This Mom Donated Her Lost Baby’s Tissue to Research
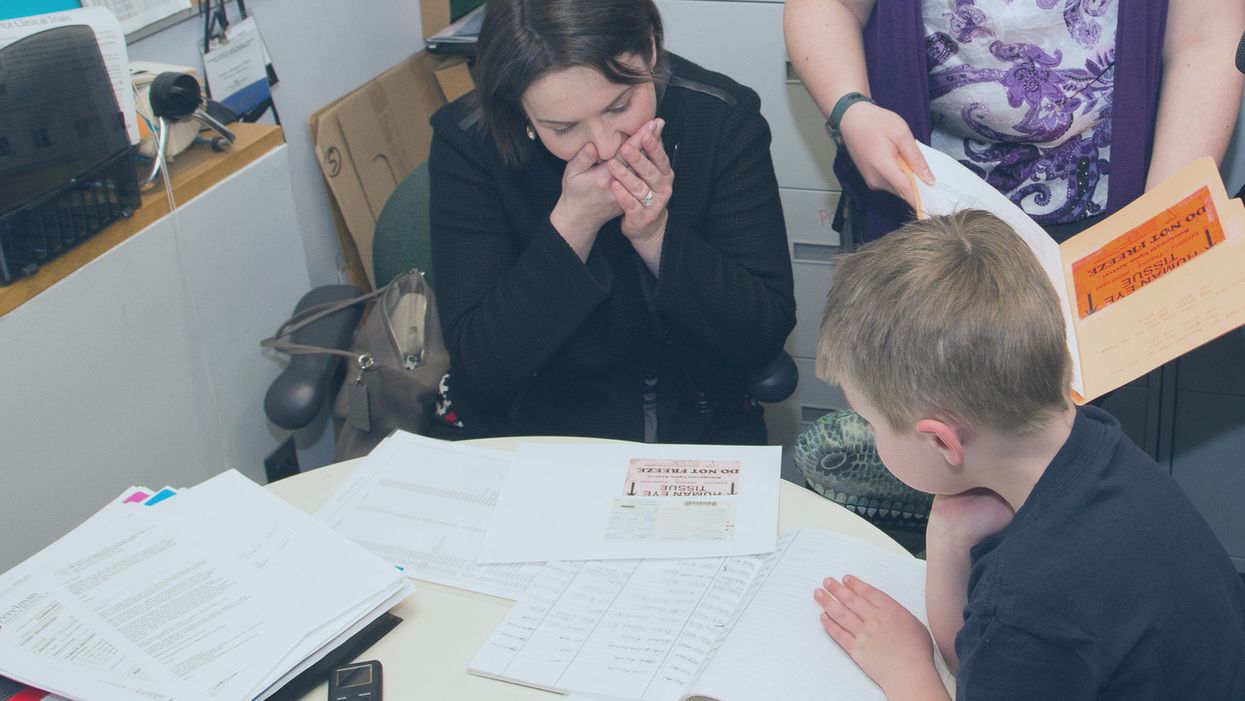
Sarah Gray views data about the use of her deceased son Thomas' retinal tissue in research for retinoblastoma, a cancer of the eye, at the University of Pennsylvania, while her son Callum looks on.
The twin boys growing within her womb filled Sarah Gray with both awe and dread. The sonogram showed that one, Callum, seemed to be the healthy child she and husband Ross had long sought; the other, Thomas, had anencephaly, a fatal developmental disorder of the skull and brain that likely would limit his life to hours. The options were to carry the boys to term or terminate both.
The decision to donate Thomas' tissue to research comforted Sarah. It brought a sense of purpose and meaning to her son's anticipated few breaths.
Sarah learned that researchers prize tissue as essential to better understanding and eventually treating the rare disorder that afflicted her son. And that other tissue from the developing infant might prove useful for transplant or basic research.
