The Promise of Pills That Know When You Swallow Them

A woman prepares to swallow a digital pill that can track whether she has taken her medication.
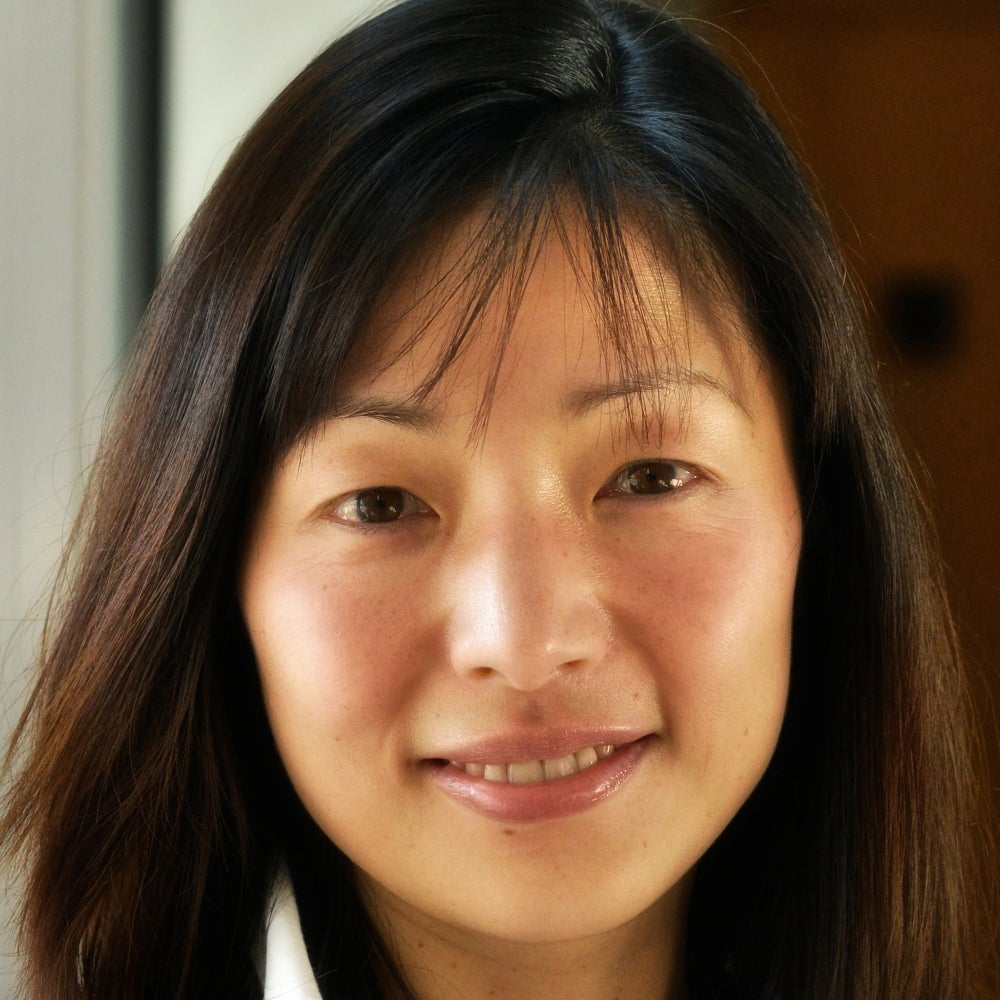
Dr. Sara Browne, an associate professor of clinical medicine at the University of California, San Diego, is a specialist in infectious diseases and, less formally, "a global health person." She often travels to southern Africa to meet with colleagues working on the twin epidemics of HIV and tuberculosis.
"This technology, in my opinion, is an absolute slam dunk for tuberculosis."
Lately she has asked them to name the most pressing things she can help with as a researcher based in a wealthier country. "Over and over and over again," she says, "the only thing they wanted to know is whether their patients are taking the drugs."
