The Science Sleuth Holding Fraudulent Research Accountable
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

Outside whistleblower Elisabeth Bik scrutinizes newly published scientific papers for misleading images and data.
Introduction by Mary Inman, Whistleblower Attorney
For most people, when they see the word "whistleblower," the image that leaps to mind is a lone individual bravely stepping forward to shine a light on misconduct she has witnessed first-hand. Meryl Streep as Karen Silkwood exposing safety violations observed while working the line at the Kerr-McGee plutonium plant. Matt Damon as Mark Whitacre in The Informant!, capturing on his pocket recorder clandestine meetings between his employer and its competitors to fix the price of lysine. However, a new breed of whistleblower is emerging who isn't at the scene of the crime but instead figures it out after the fact through laborious review of publicly available information and expert analysis. Elisabeth Bik belongs to this new class of whistleblower.
"There's this delicate balance where on one hand we want to spread results really fast as scientists, but on the other hand, we know it's incomplete, it's rushed and it's not great."
Using her expertise as a microbiologist and her trained eye, Bik studies publicly available scientific papers to sniff out potential irregularities in the images that suggest research fraud, later seeking retraction of the offending paper from the journal's publisher. There's no smoking gun, no first-hand account of any kind. Just countless hours spent reviewing scores of scientific papers and Bik's skills and dedication as a science fraud sleuth.
While Bik's story may not as readily lend itself to the big screen, her work is nonetheless equally heroic. By tirelessly combing scientific papers to expose research fraud, Bik is playing a vital role in holding the scientific publishing process accountable and ensuring that misleading information does not spread unchecked. This is important work in any age, but particularly so in the time of COVID, where we can ill afford the setbacks and delays of scientists building on false science. In the present climate, where science is politicized and scientific principles are under attack, strong voices like Bik's must rise above the din to ensure the scientific information we receive, and our governments act upon, is accurate. Our health and wellbeing depend on it.
Whistleblower outsiders like Bik are challenging the traditional concept of what it means to be a whistleblower. Fortunately for us, the whistleblower community is a broad church. As with most ecosystems, we all benefit from a diversity of voices —whistleblower insiders and outsiders alike. What follows is an illuminating conversation between Bik, and Ivan Oransky, the co-founder of Retraction Watch, an influential blog that reports on retractions of scientific papers and related topics. (Conversation facilitated by LeapsMag Editor-in-Chief Kira Peikoff)

Elisabeth Bik and Ivan Oransky.
(Photo credits Michel & Co Photography, San Jose, CA and Elizabeth Solaka)
Ivan
I'd like to hear your thoughts, Elisabeth, on an L.A. Times story, which was picking up a preprint about mutations and the novel coronavirus, alleging that the virus is mutating to become more infectious – even though this conclusion wasn't actually warranted.
Elisabeth
A lot of the news around it is picking up on one particular side of the story that is maybe not that much exaggerated by the scientists. I don't think this paper really showed that the mutations were causing the virus to be more virulent. Some of these viruses continuously mutate and mutate and mutate, and that doesn't necessarily make a strain more virulent. I think in many cases, a lot of people want to read something in a paper that is not actually there.
Ivan
The tone level, everything that's being published now, it's problematic. It's being rushed, here it wasn't even peer-reviewed. But even when they are peer-reviewed, they're being peer-reviewed by people who often aren't really an expert in that particular area.
Elisabeth
That's right.
Ivan
To me, it's all problematic. At the same time, it's all really good that it's all getting out there. I think that five or 10 years ago, or if we weren't in a pandemic, maybe that paper wouldn't have appeared at all. It would have maybe been submitted to a top-ranked journal and not have been accepted, or maybe it would have been improved during peer review and bounced down the ladder a bit to a lower-level journal.
Yet, now, because it's about coronavirus, it's in a major newspaper and, in fact, it's getting critiqued immediately.
Maybe it's too Pollyanna-ish, but I actually think that quick uploading is a good thing. The fear people have about preprint servers is based on this idea that the peer-reviewed literature is perfect. Once it is in a peer-reviewed journal, they think it must have gone through this incredible process. You're laughing because-
Elisabeth
I am laughing.
Ivan
You know it's not true.
Elisabeth
Yes, we both know that. I agree and I think in this particular situation, a pandemic that is unlike something our generation has seen before, there is a great, great need for fast dissemination of science.
If you have new findings, it is great that there is a thing called a preprint server where scientists can quickly share their results, with, of course, the caveat that it's not peer-reviewed yet.
