isn’t portable. Physicians write a prescription for a certain duration of dialysis and assess how well it’s working with semi-regular blood tests. The process of dialysis itself, however, is conducted blind. Doctors can’t tell how much dialysis a patient needs based on kidney values at the time of treatment, says Meera Harhay, a nephrologist at Drexel University in Philadelphia.
But it’s the impact of dialysis on their day-to-day lives that creates the most problems for patients. Only one-quarter of those on dialysis are able to remain employed (compared to 85% of similar-aged adults), and many report a low quality of life. Having more flexibility in life would make a major different to her patients, Harhay says.
“Almost half their week is taken up by the burden of their treatment. It really eats away at their freedom and their ability to do things that add value to their life,” she says.
Art imitates life
The challenge for artificial kidney designers was how to compress the kidney’s natural functions into a portable, wearable, or implantable device that wouldn’t need constant access to gallons of purified and sterilized water. The other universal challenge they faced was ensuring that any part of the artificial kidney that would come in contact with blood was kept germ-free to prevent infection.
As part of last year’s KidneyX Prize, a partnership between the U.S. Department of Health and Human Services and the American Society of Nephrology, inventors were challenged to create prototypes for artificial kidneys. Himmelfarb’s team at the University of Washington’s Center for Dialysis Innovation won the prize by focusing on miniaturizing existing technologies to create a portable dialysis machine. The backpack sized AKTIV device (Ambulatory Kidney to Increase Vitality) will recycle dialysate in a closed loop system that removes urea from blood and uses light-based chemical reactions to convert the urea to nitrogen and carbon dioxide, which allows the dialysate to be recirculated.
Himmelfarb says that the AKTIV can be used when at home, work, or traveling, which will give users more flexibility and freedom. “If you had a 30-pound device that you could put in the overhead bins when traveling, you could go visit your grandkids,” he says.
Kurtz’s team at UCLA partnered with the U.S. Kidney Research Corporation and Arkansas University to develop a dialysate-free desktop device (about the size of a small printer) as the first phase of a progression that will he hopes will lead to something small and implantable. Part of the reason for the artificial kidney’s size, Kurtz says, is the number of functions his team are cramming into it. Not only will it filter urea from blood, but it will also use electricity to help regulate electrolyte levels in a process called electrodeionization. Kurtz emphasizes that these additional functions are what makes his design a true artificial kidney instead of just a small dialysis machine.
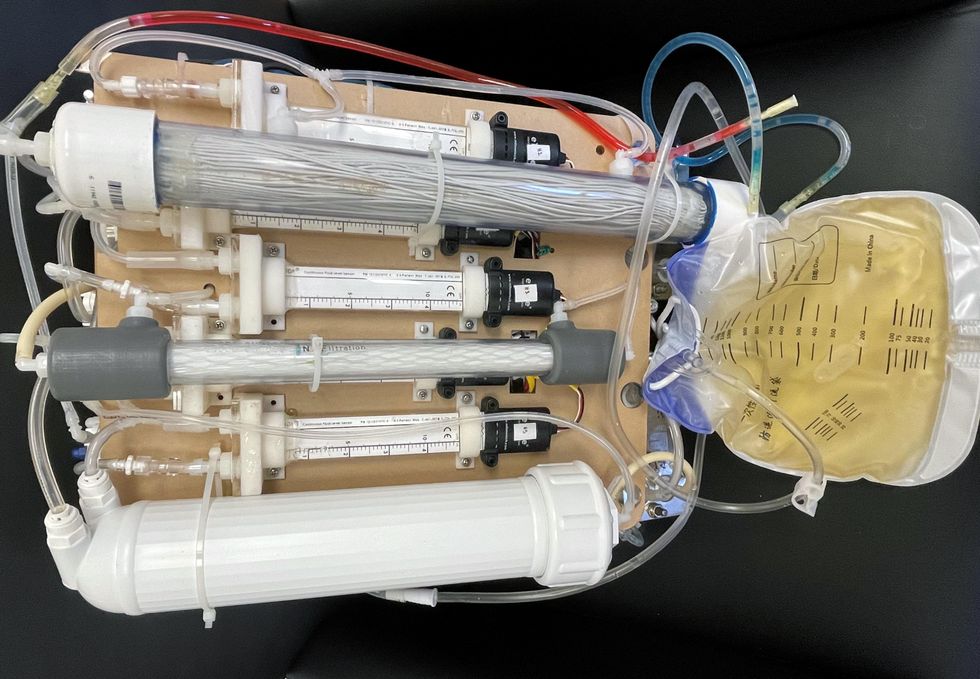
One version of an artificial kidney.
UCLA
“It doesn't have just a static function. It has a bank of sensors that measure chemicals in the blood and feeds that information back to the device,” Kurtz says.
Other startups are getting in on the game. Nephria Bio, a spinout from the South Korean-based EOFlow, is working to develop a wearable dialysis device, akin to an insulin pump, that uses miniature cartridges with nanomaterial filters to clean blood (Harhay is a scientific advisor to Nephria). Ian Welsford, Nephria’s co-founder and CTO, says that the device’s design means that it can also be used to treat acute kidney injuries in resource-limited settings. These potentials have garnered interest and investment in artificial kidneys from the U.S. Department of Defense.
For his part, Burton is most interested in an implantable device, as that would give him the most freedom. Even having a regular outpatient procedure to change batteries or filters would be a minor inconvenience to him.
