The Real Science Behind “Anti-Aging” Beauty Products

The beauty industry heavily hypes the nascent promise of stem cells for rejuvenation.
The beauty market abounds with high-end creams and serums that claim the use of stem cells to rejuvenate aging skin.
Selling on the internet and at department stores like Nordstrom, these products promise "breakthrough" applications to plump, smooth, and "reverse visible signs of aging," and at least one product offers to create a "regenerative firming serum, moisturizer, and eye cream" from customers' own stem cells – for a whopping $1200.
The beauty industry is heavily hyping glimmers of the nascent field of stem cell therapy.
Steeped in clinical-sounding terms like "proteins and peptides from pluripotent stem cells," the marketing of these products evokes a dramatic restoration of youthfulness based on cutting-edge science. But the beauty industry is heavily hyping glimmers of the nascent field of stem cell therapy. So what is real and what's not? And is there in fact a way to harness the potential of stem cells in the service of beauty?
Plant vs. Human Stem Cells
Stem cells do indeed have tremendous promise for treating a wide range of diseases and conditions. The cells come from early-stage embryos or, more commonly, from umbilical cord blood or our own bodies. Embryonic stem cells are considered the body's "master" cells because they can develop into any of our several hundred cell types. Adult stem cells, on the other hand, reside in mature tissues and organs like the brain, bone marrow, and skin, and their versatility is more limited. As an internal repair system for many tissue types, they replenish sick, injured, and worn-out cells.
Nowadays, with some sophisticated chemical coaxing, adult stem cells can be returned to an embryonic-like blank state, with the ability to become any cell type that the body might need.
Beauty product manufacturers convey in their advertising that the rejuvenating power of these cells could hold the key to the fountain of youth. But there's something the manufacturers don't always tell you: their products do not typically use human stem cells.
"The whole concept of stem cells is intriguing to the public," says Tamara Griffiths, a consultant dermatologist for the British Skin Foundation. "But what these products contain is plant stem cells and, more commonly, chemicals that have been derived from plant stem cells."
The plant stem cells are cultured in the lab with special media to get them to produce signaling proteins and peptides, like cytokines and chemokines. These have been shown to be good for reducing inflammation and promoting healthy cell functioning, even if derived from plants. However, according to Griffiths, there are so many active ingredients in these products that it's hard to say just what role each one of them plays. We do know that their ability to replenish human stem cells is extremely limited, and the effects of plant stem cells on human cells are unproven.
"...any cosmetic that is advertised to be anti-aging due to plant stem cells at this time is about as effective as all the skin creams without stem cells."
Whether products containing plant cell-derived ingredients work better than conventional skin products is unknown because these products are not regulated by the U.S. Food and Drug Administration and may rest on dubious, even more or less nonexistent, research. Cosmetics companies have conducted most of the research and the exact formulas they devise are considered proprietary information. They have no incentive to publish their research findings, and they don't have to meet standards imposed by the FDA unless they start using human cells in their products.
"There are biological limits to what you can do with plant cells in the first place," says Griffiths. "No plant stem cell is going to morph into a human skin cell no matter what magic medium you immerse it in. Nor is a plant cell likely to stimulate the production of human stem cells if applied to the skin."
According to Sarah Baucus, a cell biologist, for any type of stem cell to be of any use whatsoever, the cells must be alive. The processing needed to incorporate living cells into any type of cream or serum would inevitably kill them, rendering them useless. The splashy marketing of these products suggests that results may be drastic, but none of these creams is likely to produce the kind of rejuvenating effect that would be on par with a facelift or several other surgical or dermatological procedures.
"Plant stem cell therapy needs to move in the right direction to implement its inherent potential in skin care," researchers wrote in a 2017 paper in the journal Future Science OA. "This might happen in the next 20 years but any cosmetic that is advertised to be anti-aging due to plant stem cells at this time is about as effective as all the skin creams without stem cells."
From Beauty Counter to Doctor's Clinic
Where do you turn if you still want to harness the power of stem cells to reinvigorate the skin? Is there a legitimate treatment using human cells? The answer is possibly, but for that you have to switch from the Nordstrom cosmetics counter to a clinic with a lab, where plastic surgeons work with specialists who culture and manipulate living cells.