It's unlike the traditional way of publishing papers, which can take months or years. Preprint publishing is a very fast way of spreading your results in a good way so that is what the world needs right now.
On the other hand, of course, there's the caveat that these are brand new results and a good scientist usually thinks about their results to really interpret it well. You have to look at it from all sides and I think with the rushed publication of preprint papers, there is no such thing as carefully thinking about what results might mean.
So there's this delicate balance where on one hand we want to spread results really fast as scientists, but on the other hand, we know it's incomplete, it's rushed and it's not great. This might be hard for the general audience to understand.
Ivan
I still think the benefits of that dissemination are more positive than negative.
Elisabeth
Right. But there's also so many papers that come out now on preprint servers and most of them are not that great, but there are some really good studies in there. It's hard to find those nuggets of really great papers. There's just a lot of papers that come out now.
Ivan
Well, you've made more than a habit of finding problems in papers. These are mostly, of course, until now published papers that you examined, but what is this time like for you? How is it different?
Elisabeth
It's different because in the beginning I looked at several COVID-19-related papers that came out and wrote some critiques about it. I did experience a lot of backlash because of that. So I felt I had to take a break from social media and from writing about COVID-19.
I focused a little bit more on other work because I just felt that a lot of these papers on COVID-19 became so politically divisive that if you tried to be a scientist and think critically about a paper, you were actually assigned to a particular political party or to be against other political parties. It's hard for me to be sucked into the political discussion and to the way that our society now is so completely divided into two camps that seem to be not listening to each other.
Ivan
I was curious about that because I've followed your work for a number of years, as you know, and certainly you have had critics before. I'm thinking of the case in China that you uncovered, the leading figure in the Chinese Academy who was really a powerful political figure in addition to being a scientist.
Elisabeth
So that was a case in which I found a couple of papers at first from a particular group in China, and I was just posting on a website called PubPeer, where you can post comments, concerns about papers. And in this case, these were image duplication issues, which is my specialty.
I did not realize that the group I was looking at at that moment was led by one of the highest ranked scientists in China. If I had known that, I would probably not have posted that under my full name, but under a pseudonym. Since I had already posted, some people were starting to send me direct messages on Twitter like, "OMG, the guy you're posting about now is the top scientist in China so you're going to have a lot of backlash."
Then I decided I'll just continue doing this. I found a total of around 50 papers from this group and posted all of them on PubPeer. That story quickly became a very popular story in China: number two on Sina Weibo, a social media site in China.
I was surprised it wasn't suppressed by the Chinese government, it was actually allowed by journalists that were writing about it, and I didn't experience a lot of backlash because of that.
Actually the Chinese doctor wrote me an email saying that he appreciated my feedback and that he would look into these cases. He sent a very polite email so I sent him back that I appreciated that he would look into these cases and left it there.
Ivan
There are certain subjects that I know when we write about them in Retraction Watch, they have tended in the past to really draw a lot of ire. I'm thinking anything about vaccines and autism, anything about climate change, stem cell research.
For a while that last subject has sort of died down. But now it's become a highly politically charged atmosphere. Do you feel that this pandemic has raised the profile of people such as yourself who we refer to as scientific sleuths, people who look critically and analytically at new research?
Elisabeth
Yeah, some people. But I'm also worried that some people who are great scientists and have shown a lot of critical thinking are being attacked because of that. If you just look at what happened to Dr. Fauci, I think that's a prime example. Where somebody who actually is very knowledgeable and very cautious of new science has not been widely accepted as a great leader, in our country at least. It's sad to see that. I'm just worried how long he will be at his position, to be honest.
Ivan
We noticed a big uptick in our traffic in the last few days to Retraction Watch and it turns out it was because someone we wrote about a number of years ago has really hopped on the bandwagon to try and discredit and even try to have Dr. Fauci fired.
It's one of these reminders that the way people think about scientists has, in many cases, far more to do with their own history or their own perspective going in than with any reality or anything about the science. It's pretty disturbing, but it's not a new thing. This has been happening for a while.
You can go back and read sociologists of science from 50-60 years ago and see the same thing, but I just don't think that it's in the same way that it is now, maybe in part because of social media.
Elisabeth
I've been personally very critical about several studies, but this is the first time I've experienced being attacked by trolls and having some nasty websites written about me. It is very disturbing to read.
"I don't think that something that's been peer-reviewed is perfect and something that hasn't been peer reviewed, you should never bother reading it."
