The World’s First Longevity Charter City: An interview with Niklas Anzinger.

Niklas Anzinger is the founder of Infinita VC based in the charter city of Prospera in Honduras. Infinita focuses on a new trend of charter cities and other forms of alternative jurisdictions. Healso hosts a podcast about how to accelerate the future by unblocking “stranded technologies”.This spring he was a part of the network city experiment Zuzalu spearheaded by Ethereum founder Vitalik Buterin where a few hundred invited guests from the spheres of longevity, biotechnology, crypto, artificial intelligence and investment came together to form a two-monthlong community. It has been described as the world’s first pop-up city. Every morning Vitalians would descend on a long breakfast—the menu had been carefully designed by famed radical longevity self-experimenter Bryan Johnson—and there is where I first met Anzinger who told me about Prospera. Intrigued to say the least, I caught up with him later the same week and the following is a record of our conversation.
Q. We are sitting here in the so-called pop-up network state Zuzalu temporarily realized in the village of Lusticia Bay by the beautiful Mediterranean Sea. To me this is an entirely new concept: What is a network state?
A. A network state is a highly aligned online community that has a level of in-person civility; it crowd-funds territory, and it eventually seeks diplomatic recognition. In a way it's about starting a new country. The term was coined by the crypto influencer and former CTO of Coinbase Balaji Srinivasan in a book by the same title last year [2022]. What many people don't know is that it is a more recent addition or innovation in a space called competitive governance. The idea is that you have multiple jurisdictions competing to provide you services as a customer. When you have competition among governments or government service providers, these entities are forced to provide you with a better service instead of the often worse service at higher prices or higher taxes that we're currently getting. The idea went from seasteading, which was hardly feasible because of costs, to charter cities getting public/private partnerships with existing governments and a level of legal autonomy, to special economic zones, to now network states.
Q. How do network states compare to charter cities and similar jurisdictions?
A. Charter cities and special economic zones were legal forks from other existing states. Dubai, Shenzhen in China, to some degree Hong Kong, to some degree Singapore are some examples. There's a host of other charter cities, one of which I'm based in myself, which is Prospera located in Honduras on the island Roatán. Charter cities provide the full stack of governance; they provide new laws and regulations, business registration, tax codes and governance services, Estonia style: you log on to the government platform and you get services as a citizen.
When conceptualizing network states, Balagi Srinivasan turns the idea of a charter city a bit on its head: he doesn't want to start with this full stack because it's still very hard to get these kinds of partnerships with government. It's very expensive and requires lots of experience and lots of social capital. He is saying that network states could instead start as an online community. They could have a level of alignment where they trade with each other; they have their own economy; they meet in person in regular gatherings like we're doing here in Zuzulu for two months, and then they negotiate with existing governments or host cities to get a certain degree of legal autonomy that is centered around a moral innovation. So, his idea is: don't focus on building a completely new country or city; focus on a moral innovation.
Q. What would be an example of such a moral innovation?
A. An example would be longevity—life is good; death is bad—let's see what we can do to foster progress around that moral innovation and see how we can get legal forks from the existing system that allow us to accelerate progress in that area. There is an increasing realization in the science that there are hallmarks of aging and that aging is a cause of other diseases like cancer, ALS or Alzheimer's. But aging is not recognized as a disease by the FDA in the United States and in most countries around the world, so it's very hard to get scientific funding for biotechnology that would attack the hallmarks of aging and allow us potentially to reverse aging and extend life. This is a significant shortcoming of existing government systems that groups such as the ones that have come together here in Montenegro are now seeking alternatives too. Charter cities and now network states are such alternatives.
Q. Would it not be better to work within the current systems, and try to improve them, rather than abandon them for new experimental jurisdictions?
A. There are numerous failures of public policies. These failures are hard, if not impossible, to reverse, because as soon as you have these policies, you have entrenched interests who benefit from the regulations. The only way to disrupt incumbent industries is with start-ups, but the way the system is set up makes it excessively hard for such start-ups to become big companies. In fact, larger companies are weaponizing the legal system against small companies, because they can afford the lawyers and the fixed cost of compliance.
I don't believe that our institutions in many developed countries are beyond hope. I just think it's easier to change them if you could point at successful examples. ‘Hey, this country or this zone is already doing it very successfully’; if they can extend people’s lifespan by 10 years, if they can reduce maternal mortality, and if they have a massive medical tourism where people come back healthier, then that is just very embarrassing for the FDA.