Animal models have been useful in figuring out some of the basics of genetics and how the body responds to disease. But a mouse is not a man. The new tools of precision medicine that measure gene expression, proteins and metabolites – the various chemical products and signals that fluctuate in health and illness – are most relevant when studying human tissue directly rather than in animals.
The decision to donate Thomas' tissue to research comforted Sarah. It brought a sense of purpose and meaning to her son's anticipated few breaths.

Thomas Gray
(Photo credit: Mark Walpole)
Later Sarah would track down where some of the donated tissues had been sent and how they were being used. It was a rare initiative that just may spark a new kind of relationship between donor families and researchers who use human tissue.
Organ donation for transplant gets all the attention. That process is simple, direct, life saving, the stories are easy to understand and play out regularly in the media. Reimbursement fully covers costs.
Tissue donation for research is murkier. Seldom is there a direct one-to-one correlation between individual donation and discovery; often hundreds, sometimes thousands of samples are needed to tease out the basic mechanisms of a disease, even more to develop a treatment or cure. The research process can be agonizingly slow. And somebody has to pay for collecting, processing, and getting donations into the hands of appropriate researchers. That story rarely is told, so most people are not even aware it is possible, let alone vital to research.
Gray set out on a quest to follow where Thomas' tissue had gone and how it was being used to advance research and care.
The dichotomy between transplant and research became real for Sarah several months after the birth of her twins, and Thomas' brief life, at a meeting for families of transplant donors. Many of the participants had found closure to their grieving through contact with grateful recipients of a heart, liver, or kidney who had gained a new lease on life. But there was no similar process for those who donated for research. Sarah felt a bit, well, jealous. She wanted that type of connection too.
Gray set out on a quest to follow where Thomas' tissue had gone and how it was being used to advance research and care. Those encounters were as novel for the researchers as they were for Sarah. The experience turned her into an advocate for public education and financial and operational changes to put tissue donation for research on par with donations for transplant.
Thomas' retina had been collected and processed by the National Disease Research Interchange (NDRI), a nonprofit that performs such services for researchers on a cost recovery basis with support from the National Institutes of Health. The tissue was passed on to Arupa Ganguly, who is studying retinoblastoma, a cancer of the eye, at the University of Pennsylvania.
Ganguly was surprised and apprehensive months later when NDRI emailed her saying the mother of donated tissue wanted to learn more about how the retina was being used. That was unusual because research donations generally are anonymous.
The geneticist waited a day or two, then wrote an explanation of her work and forwarded it back through NDRI. Soon the researcher and mother were talking by phone and Sarah would visit the lab. Even then, Ganguly felt very uncomfortable. "Something very bad happened to your son Thomas but it was a benefit for me, so I'm feeling very bad," she told Sarah.
"And Sarah said, Arupa, you were the only ones who wanted his retinas. If you didn't request them, they would be buried in the ground. It gives me a sense of fulfillment to know that they were of some use," Ganguly recalls. And her apprehension melted away. The two became friends and have visited several times.

Sarah Gray visits Dr. Arupa Ganguly at the University of Pennsylvania's Genetic Diagnostic Laboratory.
(Photo credit: Daniel Burke)
Reading Sarah Gray's story led Gregory Grossman to reach out to the young mother and to create Hope and Healing, a program that brings donors and researchers together. Grossman is director of research programs at Eversight, a large network of eye banks that stretches from the Midwest to the East Coast. It supplies tissue for transplant and ocular research.
"Research seems a cold and distant thing," Grossman says, "we need to educate the general public on the importance and need for tissue donations for research, which can help us better understand disease and find treatments."
"Our own internal culture needs to be shifted too," he adds. "Researchers and surgeons can forget that these are precious gifts, they're not a commodity, they're not manufactured. Without people's generosity this doesn't exist."
The initial Hope and Healing meetings between researchers and donor families have gone well and Grossman hopes to increase them to three a year with support from the Lions Club. He sees it as a crucial element in trying to reverse the decline in ocular donations even while research needs continue to grow.
What people hear about is "Tuskegee, Henrietta Lacks, they hear about the scandals, they don't hear about the good news. I would like to change that."
