These Abortion Drugs Are Proven Safe and Effective. Why Can't Patients Use Them?

Due to federal regulations, access to abortion medications is restricted, despite their record of safety and efficacy.
A few days before Christmas 2015, Paige Alexandria, a 28-year-old counselor at the Austin Women's Health Center in Texas, found out she was pregnant.
Alexandria had missed the cutoff for a medication abortion by three days.
"It was an unplanned pregnancy, and instantaneously I knew I needed an abortion," Alexandria recalls. Already a mother of two children, one with special needs, a third child was not something Alexandria and her husband felt prepared to take on. "Mentally, I knew my limit. I wasn't prepared for a third and I didn't want one," she says.
At an ultrasound appointment one week later, scans showed she was a little over eight weeks pregnant. Alexandria opted to have an abortion as soon as possible, and preferably with medication. "I really wanted to avoid a surgical abortion," she says. "It sounded a lot more invasive, and I'm already uncomfortable with pap smears and pelvic exams, so I initially went in wanting to do the pill."
But at the time, medication guidelines stipulated that one of the pills, called Mifepristone, could only be prescribed to end a pregnancy at eight weeks gestation or earlier – Alexandria had missed the cutoff by three days. If she wanted to end the pregnancy, she would need to undergo a surgical abortion, otherwise known as a vacuum aspiration abortion.
With a vacuum aspiration abortion, doctors dilate the cervix and manually aspirate out the contents of the uterus. Medication abortion, on the other hand, consists of the patient taking two pills – Mifepristone, which blocks the hormones that help the pregnancy develop, and Misoprostol, which empties the uterus over a period of days, identical to a miscarriage.
Alexandria was upset about the change of plans but resolute in her decision to end the pregnancy. "The fact that I didn't really have a choice in how my procedure was performed has made the experience just a little more sensitive for me," she says. She scheduled the earliest available appointment for a surgical abortion.

Paige Alexandria would have chosen to terminate her pregnancy with medication if the regulations were less stringent.
(Photo courtesy of Alexandria)
Like Alexandria, many people looking to terminate a pregnancy opt to do so with medication. According to research from the Guttmacher Institute, medication abortions accounted for nearly 40 percent of all abortions in the year 2017 – a marked increase from 2001, when medication abortions only accounted for roughly five percent of terminations. Taken 24-48 hours apart, Mifepristone and Misoprostol have a 95-99 percent success rate in terminating pregnancies up to 63 days – or nine weeks – of gestation, according to the American College of Obstetrics and Gynecology (ACOG).
But even though the World Health Organization (WHO) considers medical abortion to be highly safe and effective, the medication is still carefully guarded in the United States: Mifepristone is only available for terminating pregnancies up to 10 weeks gestation, per the FDA, even though limited research suggests that both are safe and effective at terminating pregnancies between 12 and 20 weeks.
Additionally, a separate set of regulations known as a Risk Evaluation and Mitigation Strategy (REMS) means that patients can only take Mifepristone under specific circumstances. Mifepristone must be distributed in person by a healthcare provider – usually interpreted in most states as a doctor or nurse practitioner – who has registered with the drug's manufacturer. The medication cannot be distributed through a pharmacy, so doctors who wish to provide the drug must stock the medication in-office, and both the provider and the patient must sign a form that warns them of the "risk of serious complications associated with Mifepristone," according to the FDA.
"REMS is a set of restrictions that the FDA puts on the distribution of drugs it considers dangerous or risky in some way," says Dr. Elizabeth Raymond, an OB-GYN and senior medical associate at Gynuity Health Projects. Although not always called REMS, these restrictions have been imposed on Mifepristone since the medication was approved by the FDA in 2000, Raymond says.
Raymond is part of a growing number of physicians and researchers who want to eliminate the REMS requirements for Mifepristone, also known by its brand name Mifeprex. In 2017, Raymond and several other physicians authored a paper in the New England Journal of Medicine (NEJM) arguing that Mifepristone is extremely safe and needlessly over-regulated.