Q. Perhaps a comparison here would be the relationship between Hong Kong and China?
A. Correct, so having Hong Kong right in front of your door … ‘Hey, this capitalism thing seems to work, why don't we try it here?’ It was due to the very bold leadership by Deng Xiaoping that they experimented with it in the development zone of Shenzhen. It worked really well and then they expanded with more special economic zones that also worked.

Próspera is a private city and special economic zone on the island of Roatán in the Central American state of Honduras.
Q. Tell us about Prospera, the charter city in Honduras, that you are intimately connected with.
A. Honduras is a very poor country. It has a lot of crime, never had a single VC investment, and has a GDP per capita of 2,000 per year. Honduras has suffered tremendously. The goal of these special economic zones is to bring in economic development. That's their sole purpose. It's a homegrown innovation from Honduras that started in 2009 with a very forward-thinking statesman, Octavio Sanchez, who was the chief of staff to the president of Honduras, and then president. He had his own ideas about making Honduras a more decentralized system, where more of the power lies in the municipalities.
Inspired by the ideas of Nobel laureate economist Paul Romer, who gave a famous Ted Talk in 2009 about charter cities, Sanchez initiated a process that lasted for years and eventually led to the creation of a special economic zone legal regime that’s anchored in the Hunduran constitution that provides the highest legal autonomy in the world to these zones. There are today three special economic zones approved by the Honduran government: Prospera, Ciudad Morazan and Orchidea.
Q. How did you become interested and then involved in Prospera?
A. I read about it first in an article by Scott Alexander, a famous rationalist blogger, who wrote a very long article about Prospera, and I thought, this is amazing! Then I came to Prospera and I found it to be one of the most if not the most exciting project in the world going on right now and that it also opened my heart to the country and its people. Most of my friends there are Honduran, they have been working on this for 10 or more years. They want to remake Honduras and put it on the map as the place in the world where this legal and governance innovation started.
Q. To what extent is Prospera autonomous relative to the Honduran government?
A. What's interesting about the Honduran model is that it's anchored within the Honduran constitution, and it has a very clear framework for what's possible and what's not possible, and what's possible ensures the highest degree of legal autonomy anywhere seen in the world. Prospera has really pushed the model furthest in creating a common law-based polycentric legal system. The idea is that you don't have a legislature, instead you have common law and it's based on the best practice common law principles that a legal scholar named Tom W. Bell created.
One of the core ideas is that as a business you're not obligated to follow one regulatory monopoly like the FDA. You have regulatory flexibility so you can choose what you're regulated under. So, you can say: ‘if I do a medical clinic, I do it under Norwegian law here’. And you even have the possibility to amend it a bit. You're still required to have liability insurance, and have to agree to binding arbitration in case there's a legal dispute. And your insurance has to approve you. So, under that model the insurance becomes the regulator and they regulate through prices. The limiting factor is criminal law; Honduran criminal law fully applies. So does immigration law. And we pay taxes.
Q. Is there also an idea of creating a kind of healthy living there, and encourage medical tourism?
A. Yes, we specifically look for legal advantages in autonomy around creating new drugs, doing clinical trials, doing self-medication and experimentation. There is a stem cell clinic here and they're doing clinical trials. The island of Roatán is very easily accessible for American tourists. It's a beautiful island, and it's for regulatory reasons hard to do stem cell therapies in the United States, so they're flying in patients from the United States. Most of them are very savvy and often have PhDs in biotech and are able to assess the risk for themselves of taking drugs and doing clinical trials. We're also going to get a wellness center, and there have been ideas around establishing a peptide clinic and a compound pharmacy and things like that. We are developing a healthcare ecosystem.
Q. This kind of experimental tourism raises some ethical issues. What happens if patients are harmed? And what are the moral implications for society of these new treatments?
A. As a moral principle we believe in medical freedom: people have rights over their bodies, even at the (informed) risk of harm to themselves if no unconsenting third-parties are harmed; this is a fundamental right currently not protected effectively.
What we do differently is not changing ethical norms around safety and efficacy, we’re just changing the institutional setup. Instead of one centralized bureaucracy, like the FDA, we have regulatory pluralism that allows different providers of safety and efficacy to compete under market rules. Like under any legal system, common law in Prospera punishes malpractice, fraud, murder etc. This system will still produce safe and effective drugs, and it will still work with common sense legal notions like informed consent and liability for harm. There are regulations for medical practice, there is liability insurance and things like that. It will just do so more efficiently than the current way of doing things (unless it won’t, in which case it will change and evolve – or fail).
