These Abortion Drugs Are Proven Safe and Effective. Why Can't Patients Use Them?

Due to federal regulations, access to abortion medications is restricted, despite their record of safety and efficacy.
A few days before Christmas 2015, Paige Alexandria, a 28-year-old counselor at the Austin Women's Health Center in Texas, found out she was pregnant.
Alexandria had missed the cutoff for a medication abortion by three days.
"It was an unplanned pregnancy, and instantaneously I knew I needed an abortion," Alexandria recalls. Already a mother of two children, one with special needs, a third child was not something Alexandria and her husband felt prepared to take on. "Mentally, I knew my limit. I wasn't prepared for a third and I didn't want one," she says.
At an ultrasound appointment one week later, scans showed she was a little over eight weeks pregnant. Alexandria opted to have an abortion as soon as possible, and preferably with medication. "I really wanted to avoid a surgical abortion," she says. "It sounded a lot more invasive, and I'm already uncomfortable with pap smears and pelvic exams, so I initially went in wanting to do the pill."
But at the time, medication guidelines stipulated that one of the pills, called Mifepristone, could only be prescribed to end a pregnancy at eight weeks gestation or earlier – Alexandria had missed the cutoff by three days. If she wanted to end the pregnancy, she would need to undergo a surgical abortion, otherwise known as a vacuum aspiration abortion.
With a vacuum aspiration abortion, doctors dilate the cervix and manually aspirate out the contents of the uterus. Medication abortion, on the other hand, consists of the patient taking two pills – Mifepristone, which blocks the hormones that help the pregnancy develop, and Misoprostol, which empties the uterus over a period of days, identical to a miscarriage.
Alexandria was upset about the change of plans but resolute in her decision to end the pregnancy. "The fact that I didn't really have a choice in how my procedure was performed has made the experience just a little more sensitive for me," she says. She scheduled the earliest available appointment for a surgical abortion.

Paige Alexandria would have chosen to terminate her pregnancy with medication if the regulations were less stringent.
(Photo courtesy of Alexandria)
Like Alexandria, many people looking to terminate a pregnancy opt to do so with medication. According to research from the Guttmacher Institute, medication abortions accounted for nearly 40 percent of all abortions in the year 2017 – a marked increase from 2001, when medication abortions only accounted for roughly five percent of terminations. Taken 24-48 hours apart, Mifepristone and Misoprostol have a 95-99 percent success rate in terminating pregnancies up to 63 days – or nine weeks – of gestation, according to the American College of Obstetrics and Gynecology (ACOG).
But even though the World Health Organization (WHO) considers medical abortion to be highly safe and effective, the medication is still carefully guarded in the United States: Mifepristone is only available for terminating pregnancies up to 10 weeks gestation, per the FDA, even though limited research suggests that both are safe and effective at terminating pregnancies between 12 and 20 weeks.
Additionally, a separate set of regulations known as a Risk Evaluation and Mitigation Strategy (REMS) means that patients can only take Mifepristone under specific circumstances. Mifepristone must be distributed in person by a healthcare provider – usually interpreted in most states as a doctor or nurse practitioner – who has registered with the drug's manufacturer. The medication cannot be distributed through a pharmacy, so doctors who wish to provide the drug must stock the medication in-office, and both the provider and the patient must sign a form that warns them of the "risk of serious complications associated with Mifepristone," according to the FDA.
"REMS is a set of restrictions that the FDA puts on the distribution of drugs it considers dangerous or risky in some way," says Dr. Elizabeth Raymond, an OB-GYN and senior medical associate at Gynuity Health Projects. Although not always called REMS, these restrictions have been imposed on Mifepristone since the medication was approved by the FDA in 2000, Raymond says.
Raymond is part of a growing number of physicians and researchers who want to eliminate the REMS requirements for Mifepristone, also known by its brand name Mifeprex. In 2017, Raymond and several other physicians authored a paper in the New England Journal of Medicine (NEJM) arguing that Mifepristone is extremely safe and needlessly over-regulated.
"When the FDA first approved [Mifepristone] and imposed these requirements, they might have made sense 19 years ago when there was limited information about the use of this treatment in the United States," says Dr. Daniel Grossman, director at Advancing New Standards in Reproductive Health at UCSF and co-author of the 2017 report in the NEJM. "Now, after 19 years, it's clear that this medication is very safe, and safer than a lot of others available in a pharmacy."
Since 2000, Mifepristone has been implicated in 19 deaths, making its mortality rate 0.00063 percent.
According to their research, over three million people have taken Mifepristone since it was approved in 2000. Since then, Mifepristone has been implicated in 19 deaths, making its mortality rate 0.00063 percent. Even then, the risk is inflated, Grossman says.
"The requirement is that practitioners need to report any deaths that occur after taking these medications, and so you'll see deaths included in that figure which are homicides or suicides or something unrelated to taking Mifepristone," says Grossman. In contrast, Acetaminophen – better known as Tylenol – was associated with 458 overdose deaths between 1990 and 1998, as well as 56,000 emergency room visits and 26,000 hospitalizations. Sildenafil, better known as Viagra, was linked to 762 deaths in the first twenty months after it was approved by the FDA. Yet neither Tylenol nor Viagra have been burdened with the same REMS restrictions as Mifepristone.