"When the FDA first approved [Mifepristone] and imposed these requirements, they might have made sense 19 years ago when there was limited information about the use of this treatment in the United States," says Dr. Daniel Grossman, director at Advancing New Standards in Reproductive Health at UCSF and co-author of the 2017 report in the NEJM. "Now, after 19 years, it's clear that this medication is very safe, and safer than a lot of others available in a pharmacy."
Since 2000, Mifepristone has been implicated in 19 deaths, making its mortality rate 0.00063 percent.
According to their research, over three million people have taken Mifepristone since it was approved in 2000. Since then, Mifepristone has been implicated in 19 deaths, making its mortality rate 0.00063 percent. Even then, the risk is inflated, Grossman says.
"The requirement is that practitioners need to report any deaths that occur after taking these medications, and so you'll see deaths included in that figure which are homicides or suicides or something unrelated to taking Mifepristone," says Grossman. In contrast, Acetaminophen – better known as Tylenol – was associated with 458 overdose deaths between 1990 and 1998, as well as 56,000 emergency room visits and 26,000 hospitalizations. Sildenafil, better known as Viagra, was linked to 762 deaths in the first twenty months after it was approved by the FDA. Yet neither Tylenol nor Viagra have been burdened with the same REMS restrictions as Mifepristone.
"It's clearly about more than just the safety of the medication at this point," says Grossman. "It's more about stigma related to abortion and politics."
For people who want a medication abortion, the REMS requirements mean they often need to take off work to schedule a doctor's appointment, arrange for transportation and childcare, and then arrange an additional doctor's appointment days afterward to take the second dose of medication. While surgical abortion procedures are quicker (usually a one-day outpatient procedure, depending on gestation), many people prefer having the abortion in the comfort of their home or surrounded by family instead.
Paige Alexandria, who counsels people seeking abortions at her job, says that survivors of sexual violence often prefer medical abortions to surgical ones. "A lot of time survivors have a trauma associated with medical instruments or having pelvic exams, and so they're more comfortable taking a pill," she says.
But REMS also creates a barrier for healthcare providers, Grossman says. Stocking the medication in-office is "a hassle" and "expensive," while others are reluctant to register their name with the drug manufacturer, fearing harassment or violence from anti-choice protestors. As a result, the number of practitioners willing to provide medical abortions nationwide is severely limited. According to Grossman's own research published in the journal Obstetrics and Gynecology, 28 percent of OBGYNs admitted they would administer medication abortions if it were possible to write a prescription for Mifepristone rather than stock it in-office.
Amazingly, the restrictions on Mifepristone have loosened since it first came on the market. In 2016, the FDA updated the guidelines on Mifepristone to allow its use until 10 weeks gestation, up from eight weeks. But doctors say the REMS restrictions should be eliminated completely so that people can obtain abortions as early as possible.
"REMS restrictions inhibit people from being able to get a timely abortion," says Raymond, who stresses that abortion is generally more comfortable, more affordable, and safer for women the earlier it's done. "Abortion is very safe no matter when you get it, but it's also easier because there's less risk for bleeding, infections, or other complications," Raymond says. Abortions that occur earlier than eight weeks of gestation have a complication rate of less than one percent, while an abortion done at 12 or 13 weeks has a three to six percent chance of complications.
And even for people who want a medication abortion early on in their pregnancy, REMS restrictions make it so that they may not have time to obtain it before the 10-week period lapses, Raymond says.
"If you're seven weeks pregnant but it takes you three weeks to figure out travel and childcare arrangements to go into the doctor and take this medication, now you're at the cutoff date," she says. "Even if you manage to get an abortion at nine weeks, that's still a later gestational age, and so the risks are increased."
In 2016, at a little over nine weeks gestation, Alexandria completed her abortion by having a D&E. But because she didn't have anyone to drive her home after the procedure, she wasn't able to have sedation throughout, something she describes as "traumatic."