Tuberculosis is one of world's deadliest diseases; every year there are 10 million new infections and more than a million deaths. When a patient with tuberculosis is prescribed medicine to combat the disease, adherence to the regimen is important not just for the individual's health, but also for the health of the community. Poor adherence can lead to lengthier and more costly treatment and, perhaps more importantly, to drug-resistant strains of the disease -- an increasing global threat.
Browne is testing a new method to help healthcare workers track their patients' adherence with greater precision—close to exact precision even. They're called digital pills, and they involve a patient swallowing medicine as they normally would, only the capsule contains a sensor that—when it contacts stomach acid—transmits a signal to a small device worn on or near the body. That device in turn sends a signal to the patient's phone or tablet and into a cloud-based database. The fact that the pill has been swallowed has therefore been recorded almost in real time, and notice is available to whoever has access to the database.
"This technology, in my opinion, is an absolute slam dunk for tuberculosis," Browne says. TB is much more prevalent in poorer regions of the world—in Sub-Saharan Africa, for example—than in richer places like the U.S., where Browne's studies thus far have taken place. But when someone is diagnosed in the U.S., because of the risk to others if it spreads, they will likely have to deal with "directly observed therapy" to ensure that they take their medicines correctly.
DOT, as it's called, requires the patient to meet with a healthcare worker several days a week, or every day, so that the medicine intake can be observed in person -- an expensive and time-consuming process. Still, the Centers for Disease Control and Prevention website says (emphasis theirs), "DOT should be used for ALL patients with TB disease, including children and adolescents. There is no way to accurately predict whether a patient will adhere to treatment without this assistance."
Digital pills can help with both the cost and time involved, and potentially improve adherence in places where DOT is impossibly expensive. With the sensors, you can monitor a patient's adherence without a healthcare worker physically being in the room. Patients can live their normal lives and if they miss a pill, they can receive a reminder by text or a phone call from the clinic or hospital. "They can get on with their lives," said Browne. "They don't need the healthcare system to interrupt them."
A 56-year-old patient who participated in one of Browne's studies when he was undergoing TB treatment says that before he started taking the digital pills, he would go to the clinic at least once every day, except weekends. Once he switched to digital pills, he could go to work and spend time with his wife and children instead of fighting traffic every day to get to the clinic. He just had to wear a small patch on his abdomen, which would send the signal to a tablet provided by Browne's team. When he returned from work, he could see the results—that he'd taken the pill—in a database accessed via the tablet. (He could also see his heart rate and respiratory rate.) "I could do my daily activities without interference," he said.
Dr. Peter Chai, a medical toxicologist and emergency medicine physician at Brigham and Women's Hospital in Boston, is studying digital pills in a slightly different context, to help fight the country's opioid overdose crisis. Doctors like Chai prescribe pain medicine, he says, but then immediately put the onus on the patient to decide when to take it. This lack of guidance can lead to abuse and addiction. Patients are often told to take the meds "as needed." Chai and his colleagues wondered, "What does that mean to patients? And are people taking more than they actually need? Because pain is such a subjective experience."
The patients "liked the fact that somebody was watching them."
They wanted to see what "take as needed" actually led to, so they designed a study with patients who had broken a bone and come to the hospital's emergency department to get it fixed. Those who were prescribed oxycodone—a pharmaceutical opioid for pain relief—got enough digital pills to last one week. They were supposed to take the pills as needed, or as many as three pills per day. When the pills were ingested, the sensor sent a signal to a card worn on a lanyard around the neck.
Chai and his colleagues were able to see exactly when the patients took the pills and how many, and to detect patterns of ingestion more precisely than ever before. They talked to the patients after the seven days were up, and Chai said most were happy to be taking digital pills. The patients saw it as a layer of protection from afar. "They liked the fact that somebody was watching them," Chai said.
Both doctors, Browne and Chai, are in early stages of studies with patients taking pre-exposure prophylaxis, medicines that can protect people with a high-risk of contracting HIV, such as injectable drug users. Without good adherence, patients leave themselves open to getting the virus. If a patient is supposed to take a pill at 2 p.m. but the digital pill sensor isn't triggered, the healthcare provider can have an automatic message sent as a reminder. Or a reminder to one of the patient's friends or loved ones.