Plastic surgeons are experts in wound healing, a process in which stem cells play a prominent role. Doctors have long used the technique of taking fat from the body and injecting it into hollowed-out or depressed areas of the face to fill in injuries, correct wrinkles, and improve the face's curvature. Lipotransfer, or the harvesting of body fat and injecting it into the face, has been around for many years in traditional plastic surgery clinics. In recent years, some plastic surgeons have started to cull stem cells from fat. One procedure that does just that is called cell-assisted lipotransfer, or CAL.
In CAL, adipose tissue, or fat, is harvested by liposuction, usually from the lower abdomen. Fat contains stem cells that can differentiate into several cell types, including skin, muscle, cartilage, and bone. Fat tissue has an especially stem cell-rich layer. These cells are then mixed with some regular fat, making in effect a very stem cell-rich fat solution, right in the doctor's office. The process of manipulating the fat cells takes about 90 to 110 minutes, and then the solution is ready to be injected into the skin, to fill in the lips, the cheeks, and the nasolabial folds, or the deep folds around the nose and mouth.
Unlike regular fat, which is often injected into the face, some experts claim that the cell-enriched fat has better, longer-lasting results. The tissue graft grows its own blood vessels, an advantage that may lead to a more long-lasting graft – though the research is mixed, with some studies showing they do and other studies showing the complete opposite.
For almost all stem cell products on the market today in the U.S., it is not yet known whether they are safe or effective, despite how they are marketed.
One of the pioneers in CAL, a plastic surgeon in Brazil named Dr. Aris Sterodimas, says that the stem cells secrete growth factors that rejuvenate the skin -- like the plant stem cells that are used in topical creams and serums. Except that these cells are human stem cells and hence have inherently more potential in the human body.
Note that CAL doesn't actually result in large numbers of fresh, new replacement cells, as might be imagined. It's simply fat tissue treated to make it richer in stem cells, to have more of the growth-inducing proteins and peptides delivered to the dermis layer of the skin.
Sterodimas works alongside a tissue engineer to provide CAL in his clinic. He uses it as a way to rebuild soft tissues in people disfigured by accidents or diseases, or who are suffering the after-effects of radiation treatments for cancer.
Plastic surgeons get plenty of these patients. But how widespread is CAL for beauty purposes? Sterodimas says that he regularly performs the procedure for Brazilians, and it's widely available in Europe and Japan. In the U.S., the procedure hasn't taken off because there is no FDA approval for the various methods used by different doctors and clinics. A few major academic centers in the U.S. offer the treatment on a clinical trials basis and there are several trials ongoing.
But there is a downside to all lipotransfers: the transplanted fat will eventually be absorbed by the body. Even the cell-enriched fat has a limited lifespan before reabsorption. That means if you like the cosmetic results of CAL, you'll have to repeat the treatment about every two years to maintain the plumping, firming, and smoothing effects on the skin. The results of CAL are "superior to the results of laser treatments and other plastic surgery interventions, though the effect is not as dramatic as a facelift," says Sterodimas.
Buyer Beware
For almost all stem cell products on the market today in the U.S., it is not yet known whether they are safe or effective, despite how they are marketed. There are around 700 clinics in the U.S. offering stem cell treatments and up to 20,000 people have received these therapies. However, the only FDA-approved stem cell treatments use cells from bone marrow or cord blood to treat cancers of the blood and bone marrow. Safety concerns have prompted the FDA to announce increased oversight of stem cell clinics.
As for CAL, most of the clinical trials so far have been focused on using it for breast reconstruction after mastectomy, and results are mixed. Experts warn that the procedure has yet to be proven safe as well as effective. It's important to remember that this newborn science is in the early stages of research.
One question that has also not been definitively settled is whether the transplanted stem cells may give rise to tumors — a risk that is ever-present any time stem cells are used. More research is required to assess the long-term safety and effectiveness of these treatments.
Given the lack of uniform industry standards, one can easily end up at a clinic that overpromises what it can deliver.
In the journal Plastic Reconstruction Surgery in 2014, Adrian McArdle and a team of Stanford University plastic surgeons examined the common claims of CAL's "stem cell facelifts" being offered by clinics across the world. McArdle and his team write: "…the marketplace is characterized by direct-to-consumer corporate medicine strategies that are characterized by unsubstantiated, and sometimes fraudulent claims, that put our patients at risk." Given the lack of uniform industry standards, one can easily end up at a clinic that overpromises what it can deliver.