"I had the abortion completely aware and coherent, and paired with the fact that I hadn't even wanted a surgical abortion in the first place made it harder to deal with," Alexandria says.
"When you're just a day or two past eight weeks and you want an abortion – why is medication not immediately available?"
Today, Alexandria shares her story publicly to advocate for abortion care. Although she doesn't regret her surgical abortion and acknowledges that not everyone experiences surgical abortion the same way she did, she does wish that she could have gone a different route.
"If I had to do it over, I would still try to do the pill, because [the surgical abortion] was such a terrifying experience," she says. "When you're just a day or two past eight weeks and you want an abortion – why is medication not immediately available? It just doesn't make sense."
Dr. May Edward Chinn, Kizzmekia Corbett, PhD., and Alice Ball, among others, have been behind some of the most important scientific work of the last century.
If you look back on the last century of scientific achievements, you might notice that most of the scientists we celebrate are overwhelmingly white, while scientists of color take a backseat. Since the Nobel Prize was introduced in 1901, for example, no black scientists have landed this prestigious award.
The work of black women scientists has gone unrecognized in particular. Their work uncredited and often stolen, black women have nevertheless contributed to some of the most important advancements of the last 100 years, from the polio vaccine to GPS.
Here are five black women who have changed science forever.
Dr. May Edward Chinn
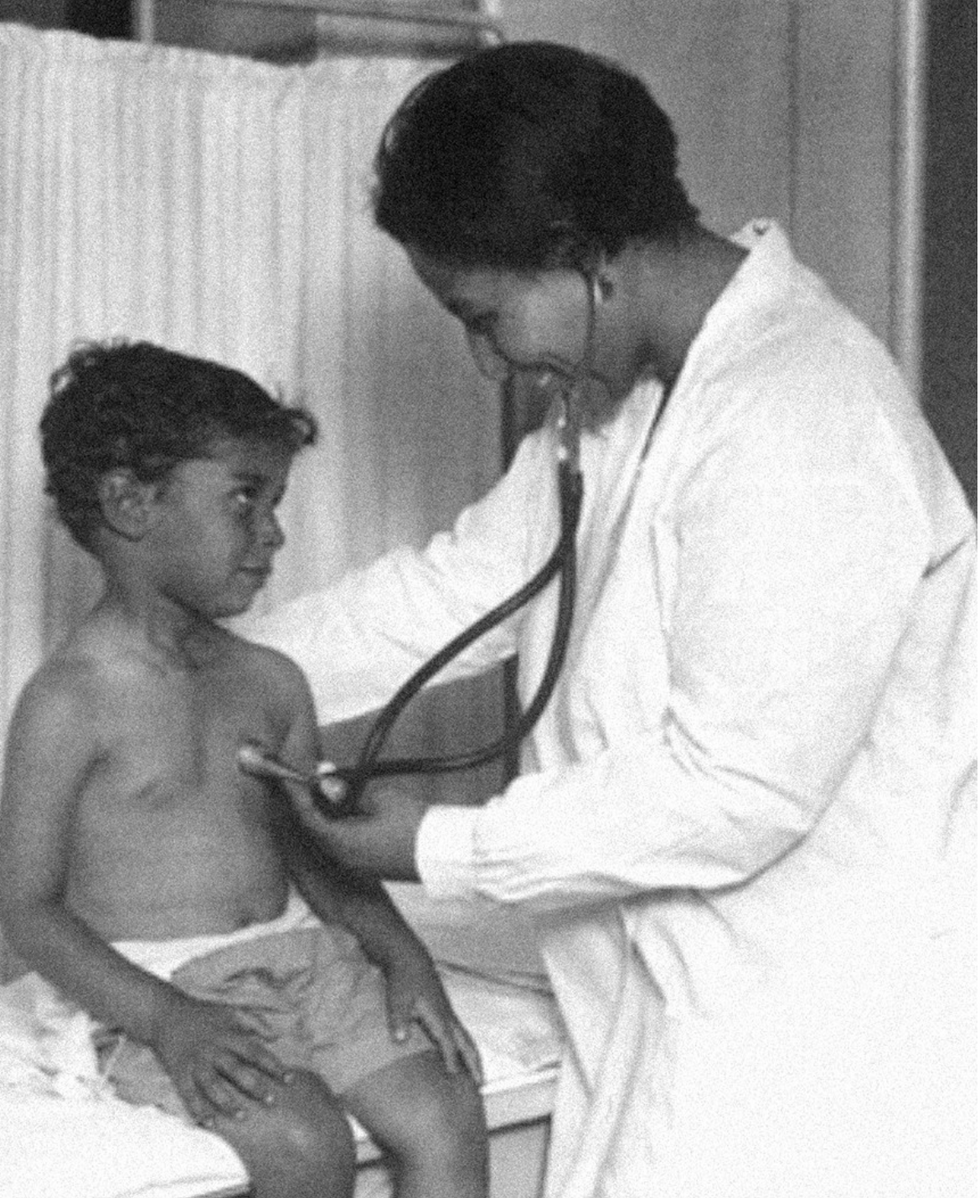
Dr. May Edward Chinn practicing medicine in Harlem
George B. Davis, PhD.
Chinn was born to poor parents in New York City just before the start of the 20th century. Although she showed great promise as a pianist, playing with the legendary musician Paul Robeson throughout the 1920s, she decided to study medicine instead. Chinn, like other black doctors of the time, were barred from studying or practicing in New York hospitals. So Chinn formed a private practice and made house calls, sometimes operating in patients’ living rooms, using an ironing board as a makeshift operating table.