A direct moral benefit ´to what we do is that we increase accessibility. Typical gene therapies on the market cost $1 million dollars in the US. The gene therapy developed in Prospera costs $25,000. As to concern about whether such treatments are problematic, we do not share this perspective. We are for advancing science responsibly and we believe that both individuals and society stand to gain from improving the resiliency of the human body through advanced biotechnology.
Q. How does Prospera relate to the local Honduran population?
A. I think it's very important that our projects deliver local benefits and that they're well anchored in local communities. Because when you go to a new place, you're seen as a foreigner, and you're seen as potentially a danger or a threat. The most important thing for Prospera and Ciudad Morazan is to show we're creating jobs; we're creating employment; we're improving people's lives on the ground. Prospera is directly and indirectly employing 1,100 people. More than 2/3 of the people who are working for Prospera are Honduran. It has a lot of local service workers from the island, and it has educated Hondurans from the mainland for whom it's an alternative to going to the United States.
Q. What makes a good Prosperian citizen?
A. People in Prospera are very entrepreneurial. They're opening companies on a small scale. For example, Vehinia, who is the cook in the kitchen at Prospera, she's from the neighboring village and she started an NGO that is now funding a school where children from the local village can go to instead of a school that's 45 minutes away. There's very much a spirit of ‘let's exchange and trade with each other’. Some people might see that as a bit too commercial, but that's something about the culture that people accept and that people see as a good thing.
Q. Five years from now, if everything goes well, what do we see in Prospera?
A. I think Prospera will have at least 10,000 residents and I think Honduras hopefully will have more zones. There could be zones with a thriving industrial sector and sort of a labor-intensive economy and some that are very strong in pharmaceuticals, there could also be other zones for synthetic biology, and other zones focused on agriculture. The zones of Prospera, Ciudad Morazan and Orchidea are already showing the results we want to see, the results that we will eventually be measured by, and I'm tremendously excited about Honduras.
A company in England has made a test that picks out the compounds from breath that reveal if people have liver disease.
Every year, around two million people worldwide die of liver disease. While some people inherit the disease, it’s most commonly caused by hepatitis, obesity and alcoholism. These underlying conditions kill liver cells, causing scar tissue to form until eventually the liver cannot function properly. Since 1979, deaths due to liver disease have increased by 400 percent.
The sooner the disease is detected, the more effective treatment can be. But once symptoms appear, the liver is already damaged. Around 50 percent of cases are diagnosed only after the disease has reached the final stages, when treatment is largely ineffective.
To address this problem, Owlstone Medical, a biotech company in England, has developed a breath test that can detect liver disease earlier than conventional approaches. Human breath contains volatile organic compounds (VOCs) that change in the first stages of liver disease. Owlstone’s breath test can reliably collect, store and detect VOCs, while picking out the specific compounds that reveal liver disease.
“There’s a need to screen more broadly for people with early-stage liver disease,” says Owlstone’s CEO Billy Boyle. “Equally important is having a test that's non-invasive, cost effective and can be deployed in a primary care setting.”
The standard tool for detection is a biopsy. It is invasive and expensive, making it impractical to use for people who aren't yet symptomatic. Meanwhile, blood tests are less invasive, but they can be inaccurate and can’t discriminate between different stages of the disease.
In the past, breath tests have not been widely used because of the difficulties of reliably collecting and storing breath. But Owlstone’s technology could help change that.
The team is testing patients in the early stages of advanced liver disease, or cirrhosis, to identify and detect these biomarkers. In an initial study, Owlstone’s breathalyzer was able to pick out patients who had early cirrhosis with 83 percent sensitivity.
Boyle’s work is personally motivated. His wife died of colorectal cancer after she was diagnosed with a progressed form of the disease. “That was a big impetus for me to see if this technology could work in early detection,” he says. “As a company, Owlstone is interested in early detection across a range of diseases because we think that's a way to save lives and a way to save costs.”
How it works
In the past, breath tests have not been widely used because of the difficulties of reliably collecting and storing breath. But Owlstone’s technology could help change that.
Study participants breathe into a mouthpiece attached to a breath sampler developed by Owlstone. It has cartridges are designed and optimized to collect gases. The sampler specifically targets VOCs, extracting them from atmospheric gases in breath, to ensure that even low levels of these compounds are captured.
