The Real Science Behind “Anti-Aging” Beauty Products

The beauty industry heavily hypes the nascent promise of stem cells for rejuvenation.
The beauty market abounds with high-end creams and serums that claim the use of stem cells to rejuvenate aging skin.
Selling on the internet and at department stores like Nordstrom, these products promise "breakthrough" applications to plump, smooth, and "reverse visible signs of aging," and at least one product offers to create a "regenerative firming serum, moisturizer, and eye cream" from customers' own stem cells – for a whopping $1200.
The beauty industry is heavily hyping glimmers of the nascent field of stem cell therapy.
Steeped in clinical-sounding terms like "proteins and peptides from pluripotent stem cells," the marketing of these products evokes a dramatic restoration of youthfulness based on cutting-edge science. But the beauty industry is heavily hyping glimmers of the nascent field of stem cell therapy. So what is real and what's not? And is there in fact a way to harness the potential of stem cells in the service of beauty?
Plant vs. Human Stem Cells
Stem cells do indeed have tremendous promise for treating a wide range of diseases and conditions. The cells come from early-stage embryos or, more commonly, from umbilical cord blood or our own bodies. Embryonic stem cells are considered the body's "master" cells because they can develop into any of our several hundred cell types. Adult stem cells, on the other hand, reside in mature tissues and organs like the brain, bone marrow, and skin, and their versatility is more limited. As an internal repair system for many tissue types, they replenish sick, injured, and worn-out cells.
Nowadays, with some sophisticated chemical coaxing, adult stem cells can be returned to an embryonic-like blank state, with the ability to become any cell type that the body might need.
Beauty product manufacturers convey in their advertising that the rejuvenating power of these cells could hold the key to the fountain of youth. But there's something the manufacturers don't always tell you: their products do not typically use human stem cells.
"The whole concept of stem cells is intriguing to the public," says Tamara Griffiths, a consultant dermatologist for the British Skin Foundation. "But what these products contain is plant stem cells and, more commonly, chemicals that have been derived from plant stem cells."
The plant stem cells are cultured in the lab with special media to get them to produce signaling proteins and peptides, like cytokines and chemokines. These have been shown to be good for reducing inflammation and promoting healthy cell functioning, even if derived from plants. However, according to Griffiths, there are so many active ingredients in these products that it's hard to say just what role each one of them plays. We do know that their ability to replenish human stem cells is extremely limited, and the effects of plant stem cells on human cells are unproven.
"...any cosmetic that is advertised to be anti-aging due to plant stem cells at this time is about as effective as all the skin creams without stem cells."
Whether products containing plant cell-derived ingredients work better than conventional skin products is unknown because these products are not regulated by the U.S. Food and Drug Administration and may rest on dubious, even more or less nonexistent, research. Cosmetics companies have conducted most of the research and the exact formulas they devise are considered proprietary information. They have no incentive to publish their research findings, and they don't have to meet standards imposed by the FDA unless they start using human cells in their products.
"There are biological limits to what you can do with plant cells in the first place," says Griffiths. "No plant stem cell is going to morph into a human skin cell no matter what magic medium you immerse it in. Nor is a plant cell likely to stimulate the production of human stem cells if applied to the skin."
According to Sarah Baucus, a cell biologist, for any type of stem cell to be of any use whatsoever, the cells must be alive. The processing needed to incorporate living cells into any type of cream or serum would inevitably kill them, rendering them useless. The splashy marketing of these products suggests that results may be drastic, but none of these creams is likely to produce the kind of rejuvenating effect that would be on par with a facelift or several other surgical or dermatological procedures.
"Plant stem cell therapy needs to move in the right direction to implement its inherent potential in skin care," researchers wrote in a 2017 paper in the journal Future Science OA. "This might happen in the next 20 years but any cosmetic that is advertised to be anti-aging due to plant stem cells at this time is about as effective as all the skin creams without stem cells."
From Beauty Counter to Doctor's Clinic
Where do you turn if you still want to harness the power of stem cells to reinvigorate the skin? Is there a legitimate treatment using human cells? The answer is possibly, but for that you have to switch from the Nordstrom cosmetics counter to a clinic with a lab, where plastic surgeons work with specialists who culture and manipulate living cells.
