To Make Science Engaging, We Need a Sesame Street for Adults
A new kind of television series could establish the baseline narratives for novel science like gene editing, quantum computing, or artificial intelligence.
This article is part of the magazine, "The Future of Science In America: The Election Issue," co-published by LeapsMag, the Aspen Institute Science & Society Program, and GOOD.
In the mid-1960s, a documentary producer in New York City wondered if the addictive jingles, clever visuals, slogans, and repetition of television ads—the ones that were captivating young children of the time—could be harnessed for good. Over the course of three months, she interviewed educators, psychologists, and artists, and the result was a bonanza of ideas.
Perhaps a new TV show could teach children letters and numbers in short animated sequences? Perhaps adults and children could read together with puppets providing comic relief and prompting interaction from the audience? And because it would be broadcast through a device already in almost every home, perhaps this show could reach across socioeconomic divides and close an early education gap?
Soon after Joan Ganz Cooney shared her landmark report, "The Potential Uses of Television in Preschool Education," in 1966, she was prototyping show ideas, attracting funding from The Carnegie Corporation, The Ford Foundation, and The Corporation for Public Broadcasting, and co-founding the Children's Television Workshop with psychologist Lloyd Morrisett. And then, on November 10, 1969, informal learning was transformed forever with the premiere of Sesame Street on public television.
For its first season, Sesame Street won three Emmy Awards and a Peabody Award. Its star, Big Bird, landed on the cover of Time Magazine, which called the show "TV's gift to children." Fifty years later, it's hard to imagine an approach to informal preschool learning that isn't Sesame Street.
And that approach can be boiled down to one word: Entertainment.
Despite decades of evidence from Sesame Street—one of the most studied television shows of all time—and more research from social science, psychology, and media communications, we haven't yet taken Ganz Cooney's concepts to heart in educating adults. Adults have news programs and documentaries and educational YouTube channels, but no Sesame Street. So why don't we? Here's how we can design a new kind of television to make science engaging and accessible for a public that is all too often intimidated by it.
We have to start from the realization that America is a nation of high-school graduates. By the end of high school, students have decided to abandon science because they think it's too difficult, and as a nation, we've made it acceptable for any one of us to say "I'm not good at science" and offload thinking to the ones who might be. So, is it surprising that a large number of Americans are likely to believe in conspiracy theories like the 25% that believe the release of COVID-19 was planned, the one in ten who believe the Moon landing was a hoax, or the 30–40% that think the condensation trails of planes are actually nefarious chemtrails? If we're meeting people where they are, the aim can't be to get the audience from an A to an A+, but from an F to a D, and without judgment of where they are starting from.
There's also a natural compulsion for a well-meaning educator to fill a literacy gap with a barrage of information, but this is what I call "factsplaining," and we know it doesn't work. And worse, it can backfire. In one study from 2014, parents were provided with factual information about vaccine safety, and it was the group that was already the most averse to vaccines that uniquely became even more averse.
Why? Our social identities and cognitive biases are stubborn gatekeepers when it comes to processing new information. We filter ideas through pre-existing beliefs—our values, our religions, our political ideologies. Incongruent ideas are rejected. Congruent ideas, no matter how absurd, are allowed through. We hear what we want to hear, and then our brains justify the input by creating narratives that preserve our identities. Even when we have all the facts, we can use them to support any worldview.
But social science has revealed many mechanisms for hijacking these processes through narrative storytelling, and this can form the foundation of a new kind of educational television.
Could new television series establish the baseline narratives for novel science like gene editing, quantum computing, or artificial intelligence?
As media creators, we can reject factsplaining and instead construct entertaining narratives that disrupt cognitive processes. Two-decade-old research tells us when people are immersed in entertaining fiction narratives, they loosen their defenses, opening a path for new information, editing attitudes, and inspiring new behavior. Where news about hot-button issues like climate change or vaccination might trigger resistance or a backfire effect, fiction can be crafted to be absorbing and, as a result, persuasive.
But the narratives can't be stuffed with information. They must be simplified. If this feels like the opposite of what an educator should be doing, it is possible to reduce the complexity of information, without oversimplification, through "exemplification," a framing device to tell the stories of individuals in specific circumstances that can speak to the greater issue without needing to explain it all. It's a technique you've seen used in biopics. The Discovery Channel true-crime miniseries Manhunt: Unabomber does many things well from a science storytelling perspective, including exemplifying the virtues of the scientific method through a character who argues for a new field of science, forensic linguistics, to catch one of the most notorious domestic terrorists in U.S. history.