Since writing about her experience in the 2016 book "A Life Everlasting," Gray has come to believe that potential donor families, and even people who administer donation programs, often are unaware of the possibility of donating for research.
And roadblocks are common for those who seek to do so. Just like her, many families have had to be persistent in their quest to donate, and even educate their medical providers. But Sarah believes the internet is facilitating creation of a grassroots movement of empowered donors who are pushing procurement systems to be more responsive to their desires to donate for research. A lot of it comes through anecdote, stories, and people asking, if they have done it in Virginia, or Ohio, why can't we do it here?

Callum Gray and Dr. Arupa Ganguly hug during his family's visit to the lab.
(Photo credit: Daniel Burke)
Gray has spoken at medical and research facilities and at conferences. Some researchers are curious to have contact with the families of donors, but she believes the research system fosters the belief that "you don't want to open that can of worms." And lurking in the background may be a fear of liability issues somehow arising.
"I believe that 99 percent of what happens in research is very positive, and those stories would come out if the connections could be made," says Sarah Gray. But what they hear about is "Tuskegee, Henrietta Lacks, they hear about the scandals, they don't hear about the good news. I would like to change that."
A new type of cancer therapy is shrinking deadly brain tumors with just one treatment
MRI scans after a new kind of immunotherapy for brain cancer show remarkable progress in one patient just days after the first treatment.
Few cancers are deadlier than glioblastomas—aggressive and lethal tumors that originate in the brain or spinal cord. Five years after diagnosis, less than five percent of glioblastoma patients are still alive—and more often, glioblastoma patients live just 14 months on average after receiving a diagnosis.
But an ongoing clinical trial at Mass General Cancer Center is giving new hope to glioblastoma patients and their families. The trial, called INCIPIENT, is meant to evaluate the effects of a special type of immune cell, called CAR-T cells, on patients with recurrent glioblastoma.
How CAR-T cell therapy works
CAR-T cell therapy is a type of cancer treatment called immunotherapy, where doctors modify a patient’s own immune system specifically to find and destroy cancer cells. In CAR-T cell therapy, doctors extract the patient’s T-cells, which are immune system cells that help fight off disease—particularly cancer. These T-cells are harvested from the patient and then genetically modified in a lab to produce proteins on their surface called chimeric antigen receptors (thus becoming CAR-T cells), which makes them able to bind to a specific protein on the patient’s cancer cells. Once modified, these CAR-T cells are grown in the lab for several weeks so that they can multiply into an army of millions. When enough cells have been grown, these super-charged T-cells are infused back into the patient where they can then seek out cancer cells, bind to them, and destroy them. CAR-T cell therapies have been approved by the US Food and Drug Administration (FDA) to treat certain types of lymphomas and leukemias, as well as multiple myeloma, but haven’t been approved to treat glioblastomas—yet.
CAR-T cell therapies don’t always work against solid tumors, such as glioblastomas. Because solid tumors contain different kinds of cancer cells, some cells can evade the immune system’s detection even after CAR-T cell therapy, according to a press release from Massachusetts General Hospital. For the INCIPIENT trial, researchers modified the CAR-T cells even further in hopes of making them more effective against solid tumors. These second-generation CAR-T cells (called CARv3-TEAM-E T cells) contain special antibodies that attack EFGR, a protein expressed in the majority of glioblastoma tumors. Unlike other CAR-T cell therapies, these particular CAR-T cells were designed to be directly injected into the patient’s brain.
The INCIPIENT trial results
The INCIPIENT trial involved three patients who were enrolled in the study between March and July 2023. All three patients—a 72-year-old man, a 74-year-old man, and a 57-year-old woman—were treated with chemo and radiation and enrolled in the trial with CAR-T cells after their glioblastoma tumors came back.