Plastic surgeons are experts in wound healing, a process in which stem cells play a prominent role. Doctors have long used the technique of taking fat from the body and injecting it into hollowed-out or depressed areas of the face to fill in injuries, correct wrinkles, and improve the face's curvature. Lipotransfer, or the harvesting of body fat and injecting it into the face, has been around for many years in traditional plastic surgery clinics. In recent years, some plastic surgeons have started to cull stem cells from fat. One procedure that does just that is called cell-assisted lipotransfer, or CAL.
In CAL, adipose tissue, or fat, is harvested by liposuction, usually from the lower abdomen. Fat contains stem cells that can differentiate into several cell types, including skin, muscle, cartilage, and bone. Fat tissue has an especially stem cell-rich layer. These cells are then mixed with some regular fat, making in effect a very stem cell-rich fat solution, right in the doctor's office. The process of manipulating the fat cells takes about 90 to 110 minutes, and then the solution is ready to be injected into the skin, to fill in the lips, the cheeks, and the nasolabial folds, or the deep folds around the nose and mouth.
Unlike regular fat, which is often injected into the face, some experts claim that the cell-enriched fat has better, longer-lasting results. The tissue graft grows its own blood vessels, an advantage that may lead to a more long-lasting graft – though the research is mixed, with some studies showing they do and other studies showing the complete opposite.
For almost all stem cell products on the market today in the U.S., it is not yet known whether they are safe or effective, despite how they are marketed.
One of the pioneers in CAL, a plastic surgeon in Brazil named Dr. Aris Sterodimas, says that the stem cells secrete growth factors that rejuvenate the skin -- like the plant stem cells that are used in topical creams and serums. Except that these cells are human stem cells and hence have inherently more potential in the human body.
Note that CAL doesn't actually result in large numbers of fresh, new replacement cells, as might be imagined. It's simply fat tissue treated to make it richer in stem cells, to have more of the growth-inducing proteins and peptides delivered to the dermis layer of the skin.
Sterodimas works alongside a tissue engineer to provide CAL in his clinic. He uses it as a way to rebuild soft tissues in people disfigured by accidents or diseases, or who are suffering the after-effects of radiation treatments for cancer.
Plastic surgeons get plenty of these patients. But how widespread is CAL for beauty purposes? Sterodimas says that he regularly performs the procedure for Brazilians, and it's widely available in Europe and Japan. In the U.S., the procedure hasn't taken off because there is no FDA approval for the various methods used by different doctors and clinics. A few major academic centers in the U.S. offer the treatment on a clinical trials basis and there are several trials ongoing.
But there is a downside to all lipotransfers: the transplanted fat will eventually be absorbed by the body. Even the cell-enriched fat has a limited lifespan before reabsorption. That means if you like the cosmetic results of CAL, you'll have to repeat the treatment about every two years to maintain the plumping, firming, and smoothing effects on the skin. The results of CAL are "superior to the results of laser treatments and other plastic surgery interventions, though the effect is not as dramatic as a facelift," says Sterodimas.
Buyer Beware
For almost all stem cell products on the market today in the U.S., it is not yet known whether they are safe or effective, despite how they are marketed. There are around 700 clinics in the U.S. offering stem cell treatments and up to 20,000 people have received these therapies. However, the only FDA-approved stem cell treatments use cells from bone marrow or cord blood to treat cancers of the blood and bone marrow. Safety concerns have prompted the FDA to announce increased oversight of stem cell clinics.
As for CAL, most of the clinical trials so far have been focused on using it for breast reconstruction after mastectomy, and results are mixed. Experts warn that the procedure has yet to be proven safe as well as effective. It's important to remember that this newborn science is in the early stages of research.
One question that has also not been definitively settled is whether the transplanted stem cells may give rise to tumors — a risk that is ever-present any time stem cells are used. More research is required to assess the long-term safety and effectiveness of these treatments.
Given the lack of uniform industry standards, one can easily end up at a clinic that overpromises what it can deliver.
In the journal Plastic Reconstruction Surgery in 2014, Adrian McArdle and a team of Stanford University plastic surgeons examined the common claims of CAL's "stem cell facelifts" being offered by clinics across the world. McArdle and his team write: "…the marketplace is characterized by direct-to-consumer corporate medicine strategies that are characterized by unsubstantiated, and sometimes fraudulent claims, that put our patients at risk." Given the lack of uniform industry standards, one can easily end up at a clinic that overpromises what it can deliver.