Ivan
It is. Yet you have been a fearless and vocal critic of some very high-profile papers, like the infamous French study about hydroxychloroquine.
Elisabeth
Right, the paper that came out was immediately tweeted by the President of the United States. At first I thought it was great that our President tweeted about science! I thought that was a major breakthrough. I took a look at this paper.
It had just come out that day, I believe. The first thing I noticed is that it was accepted within 24 hours of being submitted to the journal. It was actually published in a journal where one of the authors is the editor-in-chief, which is a huge conflict of interest, but it happens.
But in this particular case, there were also a lot of flaws with the study and that, I think, should have been caught during peer review. The paper was first published on a preprint server and then within 24 hours or so it was published in that paper, supposedly after peer review.
There were very few changes between the preprint version and the peer review paper. There were just a couple of extra lines, extra sentences added here and there, but it wasn't really, I think, critically looked at. Because there were a lot of things that I thought were flaws.
Just to go over a couple of them. This paper showed supposedly that people who were treated with hydroxychloroquine and azithromycin were doing much better by clearing their virus much faster than people who were not treated with these drugs.
But if you look carefully at the paper there were a couple of people who were left out of the study. So they were treated with hydroxychloroquine, but they were not shown in the end results of the paper. All six people who were treated with the drug combination were clearing the virus within six days, but there were a couple of others who were left out of the study. They also started the drug combination, but they stopped taking the drugs for several reasons and three of them were admitted to the intensive care, one died, one had some side effects and one apparently walked out of the hospital.
They were left out of the study but they were actually not doing very well with the drug combination. It's not very good science if you leave out people who don't do very well with your drug combination in your study. That was one of my biggest critiques of the paper.
Ivan
What struck us about that case was, in addition to what you, of course, mentioned, the fact that Trump tweeted it and was talking about hydroxychloroquine, was that it seemed to be a perfect example of, "well, it was in a peer review journal." Yeah, it was a preprint first, but, well, it's a peer review journal. And yet, as you point out, when you look at the history of the paper, it was accepted in 24 hours.
If you talk to most scientists, the actual act of a peer review, once you sit down to do it and can concentrate, a good one takes, again, these are averages, but four hours, a half a day is not unreasonable. So you had to find three people who could suddenly review this paper. As you pointed out, it was in a journal where one of the authors was editor.
Then some strange things also happened, right? The society that actually publishes the journal, they came out with a statement saying this wasn't up to our standards, which is odd. Then Elsevier came in, they're the ones who are actually contracted to publish the journal for the society. They said, basically, "Oh, we're going to look into this now too."
It just makes you wonder what happened before the paper was actually published. All the people who were supposed to have been involved in doing the peer review or checking on it are clearly very distraught about what actually happened. It's that scene from Casablanca, "I'm shocked, shocked there's gambling going on here." And then, "Your winnings, sir."
Elisabeth
Yes.
Ivan
And I don't actually blame the public, I don't blame reporters for getting a bit confused about what it all means and what they should trust. I don't think trust is a binary any more than anything else is a binary. I don't think that something that's been peer-reviewed is perfect and something that hasn't been peer reviewed, you should never bother reading it. I think everything is much more gray.
Yet we've turned things into a binary. Even if you go back before coronavirus, coffee is good for you, coffee is bad for you, red wine, chocolate, all the rest of it. A lot of that is because of this sort of binary construct of the world for journalists, frankly, for scientists that need to get their next grants. And certainly for the general public, they want answers.
On the one hand, if I had to choose what group of experts, or what field of human endeavor would I trust with finding the answer to a pandemic like this, or to any crisis, it would absolutely be scientists. Hands down. This is coming from someone who writes about scientific fraud.
But on the other hand, that means that if scientists aren't clear about what they don't know and about the nuances and about what the scientific method actually allows us to do and learn, that just sets them up for failure. It sets people like Dr. Fauci up for failure.
Elisabeth
Right.
Ivan
It sets up any public health official who has a discussion about models. There's a famous saying: "All models are wrong, but some are useful."
Just because the projections change, it's not proof of wrongness, it's not proof that the model is fatally flawed. In fact, I'd be really concerned if the projections didn't change based on new information. I would love it if this whole episode did lead to a better understanding of the scientific process and how scientific publishing fits into that — and doesn't fit into it.