Chinn worked among the city’s poor, and in doing this, started to notice her patients had late-stage cancers that often had gone undetected or untreated for years. To learn more about cancer and its prevention, Chinn begged information off white doctors who were willing to share with her, and even accompanied her patients to other clinic appointments in the city, claiming to be the family physician. Chinn took this information and integrated it into her own practice, creating guidelines for early cancer detection that were revolutionary at the time—for instance, checking patient health histories, checking family histories, performing routine pap smears, and screening patients for cancer even before they showed symptoms. For years, Chinn was the only black female doctor working in Harlem, and she continued to work closely with the poor and advocate for early cancer screenings until she retired at age 81.
Alice Ball

Pictorial Press Ltd/Alamy
Alice Ball was a chemist best known for her groundbreaking work on the development of the “Ball Method,” the first successful treatment for those suffering from leprosy during the early 20th century.
In 1916, while she was an undergraduate student at the University of Hawaii, Ball studied the effects of Chaulmoogra oil in treating leprosy. This oil was a well-established therapy in Asian countries, but it had such a foul taste and led to such unpleasant side effects that many patients refused to take it.
So Ball developed a method to isolate and extract the active compounds from Chaulmoogra oil to create an injectable medicine. This marked a significant breakthrough in leprosy treatment and became the standard of care for several decades afterward.
Unfortunately, Ball died before she could publish her results, and credit for this discovery was given to another scientist. One of her colleagues, however, was able to properly credit her in a publication in 1922.
Henrietta Lacks

onathan Newton/The Washington Post/Getty
The person who arguably contributed the most to scientific research in the last century, surprisingly, wasn’t even a scientist. Henrietta Lacks was a tobacco farmer and mother of five children who lived in Maryland during the 1940s. In 1951, Lacks visited Johns Hopkins Hospital where doctors found a cancerous tumor on her cervix. Before treating the tumor, the doctor who examined Lacks clipped two small samples of tissue from Lacks’ cervix without her knowledge or consent—something unthinkable today thanks to informed consent practices, but commonplace back then.