But according to McArdle, further research on CAL, including clinical trials, is proceeding apace. It's possible that as more research on the potential of stem cells accrues, many of the technical hurdles will be crossed.
If you decide to try CAL in a research or clinical setting, be forewarned. You will be taking part in a young science, with many unknown questions. However, the next time someone offers to sell you stem cells in a jar, you'll know what you're paying for.
Scientists have known about and studied heart rate variability, or HRV, for a long time and, in recent years, monitors have come to market that can measure HRV accurately.
This episode is about a health metric you may not have heard of before: heart rate variability, or HRV. This refers to the small changes in the length of time between each of your heart beats.
Scientists have known about and studied HRV for a long time. In recent years, though, new monitors have come to market that can measure HRV accurately whenever you want.
Five months ago, I got interested in HRV as a more scientific approach to finding the lifestyle changes that work best for me as an individual. It's at the convergence of some important trends in health right now, such as health tech, precision health and the holistic approach in systems biology, which recognizes how interactions among different parts of the body are key to health.
But HRV is just one of many numbers worth paying attention to. For this episode of Making Sense of Science, I spoke with psychologist Dr. Leah Lagos; Dr. Jessilyn Dunn, assistant professor in biomedical engineering at Duke; and Jason Moore, the CEO of Spren and an app called Elite HRV. We talked about what HRV is, research on its benefits, how to measure it, whether it can be used to make improvements in health, and what researchers still need to learn about HRV.
*Talk to your doctor before trying anything discussed in this episode related to HRV and lifestyle changes to raise it.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Show notes
Spren - https://www.spren.com/
Elite HRV - https://elitehrv.com/
Jason Moore's Twitter - https://twitter.com/jasonmooreme?lang=en
Dr. Jessilyn Dunn's Twitter - https://twitter.com/drjessilyn?lang=en
Dr. Dunn's study on HRV, flu and common cold - https://jamanetwork.com/journals/jamanetworkopen/f...
Dr. Leah Lagos - https://drleahlagos.com/
Dr. Lagos on Star Talk - https://www.youtube.com/watch?v=jC2Q10SonV8
Research on HRV and intermittent fasting - https://pubmed.ncbi.nlm.nih.gov/33859841/
Research on HRV and Mediterranean diet - https://medicalxpress.com/news/2010-06-twin-medite...:~:text=Using%20data%20from%20the%20Emory,eating%20a%20Western%2Dtype%20diet
Devices for HRV biofeedback - https://elitehrv.com/heart-variability-monitors-an...
Benefits of HRV biofeedback - https://pubmed.ncbi.nlm.nih.gov/32385728/
HRV and cognitive performance - https://www.frontiersin.org/articles/10.3389/fnins...
HRV and emotional regulation - https://pubmed.ncbi.nlm.nih.gov/36030986/
Fortune article on HRV - https://fortune.com/well/2022/12/26/heart-rate-var...
Peanut allergies affect about a million children in the U.S., and most never outgrow them. Luckily, some promising remedies are in the works.
Ever since he was a baby, Sharon Wong’s son Brandon suffered from rashes, prolonged respiratory issues and vomiting. In 2006, as a young child, he was diagnosed with a severe peanut allergy.
"My son had a history of reacting to traces of peanuts in the air or in food,” says Wong, a food allergy advocate who runs a blog focusing on nut free recipes, cooking techniques and food allergy awareness. “Any participation in school activities, social events, or travel with his peanut allergy required a lot of preparation.”
Peanut allergies affect around a million children in the U.S. Most never outgrow the condition. The problem occurs when the immune system mistakenly views the proteins in peanuts as a threat and releases chemicals to counteract it. This can lead to digestive problems, hives and shortness of breath. For some, like Wong’s son, even exposure to trace amounts of peanuts could be life threatening. They go into anaphylactic shock and need to take a shot of adrenaline as soon as possible.
Typically, people with peanut allergies try to completely avoid them and carry an adrenaline autoinjector like an EpiPen in case of emergencies. This constant vigilance is very stressful, particularly for parents with young children.
“The search for a peanut allergy ‘cure’ has been a vigorous one,” says Claudia Gray, a pediatrician and allergist at Vincent Pallotti Hospital in Cape Town, South Africa. The closest thing to a solution so far, she says, is the process of desensitization, which exposes the patient to gradually increasing doses of peanut allergen to build up a tolerance. The most common type of desensitization is oral immunotherapy, where patients ingest small quantities of peanut powder. It has been effective but there is a risk of anaphylaxis since it involves swallowing the allergen.