The sampler can store compounds stably before they are assessed through a method called mass spectrometry, in which compounds are converted into charged atoms, before electromagnetic fields filter and identify even the tiniest amounts of charged atoms according to their weight and charge.
The top four compounds in our breath
In an initial study, Owlstone captured VOCs in breath to see which ones could help them tell the difference between people with and without liver disease. They tested the breath of 46 patients with liver disease - most of them in the earlier stages of cirrhosis - and 42 healthy people. Using this data, they were able to create a diagnostic model. Individually, compounds like 2-Pentanone and limonene performed well as markers for liver disease. Owlstone achieved even better performance by examining the levels of the top four compounds together, distinguishing between liver disease cases and controls with 95 percent accuracy.
“It was a good proof of principle since it looks like there are breath biomarkers that can discriminate between diseases,” Boyle says. “That was a bit of a stepping stone for us to say, taking those identified, let’s try and dose with specific concentrations of probes. It's part of building the evidence and steering the clinical trials to get to liver disease sensitivity.”
Sabine Szunerits, a professor of chemistry in Institute of Electronics at the University of Lille, sees the potential of Owlstone’s technology.
“Breath analysis is showing real promise as a clinical diagnostic tool,” says Szunerits, who has no ties with the company. “Owlstone Medical’s technology is extremely effective in collecting small volatile organic biomarkers in the breath. In combination with pattern recognition it can give an answer on liver disease severity. I see it as a very promising way to give patients novel chances to be cured.”
Improving the breath sampling process
Challenges remain. With more than one thousand VOCs found in the breath, it can be difficult to identify markers for liver disease that are consistent across many patients.
Julian Gardner is a professor of electrical engineering at Warwick University who researches electronic sensing devices. “Everyone’s breath has different levels of VOCs and different ones according to gender, diet, age etc,” Gardner says. “It is indeed very challenging to selectively detect the biomarkers in the breath for liver disease.”
So Owlstone is putting chemicals in the body that they know interact differently with patients with liver disease, and then using the breath sampler to measure these specific VOCs. The chemicals they administer are called Exogenous Volatile Organic Compound) probes, or EVOCs.
Most recently, they used limonene as an EVOC probe, testing 29 patients with early cirrhosis and 29 controls. They gave the limonene to subjects at specific doses to measure how its concentrations change in breath. The aim was to try and see what was happening in their livers.
“They are proposing to use drugs to enhance the signal as they are concerned about the sensitivity and selectivity of their method,” Gardner says. “The approach of EVOC probes is probably necessary as you can then eliminate the person-to-person variation that will be considerable in the soup of VOCs in our breath.”
Through these probes, Owlstone could identify patients with liver disease with 83 percent sensitivity. By targeting what they knew was a disease mechanism, they were able to amplify the signal. The company is starting a larger clinical trial, and the plan is to eventually use a panel of EVOC probes to make sure they can see diverging VOCs more clearly.
“I think the approach of using probes to amplify the VOC signal will ultimately increase the specificity of any VOC breath tests, and improve their practical usability,” says Roger Yazbek, who leads the South Australian Breath Analysis Research (SABAR) laboratory in Flinders University. “Whilst the findings are interesting, it still is only a small cohort of patients in one location.”
The future of breath diagnosis
Owlstone wants to partner with pharmaceutical companies looking to learn if their drugs have an effect on liver disease. They’ve also developed a microchip, a miniaturized version of mass spectrometry instruments, that can be used with the breathalyzer. It is less sensitive but will enable faster detection.
Boyle says the company's mission is for their tests to save 100,000 lives. "There are lots of risks and lots of challenges. I think there's an opportunity to really establish breath as a new diagnostic class.”
Doctors worry that fungal pathogens may cause the next pandemic.