"It's clearly about more than just the safety of the medication at this point," says Grossman. "It's more about stigma related to abortion and politics."
For people who want a medication abortion, the REMS requirements mean they often need to take off work to schedule a doctor's appointment, arrange for transportation and childcare, and then arrange an additional doctor's appointment days afterward to take the second dose of medication. While surgical abortion procedures are quicker (usually a one-day outpatient procedure, depending on gestation), many people prefer having the abortion in the comfort of their home or surrounded by family instead.
Paige Alexandria, who counsels people seeking abortions at her job, says that survivors of sexual violence often prefer medical abortions to surgical ones. "A lot of time survivors have a trauma associated with medical instruments or having pelvic exams, and so they're more comfortable taking a pill," she says.
But REMS also creates a barrier for healthcare providers, Grossman says. Stocking the medication in-office is "a hassle" and "expensive," while others are reluctant to register their name with the drug manufacturer, fearing harassment or violence from anti-choice protestors. As a result, the number of practitioners willing to provide medical abortions nationwide is severely limited. According to Grossman's own research published in the journal Obstetrics and Gynecology, 28 percent of OBGYNs admitted they would administer medication abortions if it were possible to write a prescription for Mifepristone rather than stock it in-office.
Amazingly, the restrictions on Mifepristone have loosened since it first came on the market. In 2016, the FDA updated the guidelines on Mifepristone to allow its use until 10 weeks gestation, up from eight weeks. But doctors say the REMS restrictions should be eliminated completely so that people can obtain abortions as early as possible.
"REMS restrictions inhibit people from being able to get a timely abortion," says Raymond, who stresses that abortion is generally more comfortable, more affordable, and safer for women the earlier it's done. "Abortion is very safe no matter when you get it, but it's also easier because there's less risk for bleeding, infections, or other complications," Raymond says. Abortions that occur earlier than eight weeks of gestation have a complication rate of less than one percent, while an abortion done at 12 or 13 weeks has a three to six percent chance of complications.
And even for people who want a medication abortion early on in their pregnancy, REMS restrictions make it so that they may not have time to obtain it before the 10-week period lapses, Raymond says.
"If you're seven weeks pregnant but it takes you three weeks to figure out travel and childcare arrangements to go into the doctor and take this medication, now you're at the cutoff date," she says. "Even if you manage to get an abortion at nine weeks, that's still a later gestational age, and so the risks are increased."
In 2016, at a little over nine weeks gestation, Alexandria completed her abortion by having a D&E. But because she didn't have anyone to drive her home after the procedure, she wasn't able to have sedation throughout, something she describes as "traumatic."
"I had the abortion completely aware and coherent, and paired with the fact that I hadn't even wanted a surgical abortion in the first place made it harder to deal with," Alexandria says.
"When you're just a day or two past eight weeks and you want an abortion – why is medication not immediately available?"
Today, Alexandria shares her story publicly to advocate for abortion care. Although she doesn't regret her surgical abortion and acknowledges that not everyone experiences surgical abortion the same way she did, she does wish that she could have gone a different route.
"If I had to do it over, I would still try to do the pill, because [the surgical abortion] was such a terrifying experience," she says. "When you're just a day or two past eight weeks and you want an abortion – why is medication not immediately available? It just doesn't make sense."
A robot server, controlled remotely by a disabled worker, delivers drinks to patrons at the DAWN cafe in Tokyo.
A sleek, four-foot tall white robot glides across a cafe storefront in Tokyo’s Nihonbashi district, holding a two-tiered serving tray full of tea sandwiches and pastries. The cafe’s patrons smile and say thanks as they take the tray—but it’s not the robot they’re thanking. Instead, the patrons are talking to the person controlling the robot—a restaurant employee who operates the avatar from the comfort of their home.