"Like Swallowing Your Phone"?
Deven Desai, an associate professor of law and ethics at Georgia Tech, says that digital pills sound like a great idea for helping with patient adherence, a big issue that self-reporting doesn't fully solve. He likes the idea of a physician you trust having better information about whether you're taking your medication on time. "On the surface that's just cool," he says. "That's a good thing." But Desai, who formerly worked as academic research counsel at Google, said that some of the same questions that have come up in recent years with social media and the Internet in general also apply to digital pills.
"Think of it like your phone, but you swallowed it," he says. "At first it could be great, simple, very much about the user—in this case, the patient—and the data is going between you and your doctor and the medical people it ought to be going to. Wonderful. But over time, phones change. They become 'smarter.'" And when phones and other technologies become smarter, he says, the companies behind them tend to expand the type of data they collect, because they can. Desai says it will be crucial that prescribers be completely transparent about who is getting the patients' data and for what purpose.
"We're putting stuff in our body in good faith with our medical providers, and what if it turned out later that all of a sudden someone was data mining or putting in location trackers and we never knew about that?" Desai asks. "What science has to realize is if they don't start thinking about this, what could be a wonderful technology will get killed."
Leigh Turner, an associate professor at the University of Minnesota's Center for Bioethics, agrees with Desai that digital pills have great promise, and also that there are clear reasons to be concerned about their use. Turner compared the pills to credit cards and social media, in that the data from them can potentially be stolen or leaked. One question he would want answered before the pills were normalized: "What kind of protective measures are in place to make sure that personal information isn't spilling out and being acquired by others or used by others in unexpected and unwanted ways?"
If digital pills catch on, some experts worry that they may one day not be a voluntary technology.
Turner also wonders who will have access to the pills themselves. Only those who can afford both the medicine plus the smartphones that are currently required for their use? Or will people from all economic classes have access? If digital pills catch on, he also worries they may one day not be a voluntary technology.
"When it comes to digital pills, it's not something that's really being foisted on individuals. It's more something that people can be informed of and can choose to take or not to take," he says. "But down the road, I can imagine a scenario where we move away from purely voluntary agreements to it becoming more of an expectation."
He says it's easy to picture a scenario in which insurance companies demand that patient medicinal intake data be tracked and collected or else. Refuse to have your adherence tracked and you risk higher rates or even overall coverage. Maybe patients who don't take the digital pills suffer dire consequences financially or medically. "Maybe it becomes beneficial as much to health insurers and payers as it is to individual patients," Turner says.
In November 2017, the FDA approved the first-ever digital pill that includes a sensor, a drug called Abilify MyCite, made by Otsuka Pharmaceutical Company. The drug, which is yet to be released, is used to treat schizophrenia, bipolar disorder, and depression. With a built-in sensor developed by Proteus Digital Health, patients can give their doctors permission to see when exactly they are taking, or not taking, their meds. For patients with mental illness, the ability to help them stick to their prescribed regime can be life-saving.
But Turner wonders if Abilify is the best drug to be a forerunner for digital pills. Some people with schizophrenia might be suffering from paranoia, and perhaps giving them a pill developed by a large corporation that sends data from their body to be tracked by other people might not be the best idea. It could in fact exacerbate their sense of paranoia.
The Bottom Line: Protect the Data
We all have relatives who have pillboxes with separate compartments for each day of the week, or who carry pillboxes that beep when it's time to take the meds. But that's not always good enough for people with dementia, mental illness, drug addiction, or other life situations that make it difficult to remember to take their pills. Digital pills can play an important role in helping these people.
"The absolute principle here is that the data has to belong to the patient."
The one time the patient from Browne's study forgot to take his pills, he got a beeping reminder from his tablet that he'd missed a dose. "Taking a medication on a daily basis, sometimes we just forget, right?" he admits. "With our very accelerated lives nowadays, it helps us to remember that we have to take the medications. So patients are able to be on top of their own treatment."