As Lacks underwent treatment for her cancer, her tissue samples made their way to the desk of George Otto Gey, a cancer researcher at Johns Hopkins. He noticed that unlike the other cell cultures that came into his lab, Lacks’ cells grew and multiplied instead of dying out. Lacks’ cells were “immortal,” meaning that because of a genetic defect, they were able to reproduce indefinitely as long as certain conditions were kept stable inside the lab.
Gey started shipping Lacks’ cells to other researchers across the globe, and scientists were thrilled to have an unlimited amount of sturdy human cells with which to experiment. Long after Lacks died of cervical cancer in 1951, her cells continued to multiply and scientists continued to use them to develop cancer treatments, to learn more about HIV/AIDS, to pioneer fertility treatments like in vitro fertilization, and to develop the polio vaccine. To this day, Lacks’ cells have saved an estimated 10 million lives, and her family is beginning to get the compensation and recognition that Henrietta deserved.
Dr. Gladys West

Andre West
Gladys West was a mathematician who helped invent something nearly everyone uses today. West started her career in the 1950s at the Naval Surface Warfare Center Dahlgren Division in Virginia, and took data from satellites to create a mathematical model of the Earth’s shape and gravitational field. This important work would lay the groundwork for the technology that would later become the Global Positioning System, or GPS. West’s work was not widely recognized until she was honored by the US Air Force in 2018.
Dr. Kizzmekia "Kizzy" Corbett

TIME Magazine
At just 35 years old, immunologist Kizzmekia “Kizzy” Corbett has already made history. A viral immunologist by training, Corbett studied coronaviruses at the National Institutes of Health (NIH) and researched possible vaccines for coronaviruses such as SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome).
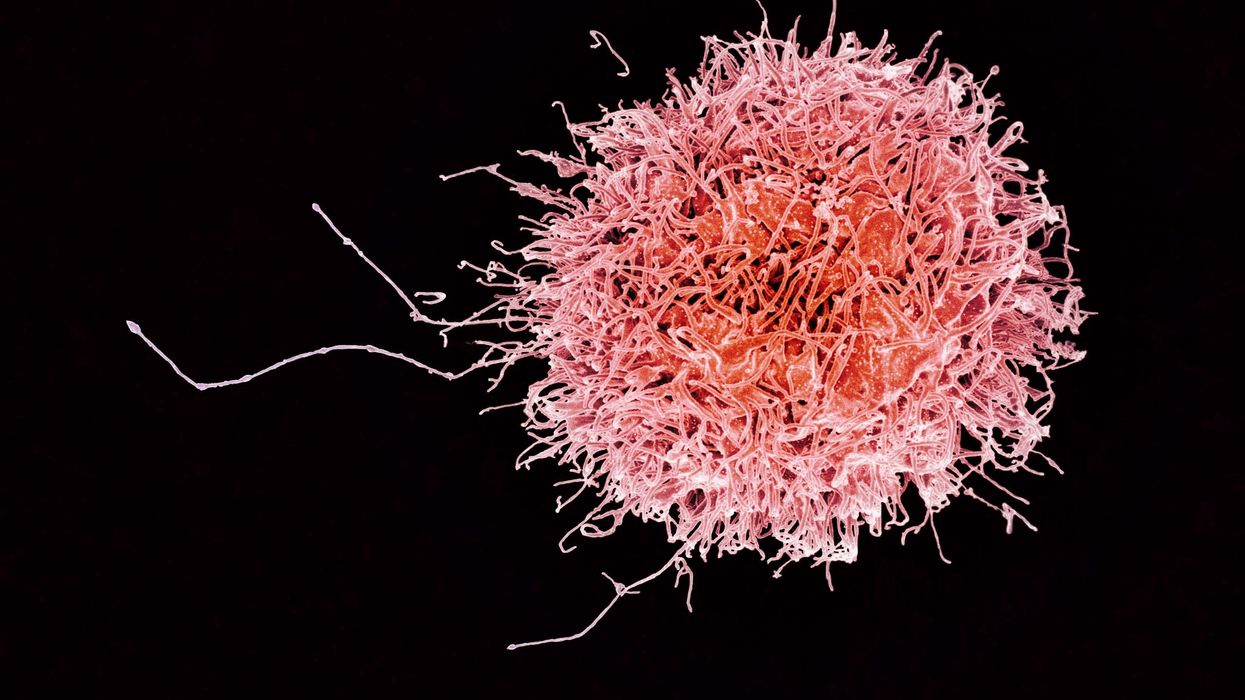
At the start of the COVID pandemic, Corbett and her team at the NIH partnered with pharmaceutical giant Moderna to develop an mRNA-based vaccine against the virus. Corbett’s previous work with mRNA and coronaviruses was vital in developing the vaccine, which became one of the first to be authorized for emergency use in the United States. The vaccine, along with others, is responsible for saving an estimated 14 million lives.On today’s episode of Making Sense of Science, I’m honored to be joined by Dr. Paul Song, a physician, oncologist, progressive activist and biotech chief medical officer. Through his company, NKGen Biotech, Dr. Song is leveraging the power of patients’ own immune systems by supercharging the body’s natural killer cells to make new treatments for Alzheimer’s and cancer.