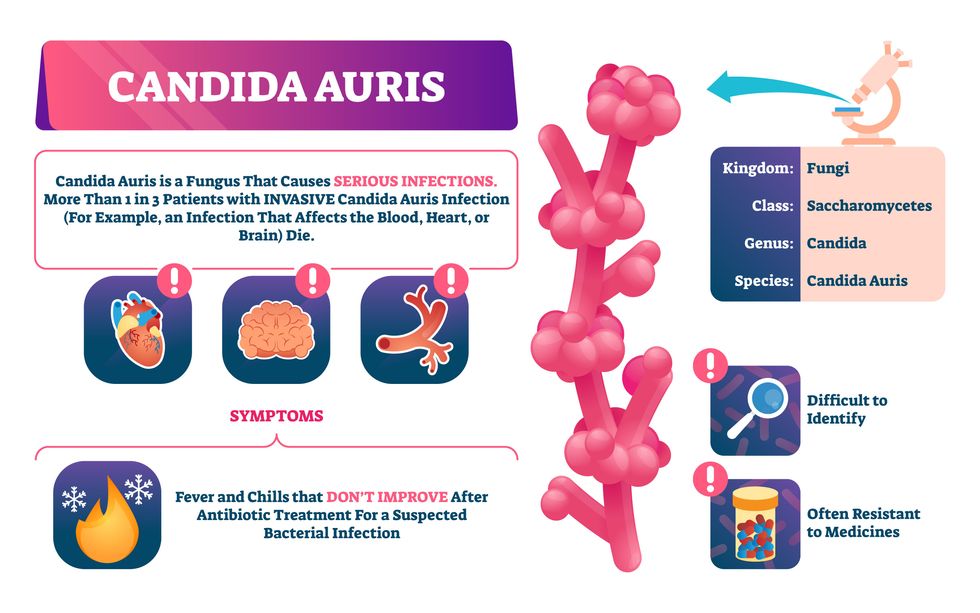
Bacterial antibiotic resistance has been a concern in the medical field for several years. Now a new, similar threat is arising: drug-resistant fungal infections. The Centers for Disease Control and Prevention considers antifungal and antimicrobial resistance to be among the world’s greatest public health challenges.
One particular type of fungal infection caused by Candida auris is escalating rapidly throughout the world. And to make matters worse, C. auris is becoming increasingly resistant to current antifungal medications, which means that if you develop a C. auris infection, the drugs your doctor prescribes may not work. “We’re effectively out of medicines,” says Thomas Walsh, founding director of the Center for Innovative Therapeutics and Diagnostics, a translational research center dedicated to solving the antimicrobial resistance problem. Walsh spoke about the challenges at a Demy-Colton Virtual Salon, one in a series of interactive discussions among life science thought leaders.
Although C. auris typically doesn’t sicken healthy people, it afflicts immunocompromised hospital patients and may cause severe infections that can lead to sepsis, a life-threatening condition in which the overwhelmed immune system begins to attack the body’s own organs. Between 30 and 60 percent of patients who contract a C. auris infection die from it, according to the CDC. People who are undergoing stem cell transplants, have catheters or have taken antifungal or antibiotic medicines are at highest risk. “We’re coming to a perfect storm of increasing resistance rates, increasing numbers of immunosuppressed patients worldwide and a bug that is adapting to higher temperatures as the climate changes,” says Prabhavathi Fernandes, chair of the National BioDefense Science Board.
Most Candida species aren’t well-adapted to our body temperatures so they aren’t a threat. C. auris, however, thrives at human body temperatures.
Although medical professionals aren’t concerned at this point about C. auris evolving to affect healthy people, they worry that its presence in hospitals can turn routine surgeries into life-threatening calamities. “It’s coming,” says Fernandes. “It’s just a matter of time.”
An emerging global threat
“Fungi are found in the environment,” explains Fernandes, so Candida spores can easily wind up on people’s skin. In hospitals, they can be transferred from contact with healthcare workers or contaminated surfaces. Most Candida species aren’t well-adapted to our body temperatures so they aren’t a threat. C. auris, however, thrives at human body temperatures. It can enter the body during medical treatments that break the skin—and cause an infection. Overall, fungal infections cost some $48 billion in the U.S. each year. And infection rates are increasing because, in an ironic twist, advanced medical therapies are enabling severely ill patients to live longer and, therefore, be exposed to this pathogen.
The first-ever case of a C. auris infection was reported in Japan in 2009, although an analysis of Candida samples dated the earliest strain to a 1996 sample from South Korea. Since then, five separate varieties – called clades, which are similar to strains among bacteria – developed independently in different geographies: South Asia, East Asia, South Africa, South America and, recently, Iran. So far, C. auris infections have been reported in 35 countries.
In the U.S., the first infection was reported in 2016, and the CDC started tracking it nationally two years later. During that time, 5,654 cases have been reported to the CDC, which only tracks U.S. data.
What’s more notable than the number of cases is their rate of increase. In 2016, new cases increased by 175 percent and, on average, they have approximately doubled every year. From 2016 through 2022, the number of infections jumped from 63 to 2,377, a roughly 37-fold increase.