Browne is convinced that digital pills can help people in developing countries with high rates of TB and HIV, though like Turner and Desai she cautions that patients' data must be protected. "I think it can be a tremendous technology for patient empowerment and I also think if properly used it can help the medical system to support patients that need it," she said. "But the absolute principle here is that the data has to belong to the patient."
Biohackers Made a Cheap and Effective Home Covid Test -- But No One Is Allowed to Use It
A stock image of a home test for COVID-19.
Last summer, when fast and cheap Covid tests were in high demand and governments were struggling to manufacture and distribute them, a group of independent scientists working together had a bit of a breakthrough.
Working on the Just One Giant Lab platform, an online community that serves as a kind of clearing house for open science researchers to find each other and work together, they managed to create a simple, one-hour Covid test that anyone could take at home with just a cup of hot water. The group tested it across a network of home and professional laboratories before being listed as a semi-finalist team for the XPrize, a competition that rewards innovative solutions-based projects. Then, the group hit a wall: they couldn't commercialize the test.
They wanted to keep their project open source, making it accessible to people around the world, so they decided to forgo traditional means of intellectual property protection and didn't seek patents. (They couldn't afford lawyers anyway). And, as a loose-knit group that was not supported by a traditional scientific institution, working in community labs and homes around the world, they had no access to resources or financial support for manufacturing or distributing their test at scale.
But without ethical and regulatory approval for clinical testing, manufacture, and distribution, they were legally unable to create field tests for real people, leaving their inexpensive, $16-per-test, innovative product languishing behind, while other, more expensive over-the-counter tests made their way onto the market.
Who Are These Radical Scientists?
Independent, decentralized biomedical research has come of age. Also sometimes called DIYbio, biohacking, or community biology, depending on whom you ask, open research is today a global movement with thousands of members, from scientists with advanced degrees to middle-grade students. Their motivations and interests vary across a wide spectrum, but transparency and accessibility are key to the ethos of the movement. Teams are agile, focused on shoestring-budget R&D, and aim to disrupt business as usual in the ivory towers of the scientific establishment.
Ethics oversight is critical to ensuring that research is conducted responsibly, even by biohackers.
Initiatives developed within the community, such as Open Insulin, which hopes to engineer processes for affordable, small-batch insulin production, "Slybera," a provocative attempt to reverse engineer a $1 million dollar gene therapy, and the hundreds of projects posted on the collaboration platform Just One Giant Lab during the pandemic, all have one thing in common: to pursue testing in humans, they need an ethics oversight mechanism.
These groups, most of which operate collaboratively in community labs, homes, and online, recognize that some sort of oversight or guidance is useful—and that it's the right thing to do.
But also, and perhaps more immediately, they need it because federal rules require ethics oversight of any biomedical research that's headed in the direction of the consumer market. In addition, some individuals engaged in this work do want to publish their research in traditional scientific journals, which—you guessed it—also require that research has undergone an ethics evaluation. Ethics oversight is critical to ensuring that research is conducted responsibly, even by biohackers.
Bridging the Ethics Gap
The problem is that traditional oversight mechanisms, such as institutional review boards at government or academic research institutions, as well as the private boards utilized by pharmaceutical companies, are not accessible to most independent researchers. Traditional review boards are either closed to the public, or charge fees that are out of reach for many citizen science initiatives. This has created an "ethics gap" in nontraditional scientific research.
Biohackers are seen in some ways as the direct descendents of "white hat" computer hackers, or those focused on calling out security holes and contributing solutions to technical problems within self-regulating communities. In the case of health and biotechnology, those problems include both the absence of treatments and the availability of only expensive treatments for certain conditions. As the DIYbio community grows, there needs to be a way to provide assurance that, when the work is successful, the public is able to benefit from it eventually. The team that developed the one-hour Covid test found a potential commercial partner and so might well overcome the oversight hurdle, but it's been 14 months since they developed the test--and counting.