"By the end of the trial, my son tolerated approximately 1.5 peanuts," Sharon Wong says.
DBV Technologies, a company based in Montrouge, France has created a skin patch to address this problem. The Viaskin Patch contains a much lower amount of peanut allergen than oral immunotherapy and delivers it through the skin to slowly increase tolerance. This decreases the risk of anaphylaxis.
Wong heard about the peanut patch and wanted her son to take part in an early phase 2 trial for 4-to-11-year-olds.
“We felt that participating in DBV’s peanut patch trial would give him the best chance at desensitization or at least increase his tolerance from a speck of peanut to a peanut,” Wong says. “The daily routine was quite simple, remove the old patch and then apply a new one. By the end of the trial, he tolerated approximately 1.5 peanuts.”
How it works
For DBV Technologies, it all began when pediatric gastroenterologist Pierre-Henri Benhamou teamed up with fellow professor of gastroenterology Christopher Dupont and his brother, engineer Bertrand Dupont. Together they created a more effective skin patch to detect when babies have allergies to cow's milk. Then they realized that the patch could actually be used to treat allergies by promoting tolerance. They decided to focus on peanut allergies first as the more dangerous.
The Viaskin patch utilizes the fact that the skin can promote tolerance to external stimuli. The skin is the body’s first defense. Controlling the extent of the immune response is crucial for the skin. So it has defense mechanisms against external stimuli and can promote tolerance.
The patch consists of an adhesive foam ring with a plastic film on top. A small amount of peanut protein is placed in the center. The adhesive ring is attached to the back of the patient's body. The peanut protein sits above the skin but does not directly touch it. As the patient sweats, water droplets on the inside of the film dissolve the peanut protein, which is then absorbed into the skin.
The peanut protein is then captured by skin cells called Langerhans cells. They play an important role in getting the immune system to tolerate certain external stimuli. Langerhans cells take the peanut protein to lymph nodes which activate T regulatory cells. T regulatory cells suppress the allergic response.
A different patch is applied to the skin every day to increase tolerance. It’s both easy to use and convenient.
“The DBV approach uses much smaller amounts than oral immunotherapy and works through the skin significantly reducing the risk of allergic reactions,” says Edwin H. Kim, the division chief of Pediatric Allergy and Immunology at the University of North Carolina, U.S., and one of the principal investigators of Viaskin’s clinical trials. “By not going through the mouth, the patch also avoids the taste and texture issues. Finally, the ability to apply a patch and immediately go about your day may be very attractive to very busy patients and families.”
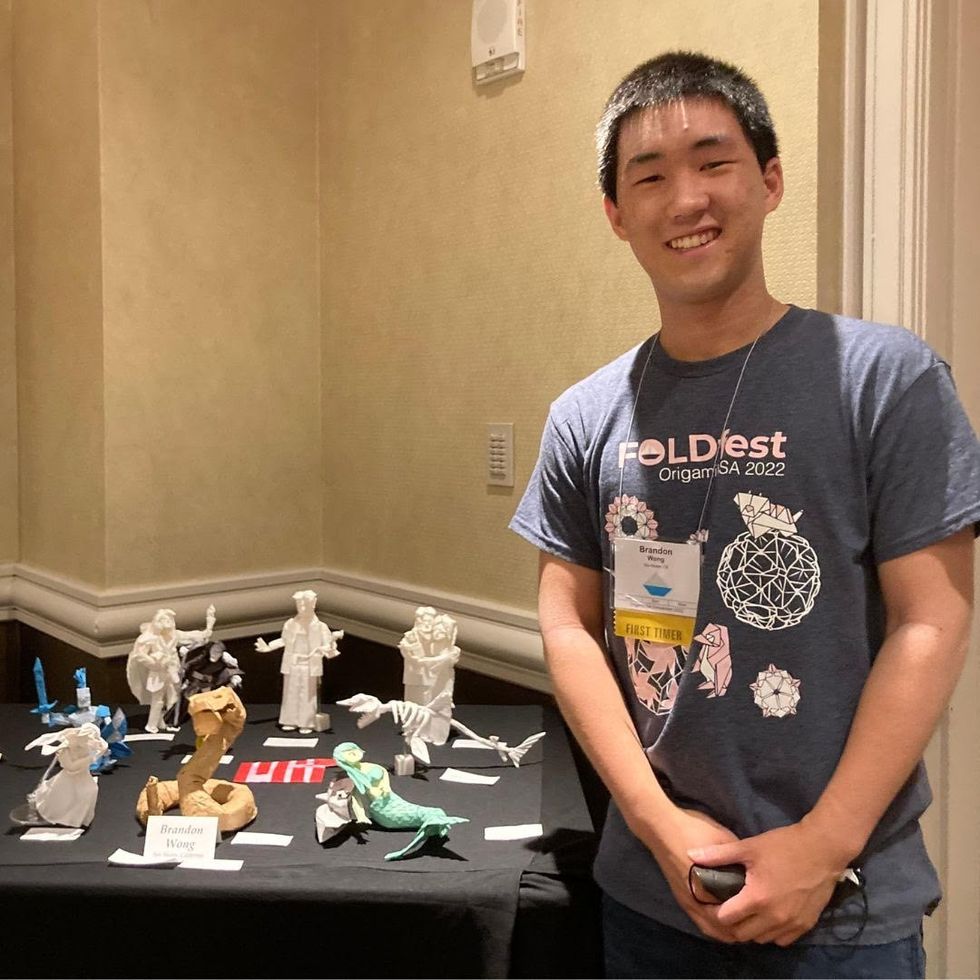
Brandon Wong displaying origami figures he folded at an Origami Convention in 2022
Sharon Wong
Clinical trials