Elisabeth
Yes, I'm with you. I'm very worried that the general audience's perspective is based on maybe watching too many movies where the scientist comes up with a conclusion one hour into the movie when everything is about to fail. Like that scene in Contagion where somebody injects, I think, eight monkeys, and one of the monkeys survives and boom we have the vaccine. That's not really how science works. Everything takes many, many years and many, many applications where usually your first ideas and your first hypothesis turn out to be completely wrong.
Then you go back to the drawing board, you develop another hypothesis and this is a very reiterative process that usually takes years. Most of the people who watch the movie might have a very wrong idea and wrong expectations about how science works. We're living in the movie Contagion and by September, we'll all be vaccinated and we can go on and live our lives. But that's not what is going to happen. It's going to take much, much longer and we're going to have to change the models every time and change our expectations. Just because we don't know all the numbers and all the facts yet.
Ivan
Generally it takes a fairly long time to change medical practice. A lot of times people see that as a bad thing. What I think that ignores, or at least doesn't take into as much account as I would, is that you don't want doctors and other health care professionals to turn on a dime and suddenly switch. Unless, of course, it turns out there was no evidence for what you were looking at.
It's a complicated situation.
Everybody wants scientists to be engineers, right?
Elisabeth
Right.
Ivan
I'm not saying engineering isn't scientific, nor am I saying that science is just completely whimsical, but there's a different process. It's a different way of looking at things and you can't just throw all the data into a big supercomputer, which is what I think a lot of people seem to want us to do, and then the obvious answer will come out on the other side.
Elisabeth
No. It's true and a lot of engineers suddenly feel their inherent need to solve this as a problem. They're not scientists and it's not building a bridge over a big river. But we're dealing with something that is very hard to solve because we don't understand the problem yet. I think scientists are usually first analyzing the problem and trying to understand what the problem actually is before you can even think about a solution.
Ivan
I think we're still at the understanding the problem phase.
Elisabeth
Exactly. And going back to the French group paper, that promised such a result and that was interpreted as such by a lot of people including presidents, but it's a very rare thing to find a medication that will have a 100% curation rate. That's something that I wish the people would understand better. We all want that to happen, but it's very unlikely and very unprecedented in the best of times.
Ivan
I would second that and also say that the world needs to better value the work that people like Elisabeth and others are doing. Because we're not going to get to a better answer if we're not rigorous about scrutinizing the literature and scrutinizing the methodology and scrutinizing the results.
"I quit my job to be able to do this work."
It's a relatively new phenomenon that you're able to do this at any scale at all, and even now it's at a very small scale. Elisabeth mentioned PubPeer and I'm a big fan — also full disclosure, I'm on their board of directors as a volunteer — it's a very powerful engine for readers and journal editors and other scientists to discuss issues.
And Elisabeth has used it really, really well. I think we need to start giving credit to people like that. And, also creating incentives for that kind of work in a way that science hasn't yet.
Elisabeth
Yeah. I quit my job to be able to do this work. It's really hard to combine it with a job either in academia or industry because we're looking for or criticizing papers and it's hard when you are still employed to do that.
I try to make it about the papers and do it in a polite way, but still it's a very hard job to do if you have a daytime job and a position and a career to worry about. Because if you're critical of other academics, that could actually mean the end of your career and that's sad. They should be more open to polite criticism.
Ivan
And for the general public, if you're reading a newspaper story or something online about a single study and it doesn't mention any other studies that have said the same thing or similar, or frankly, if it doesn't say anything about any studies that contradicted it, that's probably also telling you something.
Say you're looking at a huge painting of a shoreline, a beach, and a forest. Any single study is just a one-centimeter-by-one-centimeter square of any part of that canvas. If you just look at that, you would either think it was a painting of the sea, of a beach, or of the forest. It's actually all three of those things.
We just need to be patient, and that's very challenging to us as human beings, but we need to take the time to look at the whole picture.
DISCLAIMER: Neither Elisabeth Bik nor Ivan Oransky was compensated for participation in The Pandemic Issue. While the magazine's editors suggested broad topics for discussion, consistent with Bik's and Oransky's work, neither they nor the magazine's underwriters had any influence on their conversation.
[Editor's Note: This article was originally published on June 8th, 2020 as part of a standalone magazine called GOOD10: The Pandemic Issue. Produced as a partnership among LeapsMag, The Aspen Institute, and GOOD, the magazine is available for free online.]
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Bobby Brooke Herrera, the co-founder and CEO of e25Bio, demonstrates the company's rapid paper-strip test for detecting the coronavirus.
You're lying in bed late at night, the foggy swirl of the pandemic's 8th month just beginning to fall behind you, when you detect a slight tickle at the back of your throat.