Whereas other treatments for Alzheimer’s focus directly on reducing the build-up of proteins in the brain such as amyloid and tau in patients will mild cognitive impairment, NKGen is seeking to help patients that much of the rest of the medical community has written off as hopeless cases, those with late stage Alzheimer’s. And in small studies, NKGen has shown remarkable results, even improvement in the symptoms of people with these very progressed forms of Alzheimer’s, above and beyond slowing down the disease.
In the realm of cancer, Dr. Song is similarly setting his sights on another group of patients for whom treatment options are few and far between: people with solid tumors. Whereas some gradual progress has been made in treating blood cancers such as certain leukemias in past few decades, solid tumors have been even more of a challenge. But Dr. Song’s approach of using natural killer cells to treat solid tumors is promising. You may have heard of CAR-T, which uses genetic engineering to introduce cells into the body that have a particular function to help treat a disease. NKGen focuses on other means to enhance the 40 plus receptors of natural killer cells, making them more receptive and sensitive to picking out cancer cells.
Paul Y. Song, MD is currently CEO and Vice Chairman of NKGen Biotech. Dr. Song’s last clinical role was Asst. Professor at the Samuel Oschin Cancer Center at Cedars Sinai Medical Center.
Dr. Song served as the very first visiting fellow on healthcare policy in the California Department of Insurance in 2013. He is currently on the advisory board of the Pritzker School of Molecular Engineering at the University of Chicago and a board member of Mercy Corps, The Center for Health and Democracy, and Gideon’s Promise.
Dr. Song graduated with honors from the University of Chicago and received his MD from George Washington University. He completed his residency in radiation oncology at the University of Chicago where he served as Chief Resident and did a brachytherapy fellowship at the Institute Gustave Roussy in Villejuif, France. He was also awarded an ASTRO research fellowship in 1995 for his research in radiation inducible gene therapy.
With Dr. Song’s leadership, NKGen Biotech’s work on natural killer cells represents cutting-edge science leading to key findings and important pieces of the puzzle for treating two of humanity’s most intractable diseases.
Show links
- Paul Song LinkedIn
- NKGen Biotech on Twitter - @NKGenBiotech
- NKGen Website: https://nkgenbiotech.com/
- NKGen appoints Paul Song
- Patient Story: https://pix11.com/news/local-news/long-island/promising-new-treatment-for-advanced-alzheimers-patients/
- FDA Clearance: https://nkgenbiotech.com/nkgen-biotech-receives-ind-clearance-from-fda-for-snk02-allogeneic-natural-killer-cell-therapy-for-solid-tumors/Q3 earnings data: https://www.nasdaq.com/press-release/nkgen-biotech-inc.-reports-third-quarter-2023-financial-results-and-business