Results from DBV's phase 3 trial in children ages 1 to 3 show its potential. For a positive result, patients who could not tolerate 10 milligrams or less of peanut protein had to be able to manage 300 mg or more after 12 months. Toddlers who could already tolerate more than 10 mg needed to be able to manage 1000 mg or more. In the end, 67 percent of subjects using the Viaskin patch met the target as compared to 33 percent of patients taking the placebo dose.
“The Viaskin peanut patch has been studied in several clinical trials to date with promising results,” says Suzanne M. Barshow, assistant professor of medicine in allergy and asthma research at Stanford University School of Medicine in the U.S. “The data shows that it is safe and well-tolerated. Compared to oral immunotherapy, treatment with the patch results in fewer side effects but appears to be less effective in achieving desensitization.”
The primary reason the patch is less potent is that oral immunotherapy uses a larger amount of the allergen. Additionally, absorption of the peanut protein into the skin could be erratic.
Gray also highlights that there is some tradeoff between risk and efficacy.
“The peanut patch is an exciting advance but not as effective as the oral route,” Gray says. “For those patients who are very sensitive to orally ingested peanut in oral immunotherapy or have an aversion to oral peanut, it has a use. So, essentially, the form of immunotherapy will have to be tailored to each patient.” Having different forms such as the Viaskin patch which is applied to the skin or pills that patients can swallow or dissolve under the tongue is helpful.
The hope is that the patch’s efficacy will increase over time. The team is currently running a follow-up trial, where the same patients continue using the patch.
“It is a very important study to show whether the benefit achieved after 12 months on the patch stays stable or hopefully continues to grow with longer duration,” says Kim, who is an investigator in this follow-up trial.
"My son now attends university in Massachusetts, lives on-campus, and eats dorm food. He has so much more freedom," Wong says.
The team is further ahead in the phase 3 follow-up trial for 4-to-11-year-olds. The initial phase 3 trial was not as successful as the trial for kids between one and three. The patch enabled patients to tolerate more peanuts but there was not a significant enough difference compared to the placebo group to be definitive. The follow-up trial showed greater potency. It suggests that the longer patients are on the patch, the stronger its effects.
They’re also testing if making the patch bigger, changing the shape and extending the minimum time it’s worn can improve its benefits in a trial for a new group of 4-to-11 year-olds.
The future
DBV Technologies is using the skin patch to treat cow’s milk allergies in children ages 1 to 17. They’re currently in phase 2 trials.
As for the peanut allergy trials in toddlers, the hope is to see more efficacy soon.
For Wong’s son who took part in the earlier phase 2 trial for 4-to-11-year-olds, the patch has transformed his life.
“My son continues to maintain his peanut tolerance and is not affected by peanut dust in the air or cross-contact,” Wong says. ”He attends university in Massachusetts, lives on-campus, and eats dorm food. He still carries an EpiPen but has so much more freedom than before his clinical trial. We will always be grateful.”