"If half of people choose to use these tests every other day, then we can stop transmission faster than a vaccine can."
Suddenly fully awake, a jolt of panicked electricity races through your body. Has COVID-19 come for you? In the U.S., answering this simple question is incredibly difficult.
Now, you might have to wait for hours in line in your car to get a test for $100, only to find out your result 10-14 days later -- much too late to matter in stopping an outbreak. Due to such obstacles, a recent report in JAMA Internal Medicine estimated that 9 out of 10 infections in the U.S. are being missed.
But what if you could use a paper strip in the privacy of your own home, like a pregnancy test, and find out if you are contagious in real time?
e25 Bio, a small company in Cambridge, Mass., has already created such a test and it has been sitting on a lab bench, inaccessible, since April. It is an antigen test, which looks for proteins on the outside of a virus, and can deliver results in about 15 minutes. Also like an over-the-counter pregnancy test, e25 envisions its paper strips as a public health screening tool, rather than a definitive diagnostic test. People who see a positive result would be encouraged to then seek out a physician-administered, gold-standard diagnostic test: the more sensitive PCR.
Typically, hospitals and other health facilities rely on PCR tests to diagnose viruses. This test can detect small traces of genetic material that a virus leaves behind in the human body, which tells a clinician that the patient is either actively infected with or recently cleared that virus. PCR is quite sensitive, meaning that it is able to detect the presence of a virus' genetic material very accurately.
But although PCR is the gold-standard for diagnostics, it's also the most labor-intensive way to test for a virus and takes a relatively long time to produce results. That's not a good match for stopping super-spreader events during an unchecked pandemic. PCR is also not great at identifying the infected people when they are most at risk of potentially transmitting the virus to others.
That's because the viral threshold at which PCR can detect a positive result is so low, that it's actually too sensitive for the purposes of telling whether someone is contagious.
"The majority of time someone is PCR positive, those [genetic] remnants do not indicate transmissible virus," epidemiologist Michael Mina recently Tweeted. "They indicate remnants of a recently cleared infection."
To stop the chain of transmission for COVID-19, he says, "We need a more accurate test than PCR, that turns positive when someone is able to transmit."
In other words, we need a test that is better at detecting whether a person is contagious, as opposed to whether a small amount of virus can be detected in their nose or saliva. This kind of test is especially critical given the research showing that asymptomatic and pre-symptomatic people have high viral loads and are spreading the virus undetected.
The critical question for contagiousness testing, then, is how big a dose of SARS-CoV-2, the virus that causes COVID, does it take to infect most people? Researchers are still actively trying to answer this. As Angela Rasmussen, a coronavirus expert at Columbia University, told STAT: "We don't know the amount that is required to cause an infection, but it seems that it's probably not a really, really small amount, like measles."
Amesh Adalja, an infectious disease physician and a senior scholar at the Johns Hopkins University Center for Health Security, told LeapsMag: "It's still unclear what viral load is associated with contagiousness but it is biologically plausible that higher viral loads, in general, are associated with more efficient transmission especially in symptomatic individuals. In those without symptoms, however, the same relationship may not hold and this may be one of the reasons young children, despite their high viral loads, are not driving outbreaks."
"Antigen tests work best when there's high viral loads. They're catching people who are super spreaders."
Mina and colleagues estimate that widespread use of weekly cheap, rapid tests that are 100 times less sensitive than PCR tests would prevent outbreaks -- as long as the people who are positive self-isolate.
So why can't we buy e25Bio's test at a drugstore right now? Ironically, it's barred for the very reason that it's useful in the first place: Because it is not sensitive enough to satisfy the U.S. Food and Drug Administration, according to the company.
"We're ready to go," says Carlos-Henri Ferré, senior associate of operations and communications at e25. "We've applied to FDA, and now it's in their hands."
The problem, he said, is that the FDA is evaluating applications for antigen tests based on criteria for assessing diagnostics, like PCR, even when the tests serve a different purpose -- as a screening tool.
"Antigen tests work best when there's high viral loads," Ferré says. "They're catching people who are super spreaders, that are capable of continuing the spread of disease … FDA criteria is for diagnostics and not this."
FDA released guidance on July 29th -- 140 days into the pandemic -- recommending that at-home tests should perform with at least 80 percent sensitivity if ordered by prescription, and at least 90 percent sensitivity if purchased over the counter. "The danger of a false negative result is that it can contribute to the spread of COVID-19," according to an FDA spokesperson. "However, oversight of a health care professional who reviews the results, in combination with the patient's symptoms and uses their clinical judgment to recommend additional testing, if needed, among other things, can help mitigate some risks."