But according to McArdle, further research on CAL, including clinical trials, is proceeding apace. It's possible that as more research on the potential of stem cells accrues, many of the technical hurdles will be crossed.
If you decide to try CAL in a research or clinical setting, be forewarned. You will be taking part in a young science, with many unknown questions. However, the next time someone offers to sell you stem cells in a jar, you'll know what you're paying for.
Researchers claimed they built a breakthrough superconductor. Social media shot it down almost instantly.
In July, South Korean scientists posted a paper finding they had achieved superconductivity - a claim that was debunked within days.
Harsh Mathur was a graduate physics student at Yale University in late 1989 when faculty announced they had failed to replicate claims made by scientists at the University of Utah and the University of Wolverhampton in England.
Such work is routine. Replicating or attempting to replicate the contraptions, calculations and conclusions crafted by colleagues is foundational to the scientific method. But in this instance, Yale’s findings were reported globally.
“I had a ringside view, and it was crazy,” recalls Mathur, now a professor of physics at Case Western Reserve University in Ohio.
Yale’s findings drew so much attention because initial experiments by Stanley Pons of Utah and Martin Fleischmann of Wolverhampton led to a startling claim: They were able to fuse atoms at room temperature – a scientific El Dorado known as “cold fusion.”
Nuclear fusion powers the stars in the universe. However, star cores must be at least 23.4 million degrees Fahrenheit and under extraordinary pressure to achieve fusion. Pons and Fleischmann claimed they had created an almost limitless source of power achievable at any temperature.
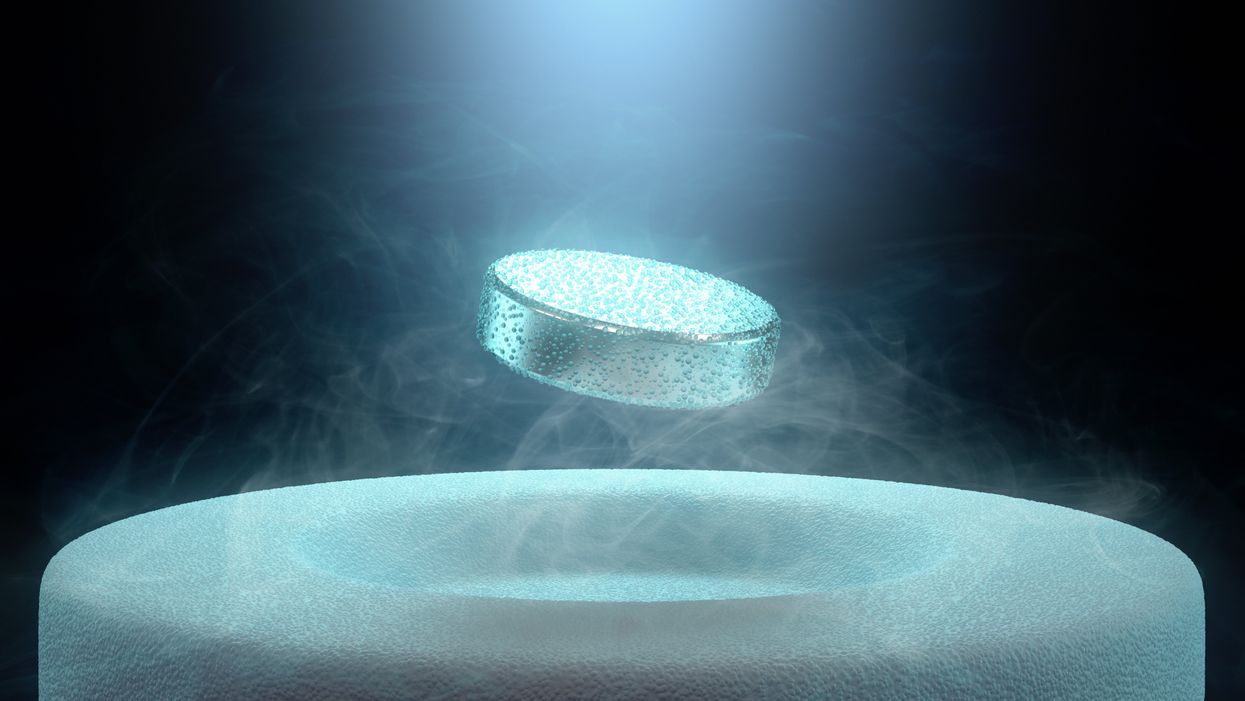
Like fusion, superconductivity can only be achieved in mostly impractical circumstances.