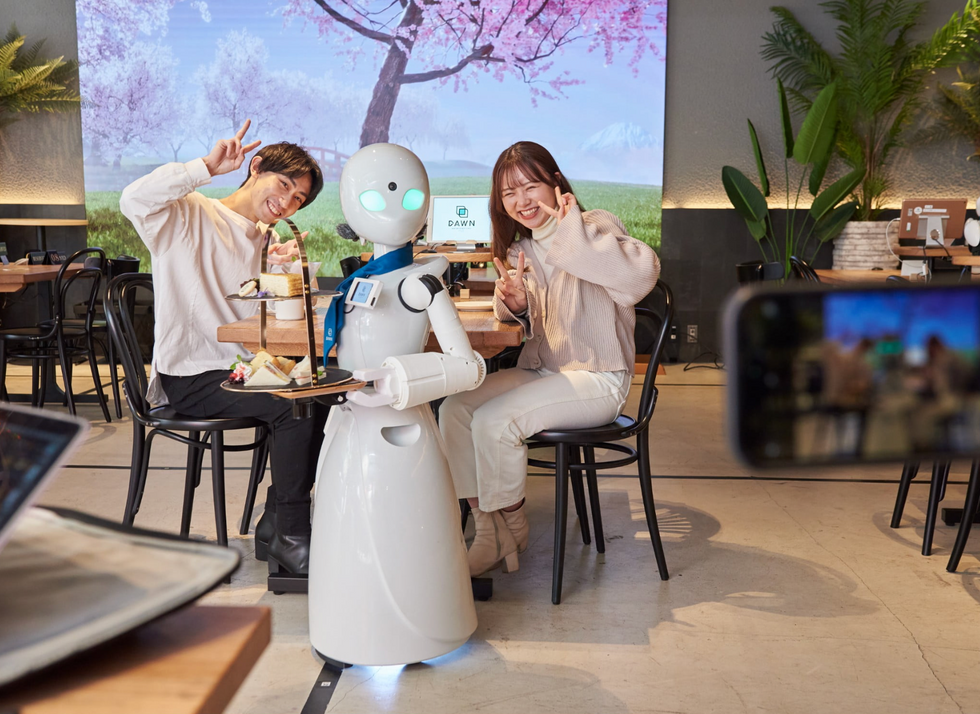
It’s a typical scene at DAWN, short for Diverse Avatar Working Network—a cafe that launched in Tokyo six years ago as an experimental pop-up and quickly became an overnight success. Today, the cafe is a permanent fixture in Nihonbashi, staffing roughly 60 remote workers who control the robots remotely and communicate to customers via a built-in microphone.
More than just a creative idea, however, DAWN is being hailed as a life-changing opportunity. The workers who control the robots remotely (known as “pilots”) all have disabilities that limit their ability to move around freely and travel outside their homes. Worldwide, an estimated 16 percent of the global population lives with a significant disability—and according to the World Health Organization, these disabilities give rise to other problems, such as exclusion from education, unemployment, and poverty.
These are all problems that Kentaro Yoshifuji, founder and CEO of Ory Laboratory, which supplies the robot servers at DAWN, is looking to correct. Yoshifuji, who was bedridden for several years in high school due to an undisclosed health problem, launched the company to help enable people who are house-bound or bedridden to more fully participate in society, as well as end the loneliness, isolation, and feelings of worthlessness that can sometimes go hand-in-hand with being disabled.
“It’s heartbreaking to think that [people with disabilities] feel they are a burden to society, or that they fear their families suffer by caring for them,” said Yoshifuji in an interview in 2020. “We are dedicating ourselves to providing workable, technology-based solutions. That is our purpose.”

Shota, Kuwahara, a DAWN employee with muscular dystrophy, agrees. "There are many difficulties in my daily life, but I believe my life has a purpose and is not being wasted," he says. "Being useful, able to help other people, even feeling needed by others, is so motivational."
A woman receives a mammogram, which can detect the presence of tumors in a patient's breast.
When a patient is diagnosed with early-stage breast cancer, having surgery to remove the tumor is considered the standard of care. But what happens when a patient can’t have surgery?
Whether it’s due to high blood pressure, advanced age, heart issues, or other reasons, some breast cancer patients don’t qualify for a lumpectomy—one of the most common treatment options for early-stage breast cancer. A lumpectomy surgically removes the tumor while keeping the patient’s breast intact, while a mastectomy removes the entire breast and nearby lymph nodes.
Fortunately, a new technique called cryoablation is now available for breast cancer patients who either aren’t candidates for surgery or don’t feel comfortable undergoing a surgical procedure. With cryoablation, doctors use an ultrasound or CT scan to locate any tumors inside the patient’s breast. They then insert small, needle-like probes into the patient's breast which create an “ice ball” that surrounds the tumor and kills the cancer cells.
Cryoablation has been used for decades to treat cancers of the kidneys and liver—but only in the past few years have doctors been able to use the procedure to treat breast cancer patients. And while clinical trials have shown that cryoablation works for tumors smaller than 1.5 centimeters, a recent clinical trial at Memorial Sloan Kettering Cancer Center in New York has shown that it can work for larger tumors, too.
In this study, doctors performed cryoablation on patients whose tumors were, on average, 2.5 centimeters. The cryoablation procedure lasted for about 30 minutes, and patients were able to go home on the same day following treatment. Doctors then followed up with the patients after 16 months. In the follow-up, doctors found the recurrence rate for tumors after using cryoablation was only 10 percent.
For patients who don’t qualify for surgery, radiation and hormonal therapy is typically used to treat tumors. However, said Yolanda Brice, M.D., an interventional radiologist at Memorial Sloan Kettering Cancer Center, “when treated with only radiation and hormonal therapy, the tumors will eventually return.” Cryotherapy, Brice said, could be a more effective way to treat cancer for patients who can’t have surgery.
“The fact that we only saw a 10 percent recurrence rate in our study is incredibly promising,” she said.