Crucially, the 90 percent sensitivity recommendation is judged upon comparison to PCR tests, meaning that if a PCR test is able to detect virus in 100 samples, the at-home antigen test would need to detect virus in at least 90 of those samples. Since antigen tests only detect high viral loads, frustrated critics like Mina say that such guidance is "unreasonable."
"The FDA at this moment is not understanding the true potential for wide-scale frequent testing. In some ways this is not their fault," Mina told LeapsMag. "The FDA does not have any remit to evaluate tests that fall outside of medical diagnostic testing. The proposal I have put forth is not about diagnostic testing (leave that for symptomatic cases reporting to their physician and getting PCR tests)....Daily rapid tests are not about diagnosing people and they are not about public health surveillance and they are not about passports to go to school, out to dinner or into the office. They are about reducing population-level transmission given a similar approach as vaccines."
A reasonable standard, he added, would be to follow the World Health Organization's Target Product Profiles, which are documents to help developers build desirable and minimally acceptable testing products. "A decent limit," Mina says, "is a 70% or 80% sensitivity (if they truly require sensitivity as a metric) to detect virus at Ct values less than 25. This coincides with detection of the most transmissible people, which is important."
(A Ct value is a type of measurement that corresponds inversely to the amount of viral load in a given sample. Researchers have found that Ct values of 13-17 indicate high viral load, whereas Ct values greater than 34 indicate a lack of infectious virus.)
"We believe this should be an at-home test, but [if FDA approval comes through] the first rollout is to do this in laboratories, hospitals, and clinics."
"We believe that population screening devices have an immediate place and use in helping beat the virus," says Ferré. "You can have a significant impact even with a test at 60% sensitivity if you are testing frequently."
When presented with criticism of its recommendations, the FDA indicated that it will not automatically deny any at-home test that fails to meet the 90 percent sensitivity guidance.
"FDA is always open to alternative proposals from developers, including strategies for serial testing with less sensitive tests," a spokesperson wrote in a statement. "For example, it is possible that overall sensitivity of the strategy could be considered cumulatively rather than based on one-time testing….In the case of a manufacturer with an at-home test that can only detect people with COVID-19 when they have a high viral load, we encourage them to talk with us so we can better understand their test, how they propose to use it, and the validation data they have collected to support that use."
However, the FDA's actions so far conflict with its stated openness. e25 ended up adding a step to the protocol in order to better meet FDA standards for sensitivity, but that extra step—sending samples to a laboratory for results—will undercut the test's ability to work as an at-home screening tool.
"We believe this should be an at-home test, but [if FDA approval comes through] the first rollout is to do this in laboratories, hospitals, and clinics," Ferré says.
According to the FDA, no test developers have approached them with a request for an emergency use authorization that proposes an alternate testing paradigm, such as serial testing, to mitigate test sensitivity below 80 percent.
From a scientific perspective, antigen tests like e25Bio's are not the only horse in the race for a simple rapid test with potential for at-home use. CRISPR technology has long been touted as fertile ground for diagnostics, and in an eerily prescient interview with LeapsMag in November, CRISPR pioneer Feng Zhang spoke of its potential application as an at-home diagnostic for an infectious disease specifically.
"I think in the long run it will be great to see this for, say, at-home disease testing, for influenza and other sorts of important public health [concerns]," he said in the fall. "To be able to get a readout at home, people can potentially quarantine themselves rather than traveling to a hospital and then carrying the risk of spreading that disease to other people as they get to the clinic."
Zhang's company Sherlock Biosciences is now working on scaled-up manufacturing of a test to detect SARS CoV-2. Mammoth Biosciences, which secured funding from the National Institutes of Health's Rapid Acceleration of Diagnostics program, is also working on a CRISPR diagnostic for SARS CoV-2. Both would check the box for rapid testing, but so far not for at-home testing, as they would also require laboratory infrastructure to provide results.
If any at-home tests can clear the regulatory hurdles, they would also need to be manufactured on a large scale and be cheap enough to entice people to actually use them. In the world of at-home diagnostics, pregnancy tests have become the sole mainstream victor because they're simple to use, small to carry, easy to interpret, and costs about seven or eight dollars at any ubiquitous store, like Target or Walmart. By comparison, the at-home COVID collection tests that don't even offer diagnostics—you send away your sample to an external lab—all cost over $100 to take just one time.