But about six months after they made their startling announcement, the pair’s findings were discredited by researchers at Yale and the California Institute of Technology. It was one of the first instances of a major scientific debunking covered by mass media.
Some scholars say the media attention for cold fusion stemmed partly from a dazzling announcement made three years prior in 1986: Scientists had created the first “superconductor” – material that could transmit electrical current with little or no resistance. It drew global headlines – and whetted the public’s appetite for announcements of scientific breakthroughs that could cause economic transformations.
But like fusion, superconductivity can only be achieved in mostly impractical circumstances: It must operate either at temperatures of at least negative 100 degrees Fahrenheit, or under pressures of around 150,000 pounds per square inch. Superconductivity that functions in closer to a normal environment would cut energy costs dramatically while also opening infinite possibilities for computing, space travel and other applications.
In July, a group of South Korean scientists posted material claiming they had created an iron crystalline substance called LK-99 that could achieve superconductivity at slightly above room temperature and at ambient pressure. The group partners with the Quantum Energy Research Centre, a privately-held enterprise in Seoul, and their claims drew global headlines.
Their work was also debunked. But in the age of internet and social media, the process was compressed from half-a-year into days. And it did not require researchers at world-class universities.
One of the most compelling critiques came from Derrick VanGennep. Although he works in finance, he holds a Ph.D. in physics and held a postdoctoral position at Harvard. The South Korean researchers had posted a video of a nugget of LK-99 in what they claimed was the throes of the Meissner effect – an expulsion of the substance’s magnetic field that would cause it to levitate above a magnet. Unless Hollywood magic is involved, only superconducting material can hover in this manner.
That claim made VanGennep skeptical, particularly since LK-99’s levitation appeared unenthusiastic at best. In fact, a corner of the material still adhered to the magnet near its center. He thought the video demonstrated ferromagnetism – two magnets repulsing one another. He mixed powdered graphite with super glue, stuck iron filings to its surface and mimicked the behavior of LK-99 in his own video, which was posted alongside the researchers’ video.
VanGennep believes the boldness of the South Korean claim was what led to him and others in the scientific community questioning it so quickly.
“The swift replication attempts stemmed from the combination of the extreme claim, the fact that the synthesis for this material is very straightforward and fast, and the amount of attention that this story was getting on social media,” he says.
But practicing scientists were suspicious of the data as well. Michael Norman, director of the Argonne Quantum Institute at the Argonne National Laboratory just outside of Chicago, had doubts immediately.
Will this saga hurt or even affect the careers of the South Korean researchers? Possibly not, if the previous fusion example is any indication.
“It wasn’t a very polished paper,” Norman says of the Korean scientists’ work. That opinion was reinforced, he adds, when it turned out the paper had been posted online by one of the researchers prior to seeking publication in a peer-reviewed journal. Although Norman and Mathur say that is routine with scientific research these days, Norman notes it was posted by one of the junior researchers over the doubts of two more senior scientists on the project.
Norman also raises doubts about the data reported. Among other issues, he observes that the samples created by the South Korean researchers contained traces of copper sulfide that could inadvertently amplify findings of conductivity.
The lack of the Meissner effect also caught Mathur’s attention. “Ferromagnets tend to be unstable when they levitate,” he says, adding that the video “just made me feel unconvinced. And it made me feel like they hadn't made a very good case for themselves.”
Will this saga hurt or even affect the careers of the South Korean researchers? Possibly not, if the previous fusion example is any indication. Despite being debunked, cold fusion claimants Pons and Fleischmann didn’t disappear. They moved their research to automaker Toyota’s IMRA laboratory in France, which along with the Japanese government spent tens of millions of dollars on their work before finally pulling the plug in 1998.
Fusion has since been created in laboratories, but being unable to reproduce the density of a star’s core would require excruciatingly high temperatures to achieve – about 160 million degrees Fahrenheit. A recently released Government Accountability Office report concludes practical fusion likely remains at least decades away.