“This reminds me of what we saw with epidemics from 2013 through 2020… with Ebola, Zika and the COVID-19 pandemic,” says Robin Robinson, CEO of Spriovas and founding director of the Biomedical Advanced Research and Development Authority (BARDA), which is part of the U.S. Department of Health and Human Services. These epidemics started with a hockey stick trajectory, Robinson says—a gradual growth leading to a sharp spike, just like the shape of a hockey stick.
Another challenge is that right now medics don’t have rapid diagnostic tests for fungal infections. Currently, patients are often misdiagnosed because C. auris resembles several other easily treated fungi. Or they are diagnosed long after the infection begins and is harder to treat.
The problem is that existing diagnostics tests can only identify C. auris once it reaches the bloodstream. Yet, because this pathogen infects bodily tissues first, it should be possible to catch it much earlier before it becomes life-threatening. “We have to diagnose it before it reaches the bloodstream,” Walsh says.
The most alarming fact is that some Candida infections no longer respond to standard therapeutics.
“We need to focus on rapid diagnostic tests that do not rely on a positive blood culture,” says John Sperzel, president and CEO of T2 Biosystems, a company specializing in diagnostics solutions. Blood cultures typically take two to three days for the concentration of Candida to become large enough to detect. The company’s novel test detects about 90 percent of Candida species within three to five hours—thanks to its ability to spot minute quantities of the pathogen in blood samples instead of waiting for them to incubate and proliferate.
Unlike other Candida species C. auris thrives at human body temperatures
Adobe Stock
Tackling the resistance challenge
The most alarming fact is that some Candida infections no longer respond to standard therapeutics. The number of cases that stopped responding to echinocandin, the first-line therapy for most Candida infections, tripled in 2020, according to a study by the CDC.
Now, each of the first four clades shows varying levels of resistance to all three commonly prescribed classes of antifungal medications, such as azoles, echinocandins, and polyenes. For example, 97 percent of infections from C. auris Clade I are resistant to fluconazole, 54 percent to voriconazole and 30 percent of amphotericin. Nearly half are resistant to multiple antifungal drugs. Even with Clade II fungi, which has the least resistance of all the clades, 11 to 14 percent have become resistant to fluconazole.
Anti-fungal therapies typically target specific chemical compounds present on fungi’s cell membranes, but not on human cells—otherwise the medicine would cause damage to our own tissues. Fluconazole and other azole antifungals target a compound called ergosterol, preventing the fungal cells from replicating. Over the years, however, C. auris evolved to resist it, so existing fungal medications don’t work as well anymore.
A newer class of drugs called echinocandins targets a different part of the fungal cell. “The echinocandins – like caspofungin – inhibit (a part of the fungi) involved in making glucan, which is an essential component of the fungal cell wall and is not found in human cells,” Fernandes says. New antifungal treatments are needed, she adds, but there are only a few magic bullets that will hit just the fungus and not the human cells.
Research to fight infections also has been challenged by a lack of government support. That is changing now that BARDA is requesting proposals to develop novel antifungals. “The scope includes C. auris, as well as antifungals following a radiological/nuclear emergency, says BARDA spokesperson Elleen Kane.
The remaining challenge is the number of patients available to participate in clinical trials. Large numbers are needed, but the available patients are quite sick and often die before trials can be completed. Consequently, few biopharmaceutical companies are developing new treatments for C. auris.
ClinicalTrials.gov reports only two drugs in development for invasive C. auris infections—those than can spread throughout the body rather than localize in one particular area, like throat or vaginal infections: ibrexafungerp by Scynexis, Inc., fosmanogepix, by Pfizer.
Scynexis’ ibrexafungerp appears active against C. auris and other emerging, drug-resistant pathogens. The FDA recently approved it as a therapy for vaginal yeast infections and it is undergoing Phase III clinical trials against invasive candidiasis in an attempt to keep the infection from spreading.
“Ibreafungerp is structurally different from other echinocandins,” Fernandes says, because it targets a different part of the fungus. “We’re lucky it has activity against C. auris.”
Pfizer’s fosmanogepix is in Phase II clinical trials for patients with invasive fungal infections caused by multiple Candida species. Results are showing significantly better survival rates for people taking fosmanogepix.
Although C. auris does pose a serious threat to healthcare worldwide, scientists try to stay optimistic—because they recognized the problem early enough, they might have solutions in place before the perfect storm hits. “There is a bit of hope,” says Robinson. “BARDA has finally been able to fund the development of new antifungal agents and, hopefully, this year we can get several new classes of antifungals into development.”