For the time being, the only available diagnostics for COVID require a lab or an expensive dedicated machine to process. This disconnect could prolong the world's worst health crisis in a century.
"Daily rapid tests have enormous potential to sever transmission chains and create herd effects similar to herd immunity," Mina says. "We all recognize that vaccines and infections can result in herd immunity when something around half of people are no longer susceptible.
"The same thing exists with these tests. These are the intervention to stop the virus. If half of people choose to use these tests every other day, then we can stop transmission faster than a vaccine can. The technology exists, the theory and mathematics back it up, the epidemiology is sound. There is no reason we are not approaching this as strongly as we would be approaching vaccines."
--Additional reporting by Julia Sklar
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
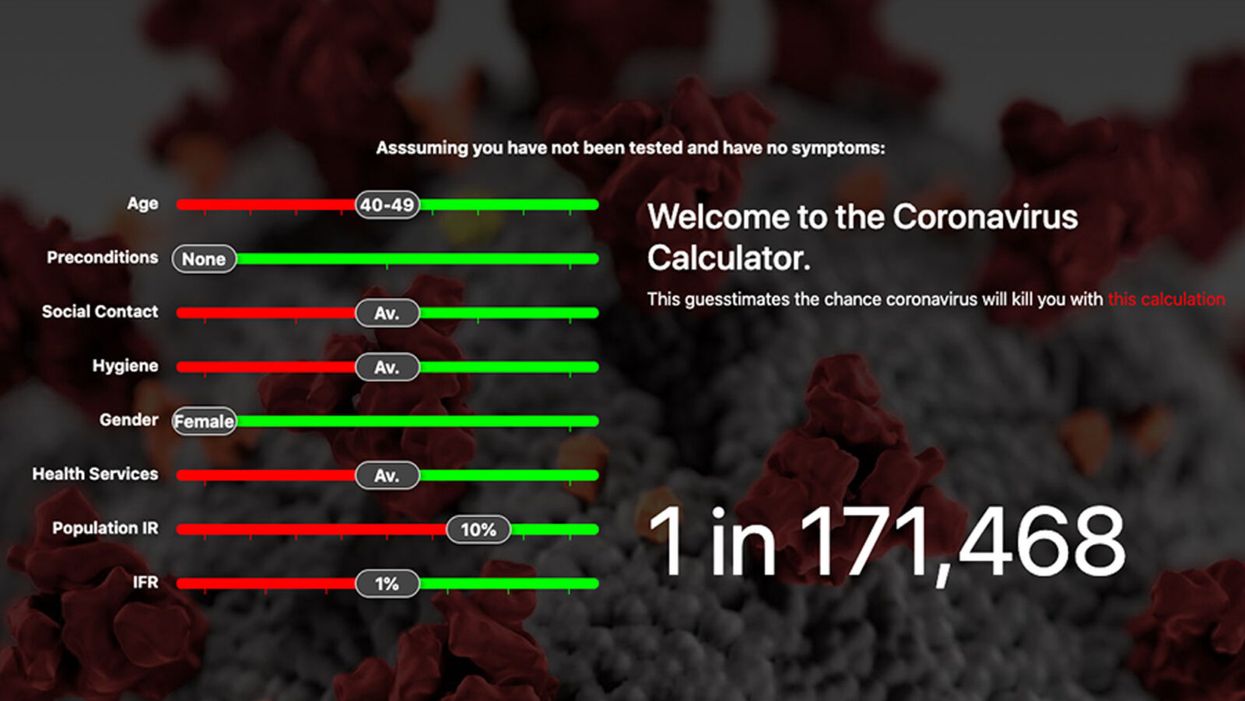
Coronavirus Risk Calculators: What You Need to Know
A screenshot of one coronavirus risk calculator.
People in my family seem to develop every ailment in the world, including feline distemper and Dutch elm disease, so I naturally put fingers to keyboard when I discovered that COVID-19 risk calculators now exist.
"It's best to look at your risk band. This will give you a more useful insight into your personal risk."
But the results – based on my answers to questions -- are bewildering.
A British risk calculator developed by the Nexoid software company declared I have a 5 percent, or 1 in 20, chance of developing COVID-19 and less than 1 percent risk of dying if I get it. Um, great, I think? Meanwhile, 19 and Me, a risk calculator created by data scientists, says my risk of infection is 0.01 percent per week, or 1 in 10,000, and it gave me a risk score of 44 out of 100.