However, like Pons and Fleischman, the South Korean researchers are not going anywhere. They claim that LK-99’s Meissner effect is being obscured by the fact the substance is both ferromagnetic and diamagnetic. They have filed for a patent in their country. But for now, those claims remain chimerical.
In the meantime, the consensus as to when a room temperature superconductor will be achieved is mixed. VenGennep – who studied the issue during his graduate and postgraduate work – puts the chance of creating such a superconductor by 2050 at perhaps 50-50. Mathur believes it could happen sooner, but adds that research on the topic has been going on for nearly a century, and that it has seen many plateaus.
“There's always this possibility that there's going to be something out there that we're going to discover unexpectedly,” Norman notes. The only certainty in this age of social media is that it will be put through the rigors of replication instantly.
Scientists implant brain cells to counter Parkinson's disease
In a recent research trial, patients with Parkinson's disease reported that their symptoms had improved after stem cells were implanted into their brains. Martin Taylor, far right, was diagnosed at age 32.
Martin Taylor was only 32 when he was diagnosed with Parkinson's, a disease that causes tremors, stiff muscles and slow physical movement - symptoms that steadily get worse as time goes on.
“It's horrible having Parkinson's,” says Taylor, a data analyst, now 41. “It limits my ability to be the dad and husband that I want to be in many cruel and debilitating ways.”
Today, more than 10 million people worldwide live with Parkinson's. Most are diagnosed when they're considerably older than Taylor, after age 60. Although recent research has called into question certain aspects of the disease’s origins, Parkinson’s eventually kills the nerve cells in the brain that produce dopamine, a signaling chemical that carries messages around the body to control movement. Many patients have lost 60 to 80 percent of these cells by the time they are diagnosed.
For years, there's been little improvement in the standard treatment. Patients are typically given the drug levodopa, a chemical that's absorbed by the brain’s nerve cells, or neurons, and converted into dopamine. This drug addresses the symptoms but has no impact on the course of the disease as patients continue to lose dopamine producing neurons. Eventually, the treatment stops working effectively.
BlueRock Therapeutics, a cell therapy company based in Massachusetts, is taking a different approach by focusing on the use of stem cells, which can divide into and generate new specialized cells. The company makes the dopamine-producing cells that patients have lost and inserts these cells into patients' brains. “We have a disease with a high unmet need,” says Ahmed Enayetallah, the senior vice president and head of development at BlueRock. “We know [which] cells…are lost to the disease, and we can make them. So it really came together to use stem cells in Parkinson's.”
In a phase 1 research trial announced late last month, patients reported that their symptoms had improved after a year of treatment. Brain scans also showed an increased number of neurons generating dopamine in patients’ brains.
Increases in dopamine signals
The recent phase 1 trial focused on deploying BlueRock’s cell therapy, called bemdaneprocel, to treat 12 patients suffering from Parkinson’s. The team developed the new nerve cells and implanted them into specific locations on each side of the patient's brain through two small holes in the skull made by a neurosurgeon. “We implant cells into the places in the brain where we think they have the potential to reform the neural networks that are lost to Parkinson's disease,” Enayetallah says. The goal is to restore motor function to patients over the long-term.
Five patients were given a relatively low dose of cells while seven got higher doses. Specialized brain scans showed evidence that the transplanted cells had survived, increasing the overall number of dopamine producing cells. The team compared the baseline number of these cells before surgery to the levels one year later. “The scans tell us there is evidence of increased dopamine signals in the part of the brain affected by Parkinson's,” Enayetallah says. “Normally you’d expect the signal to go down in untreated Parkinson’s patients.”
"I think it has a real chance to reverse motor symptoms, essentially replacing a missing part," says Tilo Kunath, a professor of regenerative neurobiology at the University of Edinburgh.
The team also asked patients to use a specific type of home diary to log the times when symptoms were well controlled and when they prevented normal activity. After a year of treatment, patients taking the higher dose reported symptoms were under control for an average of 2.16 hours per day above their baselines. At the smaller dose, these improvements were significantly lower, 0.72 hours per day. The higher-dose patients reported a corresponding decrease in the amount of time when symptoms were uncontrolled, by an average of 1.91 hours, compared to 0.75 hours for the lower dose. The trial was safe, and patients tolerated the year of immunosuppression needed to make sure their bodies could handle the foreign cells.