In short, without some kind of oversight mechanism for the work of independent biomedical researchers, the solutions they innovate will never have the opportunity to reach consumers.
In a new paper in the journal Citizen Science: Theory & Practice, we consider the issue of the ethics gap and ask whether ethics oversight is something nontraditional researchers want, and if so, what forms it might take. Given that individuals within these communities sometimes vehemently disagree with each other, is consensus on these questions even possible?
We learned that there is no "one size fits all" solution for ethics oversight of nontraditional research. Rather, the appropriateness of any oversight model will depend on each initiative's objectives, needs, risks, and constraints.
We also learned that nontraditional researchers are generally willing (and in some cases eager) to engage with traditional scientific, legal, and bioethics experts on ethics, safety, and related questions.
We suggest that these experts make themselves available to help nontraditional researchers build infrastructure for ethics self-governance and identify when it might be necessary to seek outside assistance.
Independent biomedical research has promise, but like any emerging science, it poses novel ethical questions and challenges. Existing research ethics and oversight frameworks may not be well-suited to answer them in every context, so we need to think outside the box about what we can create for the future. That process should begin by talking to independent biomedical researchers about their activities, priorities, and concerns with an eye to understanding how best to support them.
Christi Guerrini, JD, MPH studies biomedical citizen science and is an Associate Professor at Baylor College of Medicine. Alex Pearlman, MA, is a science journalist and bioethicist who writes about emerging issues in biotechnology. They have recently launched outlawbio.org, a place for discussion about nontraditional research.
Sept. 13th Event: Delta, Vaccines, and Breakthrough Infections
A visualization of the virus that causes COVID-19.
This virtual event will convene leading scientific and medical experts to address the public's questions and concerns about COVID-19 vaccines, Delta, and breakthrough infections. Audience Q&A will follow the panel discussion. Your questions can be submitted in advance at the registration link.
DATE:
Monday, September 13th, 2021
12:30 p.m. - 1:45 p.m. EDT
REGISTER:

Dr. Amesh Adalja, M.D., FIDSA, Senior Scholar, Johns Hopkins Center for Health Security; Adjunct Assistant Professor, Johns Hopkins Bloomberg School of Public Health; Affiliate of the Johns Hopkins Center for Global Health. His work is focused on emerging infectious disease, pandemic preparedness, and biosecurity.

Dr. Nahid Bhadelia, M.D., MALD, Founding Director, Boston University Center for Emerging Infectious Diseases Policy and Research (CEID); Associate Director, National Emerging Infectious Diseases Laboratories (NEIDL), Boston University; Associate Professor, Section of Infectious Diseases, Boston University School of Medicine. She is an internationally recognized leader in highly communicable and emerging infectious diseases (EIDs) with clinical, field, academic, and policy experience in pandemic preparedness.
Dr. Akiko Iwasaki, Ph.D., Waldemar Von Zedtwitz Professor of Immunobiology and Molecular, Cellular and Developmental Biology and Professor of Epidemiology (Microbial Diseases), Yale School of Medicine; Investigator, Howard Hughes Medical Institute. Her laboratory researches how innate recognition of viral infections lead to the generation of adaptive immunity, and how adaptive immunity mediates protection against subsequent viral challenge.
 Dr. Marion Pepper, Ph.D., Associate Professor, Department of Immunology, University of Washington. Her lab studies how cells of the adaptive immune system, called CD4+ T cells and B cells, form immunological memory by visualizing their differentiation, retention, and function.
Dr. Marion Pepper, Ph.D., Associate Professor, Department of Immunology, University of Washington. Her lab studies how cells of the adaptive immune system, called CD4+ T cells and B cells, form immunological memory by visualizing their differentiation, retention, and function.
This event is the third of a four-part series co-hosted by Leaps.org, the Aspen Institute Science & Society Program, and the Sabin–Aspen Vaccine Science & Policy Group, with generous support from the Gordon and Betty Moore Foundation and the Howard Hughes Medical Institute.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.