Confused? Join the club. But it's actually possible to interpret numbers like these and put them to use. Here are five tips about using coronavirus risk calculators:
1. Make Sure the Calculator Is Designed For You
Not every COVID-19 risk calculator is designed to be used by the general public. Cleveland Clinic's risk calculator, for example, is only a tool for medical professionals, not sick people or the "worried well," said Dr. Lara Jehi, Cleveland Clinic's chief research information officer.
Unfortunately, the risk calculator's web page fails to explicitly identify its target audience. But there are hints that it's not for lay people such as its references to "platelets" and "chlorides."
The 19 and Me or the Nexoid risk calculators, in contrast, are both designed for use by everyone, as is a risk calculator developed by Emory University.
2. Take a Look at the Calculator's Privacy Policy
COVID-19 risk calculators ask for a lot of personal information. The Nexoid calculator, for example, wanted to know my age, weight, drug and alcohol history, pre-existing conditions, blood type and more. It even asked me about the prescription drugs I take.
It's wise to check the privacy policy and be cautious about providing an email address or other personal information. Nexoid's policy says it provides the information it gathers to researchers but it doesn't release IP addresses, which can reveal your location in certain circumstances.
John-Arne Skolbekken, a professor and risk specialist at Norwegian University of Science and Technology, entered his own data in the Nexoid calculator after being contacted by LeapsMag for comment. He noted that the calculator, among other things, asks for information about use of recreational drugs that could be illegal in some places. "I have given away some of my personal data to a company that I can hope will not misuse them," he said. "Let's hope they are trustworthy."
The 19 and Me calculator, by contrast, doesn't gather any data from users, said Cindy Hu, data scientist at Mathematica, which created it. "As soon as the window is closed, that data is gone and not captured."
The Emory University risk calculator, meanwhile, has a long privacy policy that states "the information we collect during your assessment will not be correlated with contact information if you provide it." However, it says personal information can be shared with third parties.
3. Keep an Eye on Time Horizons
Let's say a risk calculator says you have a 1 percent risk of infection. That's fairly low if we're talking about this year as a whole, but it's quite worrisome if the risk percentage refers to today and jumps by 1 percent each day going forward. That's why it's helpful to know exactly what the numbers mean in terms of time.
Unfortunately, this information isn't always readily available. You may have to dig around for it or contact a risk calculator's developers for more information. The 19 and Me calculator's risk percentages refer to this current week based on your behavior this week, Hu said. The Nexoid calculator, by contrast, has an "infinite timeline" that assumes no vaccine is developed, said Jonathon Grantham, the company's managing director. But your results will vary over time since the calculator's developers adjust it to reflect new data.
When you use a risk calculator, focus on this question: "How does your risk compare to the risk of an 'average' person?"
4. Focus on the Big Picture
The Nexoid calculator gave me numbers of 5 percent (getting COVID-19) and 99.309 percent (surviving it). It even provided betting odds for gambling types: The odds are in favor of me not getting infected (19-to-1) and not dying if I get infected (144-to-1).
However, Grantham told me that these numbers "are not the whole story." Instead, he said, "it's best to look at your risk band. This will give you a more useful insight into your personal risk." Risk bands refer to a segmentation of people into five categories, from lowest to highest risk, according to how a person's result sits relative to the whole dataset.
The Nexoid calculator says I'm in the "lowest risk band" for getting COVID-19, and a "high risk band" for dying of it if I get it. That suggests I'd better stay in the lowest-risk category because my pre-existing risk factors could spell trouble for my survival if I get infected.
Michael J. Pencina, a professor and biostatistician at Duke University School of Medicine, agreed that focusing on your general risk level is better than focusing on numbers. When you use a risk calculator, he said, focus on this question: "How does your risk compare to the risk of an 'average' person?"
The 19 and Me calculator, meanwhile, put my risk at 44 out of 100. Hu said that a score of 50 represents the typical person's risk of developing serious consequences from another disease – the flu.
5. Remember to Take Action
Hu, who helped develop the 19 and Me risk calculator, said it's best to use it to "understand the relative impact of different behaviors." As she noted, the calculator is designed to allow users to plug in different answers about their behavior and immediately see how their risk levels change.
This information can help us figure out if we should change the way we approach the world by, say, washing our hands more or avoiding more personal encounters.
"Estimation of risk is only one part of prevention," Pencina said. "The other is risk factors and our ability to reduce them." In other words, odds, percentages and risk bands can be revealing, but it's what we do to change them that matters.