Claire Bale, the associate director of research at Parkinson's U.K., sees the promise of BlueRock's approach, while noting the need for more research on a possible placebo effect. The trial participants knew they were getting the active treatment, and placebo effects are known to be a potential factor in Parkinson’s research. Even so, “The results indicate that this therapy produces improvements in symptoms for Parkinson's, which is very encouraging,” Bale says.
Tilo Kunath, a professor of regenerative neurobiology at the University of Edinburgh, also finds the results intriguing. “I think it's excellent,” he says. “I think it has a real chance to reverse motor symptoms, essentially replacing a missing part.” However, it could take time for this therapy to become widely available, Kunath says, and patients in the late stages of the disease may not benefit as much. “Data from cell transplantation with fetal tissue in the 1980s and 90s show that cells did not survive well and release dopamine in these [late-stage] patients.”
Searching for the right approach
There's a long history of using cell therapy as a treatment for Parkinson's. About four decades ago, scientists at the University of Lund in Sweden developed a method in which they transferred parts of fetal brain tissue to patients with Parkinson's so that their nerve cells would produce dopamine. Many benefited, and some were able to stop their medication. However, the use of fetal tissue was highly controversial at that time, and the tissues were difficult to obtain. Later trials in the U.S. showed that people benefited only if a significant amount of the tissue was used, and several patients experienced side effects. Eventually, the work lost momentum.
“Like many in the community, I'm aware of the long history of cell therapy,” says Taylor, the patient living with Parkinson's. “They've long had that cure over the horizon.”
In 2000, Lorenz Studer led a team at the Memorial Sloan Kettering Centre, in New York, to find the chemical signals needed to get stem cells to differentiate into cells that release dopamine. Back then, the team managed to make cells that produced some dopamine, but they led to only limited improvements in animals. About a decade later, in 2011, Studer and his team found the specific signals needed to guide embryonic cells to become the right kind of dopamine producing cells. Their experiments in mice, rats and monkeys showed that their implanted cells had a significant impact, restoring lost movement.
Studer then co-founded BlueRock Therapeutics in 2016. Forming the most effective stem cells has been one of the biggest challenges, says Enayetallah, the BlueRock VP. “It's taken a lot of effort and investment to manufacture and make the cells at the right scale under the right conditions.” The team is now using cells that were first isolated in 1998 at the University of Wisconsin, a major advantage because they’re available in a virtually unlimited supply.
Other efforts underway
In the past several years, University of Lund researchers have begun to collaborate with the University of Cambridge on a project to use embryonic stem cells, similar to BlueRock’s approach. They began clinical trials this year.
A company in Japan called Sumitomo is using a different strategy; instead of stem cells from embryos, they’re reprogramming adults' blood or skin cells into induced pluripotent stem cells - meaning they can turn into any cell type - and then directing them into dopamine producing neurons. Although Sumitomo started clinical trials earlier than BlueRock, they haven’t yet revealed any results.
“It's a rapidly evolving field,” says Emma Lane, a pharmacologist at the University of Cardiff who researches clinical interventions for Parkinson’s. “But BlueRock’s trial is the first full phase 1 trial to report such positive findings with stem cell based therapies.” The company’s upcoming phase 2 research will be critical to show how effectively the therapy can improve disease symptoms, she added.
The cure over the horizon
BlueRock will continue to look at data from patients in the phase 1 trial to monitor the treatment’s effects over a two-year period. Meanwhile, the team is planning the phase 2 trial with more participants, including a placebo group.
For patients with Parkinson’s like Martin Taylor, the therapy offers some hope, though Taylor recognizes that more research is needed.

BlueRock Therapeutics
“Like many in the community, I'm aware of the long history of cell therapy,” he says. “They've long had that cure over the horizon.” His expectations are somewhat guarded, he says, but, “it's certainly positive to see…movement in the field again.”
"If we can demonstrate what we’re seeing today in a more robust study, that would be great,” Enayetallah says. “At the end of the day, we want to address that unmet need in a field that's been waiting for a long time.”
Editor's note: The company featured in this piece, BlueRock Therapeutics, is a portfolio company of Leaps by Bayer, which is a sponsor of Leaps.org. BlueRock was acquired by Bayer Pharmaceuticals in 2019. Leaps by Bayer and other sponsors have never exerted influence over Leaps.org content or contributors.