“Being plugged into a machine, that’s not mimicking life,” he says.
Today’s more than 20,000 mental health apps have a wide range of functionalities and business models. Many of them can be useful for depression.
Even before the pandemic created a need for more telehealth options, depression was a hot area of research for app developers. Given the high prevalence of depression and its connection to suicidality — especially among today’s teenagers and young adults who grew up with mobile devices, use them often, and experience these conditions with alarming frequency — apps for depression could be not only useful but lifesaving.
“For people who are not depressed, but have been depressed in the past, the apps can be helpful for maintaining positive thinking and behaviors,” said Andrea K. Wittenborn, PhD, director of the Couple and Family Therapy Doctoral Program and a professor in human development and family studies at Michigan State University. “For people who are mildly to severely depressed, apps can be a useful complement to working with a mental health professional.”
Health and fitness apps, in general, number in the hundreds of thousands. These are driving a market expected to reach $102.45 billion by next year. The mobile mental health app market is a small part of this but still sizable at $500 million, with revenues generated through user health insurance, employers, and direct payments from individuals.
Apps can provide data that health professionals cannot gather on their own. People’s constant interaction with smartphones and wearable devices yields data on many health conditions for millions of patients in their natural environments and while they go about their usual activities. Compared with the in-office measurements of weight and blood pressure and the brevity of doctor-patient interactions, the thousands of data points gathered unobtrusively over an extended time period provide a far better and more detailed picture of the person and their health.
At their most advanced level, apps for mental health, including depression, passively gather data on how the user touches and interacts with the mobile device through changes in digital biomarkers that relate to depressive symptoms and other conditions.
Building on three decades of research since early “apps” were used for delivering treatment manuals to health professionals, today’s more than 20,000 mental health apps have a wide range of functionalities and business models. Many of these apps can be useful for depression.
Some apps primarily provide a virtual connection to a group of mental health professionals employed or contracted by the app. Others have options for meditation, sleeping or, in the case of industry leaders Calm and Headspace, overall well-being. On the cutting edge are apps that detect changes in a person’s use of mobile devices and their interactions with them.
Apps such as AbleTo, Happify Health, and Woebot Health focus on cognitive behavioral therapy, a type of counseling with proven potential to change a person’s behaviors and feelings. “CBT has been demonstrated in innumerable studies over the last several decades to be effective in the treatment of behavioral health conditions such as depression and anxiety disorders,” said Dr. Reena Pande, chief medical officer at AbleTo. “CBT is intended to be delivered as a structured intervention incorporating key elements, including behavioral activation and adaptive thinking strategies.”
These CBT skills help break the negative self-talk (rumination) common in patients with depression. They are taught and reinforced by some self-guided apps, using either artificial intelligence or programmed interactions with users. Apps can address loneliness and isolation through connections with others, even when a symptomatic person doesn’t feel like leaving the house.
At their most advanced level, apps for mental health, including depression, passively gather data on how the user touches and interacts with the mobile device through changes in “digital biomarkers” that can be associated with onset or worsening of depressive symptoms and other cognitive conditions. In one study, Mindstrong Health gathered a year’s worth of data on how people use their smartphones, such as scrolling through articles, typing and clicking. Mindstrong, whose founders include former leaders of the National Institutes of Health, modeled the timing and order of these actions to make assessments that correlated closely with gold-standard tests of cognitive function.
National organizations of mental health professionals have been following the expanding number of available apps over the years with keen interest. App Advisor is an initiative of the American Psychiatric Association that helps psychiatrists and other mental health professionals navigate the issues raised by mobile health technology. App Advisor does not rate or recommend particular apps but rather provides guidance about why apps should be assessed and how health professionals can do this.
A website that does review mental health apps is One Mind Psyber Guide, an independent nonprofit that partners with several national organizations. One Mind users can select among numerous search terms for the condition and therapeutic approach of interest. Apps are rated on a five-point scale, with reviews written by professionals in the field.
Do mental health apps related to depression have the kind of safety and effectiveness data required for medications and other medical interventions? Not always — and not often. Yet the overall results have shown early promise, Wittenborn noted.
“Studies that have attempted to detect depression from smartphone and wearable sensors [during a single session] have ranged in accuracy from about 86 to 89 percent,” Wittenborn said. “Studies that tried to predict changes in depression over time have been less accurate, with accuracy ranging from 59 to 85 percent.”
The Food and Drug Administration encourages the development of apps and has approved a few of them—mostly ones used by health professionals—but it is generally “hands off,” according to the American Psychiatric Association. The FDA has published a list of examples of software (including programming of apps) that it does not plan to regulate because they pose low risk to the public. First on the list is software that helps patients with diagnosed psychiatric conditions, including depression, maintain their behavioral coping skills by providing a “Skill of the Day” technique or message.
On its App Advisor site, the American Psychiatric Association says mental health apps can be dangerous or cause harm in multiple ways, such as by providing false information, overstating the app’s therapeutic value, selling personal data without clearly notifying users, and collecting data that isn’t relevant to mental health.
Although there is currently reason for caution, patients may eventually come to expect mental health professionals to recommend apps, especially as their rating systems, features and capabilities expand. Through such apps, patients might experience more and higher quality interactions with their mental health professionals. “Apps will continue to be refined and become more effective through future research,” said Wittenborn. “They will become more integrated into practice over time.”