The results, which were published earlier this year in the New England Journal of Medicine (NEJM), were called “rapid” and “dramatic” by doctors involved in the trial. After just a single infusion of the CAR-T cells, each patient experienced a significant reduction in their tumor sizes. Just two days after receiving the infusion, the glioblastoma tumor of the 72-year-old man decreased by nearly twenty percent. Just two months later the tumor had shrunk by an astonishing 60 percent, and the change was maintained for more than six months. The most dramatic result was in the 57-year-old female patient, whose tumor shrank nearly completely after just one infusion of the CAR-T cells.
The results of the INCIPIENT trial were unexpected and astonishing—but unfortunately, they were also temporary. For all three patients, the tumors eventually began to grow back regardless of the CAR-T cell infusions. According to the press release from MGH, the medical team is now considering treating each patient with multiple infusions or prefacing each treatment with chemotherapy to prolong the response.
While there is still “more to do,” says co-author of the study neuro-oncologist Dr. Elizabeth Gerstner, the results are still promising. If nothing else, these second-generation CAR-T cell infusions may someday be able to give patients more time than traditional treatments would allow.
“These results are exciting but they are also just the beginning,” says Dr. Marcela Maus, a doctor and professor of medicine at Mass General who was involved in the clinical trial. “They tell us that we are on the right track in pursuing a therapy that has the potential to change the outlook for this intractable disease.”
A recent study in The Lancet Oncology showed that AI found 20 percent more cancers on mammogram screens than radiologists alone.
Since the early 2000s, AI systems have eliminated more than 1.7 million jobs, and that number will only increase as AI improves. Some research estimates that by 2025, AI will eliminate more than 85 million jobs.
But for all the talk about job security, AI is also proving to be a powerful tool in healthcare—specifically, cancer detection. One recently published study has shown that, remarkably, artificial intelligence was able to detect 20 percent more cancers in imaging scans than radiologists alone.
Published in The Lancet Oncology, the study analyzed the scans of 80,000 Swedish women with a moderate hereditary risk of breast cancer who had undergone a mammogram between April 2021 and July 2022. Half of these scans were read by AI and then a radiologist to double-check the findings. The second group of scans was read by two researchers without the help of AI. (Currently, the standard of care across Europe is to have two radiologists analyze a scan before diagnosing a patient with breast cancer.)
The study showed that the AI group detected cancer in 6 out of every 1,000 scans, while the radiologists detected cancer in 5 per 1,000 scans. In other words, AI found 20 percent more cancers than the highly-trained radiologists.

But even though the AI was better able to pinpoint cancer on an image, it doesn’t mean radiologists will soon be out of a job. Dr. Laura Heacock, a breast radiologist at NYU, said in an interview with CNN that radiologists do much more than simply screening mammograms, and that even well-trained technology can make errors. “These tools work best when paired with highly-trained radiologists who make the final call on your mammogram. Think of it as a tool like a stethoscope for a cardiologist.”
AI is still an emerging technology, but more and more doctors are using them to detect different cancers. For example, researchers at MIT have developed a program called MIRAI, which looks at patterns in patient mammograms across a series of scans and uses an algorithm to model a patient's risk of developing breast cancer over time. The program was "trained" with more than 200,000 breast imaging scans from Massachusetts General Hospital and has been tested on over 100,000 women in different hospitals across the world. According to MIT, MIRAI "has been shown to be more accurate in predicting the risk for developing breast cancer in the short term (over a 3-year period) compared to traditional tools." It has also been able to detect breast cancer up to five years before a patient receives a diagnosis.
The challenges for cancer-detecting AI tools now is not just accuracy. AI tools are also being challenged to perform consistently well across different ages, races, and breast density profiles, particularly given the increased risks that different women face. For example, Black women are 42 percent more likely than white women to die from breast cancer, despite having nearly the same rates of breast cancer as white women. Recently, an FDA-approved AI device for screening breast cancer has come under fire for wrongly detecting cancer in Black patients significantly more often than white patients.
As AI technology improves, radiologists will be able to accurately scan a more diverse set of patients at a larger volume than ever before, potentially saving more lives than ever.