We must also appeal to the audience's curiosity. We know curiosity is such a strong driver of human behavior that it can even counteract the biases put up by one's political ideology around subjects like climate change. If we treat science information like a product—and we should—advertising research tells us we can maximize curiosity though a Goldilocks effect. If the information is too complex, your show might as well be a PowerPoint presentation. If it's too simple, it's Sesame Street. There's a sweet spot for creating intrigue about new information when there's a moderate cognitive gap.
The science of "identification" tells us that the more the main character is endearing to a viewer, the more likely the viewer will adopt the character's worldview and journey of change. This insight further provides incentives to craft characters reflective of our audiences. If we accept our biases for what they are, we can understand why the messenger becomes more important than the message, because, without an appropriate messenger, the message becomes faint and ineffective. And research confirms that the stereotype-busting doctor-skeptic Dana Scully of The X-Files, a popular science-fiction series, was an inspiration for a generation of women who pursued science careers.
With these directions, we can start making a new kind of television. But is television itself still the right delivery medium? Americans do spend six hours per day—a quarter of their lives—watching video. And even with the rise of social media and apps, science-themed television shows remain popular, with four out of five adults reporting that they watch shows about science at least sometimes. CBS's The Big Bang Theory was the most-watched show on television in the 2017–2018 season, and Cartoon Network's Rick & Morty is the most popular comedy series among millennials. And medical and forensic dramas continue to be broadcast staples. So yes, it's as true today as it was in the 1980s when George Gerbner, the "cultivation theory" researcher who studied the long-term impacts of television images, wrote, "a single episode on primetime television can reach more people than all science and technology promotional efforts put together."
We know from cultivation theory that media images can shape our views of scientists. Quick, picture a scientist! Was it an old, white man with wild hair in a lab coat? If most Americans don't encounter research science firsthand, it's media that dictates how we perceive science and scientists. Characters like Sheldon Cooper and Rick Sanchez become the model. But we can correct that by representing professionals more accurately on-screen and writing characters more like Dana Scully.
Could new television series establish the baseline narratives for novel science like gene editing, quantum computing, or artificial intelligence? Or could new series counter the misinfodemics surrounding COVID-19 and vaccines through more compelling, corrective narratives? Social science has given us a blueprint suggesting they could. Binge-watching a show like the surreal NBC sitcom The Good Place doesn't replace a Ph.D. in philosophy, but its use of humor plants the seed of continued interest in a new subject. The goal of persuasive entertainment isn't to replace formal education, but it can inspire, shift attitudes, increase confidence in the knowledge of complex issues, and otherwise prime viewers for continued learning.
[Editor's Note: To read other articles in this special magazine issue, visit the beautifully designed e-reader version.]
Bobby Brooke Herrera, the co-founder and CEO of e25Bio, demonstrates the company's rapid paper-strip test for detecting the coronavirus.
You're lying in bed late at night, the foggy swirl of the pandemic's 8th month just beginning to fall behind you, when you detect a slight tickle at the back of your throat.
"If half of people choose to use these tests every other day, then we can stop transmission faster than a vaccine can."
Suddenly fully awake, a jolt of panicked electricity races through your body. Has COVID-19 come for you? In the U.S., answering this simple question is incredibly difficult.
Now, you might have to wait for hours in line in your car to get a test for $100, only to find out your result 10-14 days later -- much too late to matter in stopping an outbreak. Due to such obstacles, a recent report in JAMA Internal Medicine estimated that 9 out of 10 infections in the U.S. are being missed.
But what if you could use a paper strip in the privacy of your own home, like a pregnancy test, and find out if you are contagious in real time?
e25 Bio, a small company in Cambridge, Mass., has already created such a test and it has been sitting on a lab bench, inaccessible, since April. It is an antigen test, which looks for proteins on the outside of a virus, and can deliver results in about 15 minutes. Also like an over-the-counter pregnancy test, e25 envisions its paper strips as a public health screening tool, rather than a definitive diagnostic test. People who see a positive result would be encouraged to then seek out a physician-administered, gold-standard diagnostic test: the more sensitive PCR.
Typically, hospitals and other health facilities rely on PCR tests to diagnose viruses. This test can detect small traces of genetic material that a virus leaves behind in the human body, which tells a clinician that the patient is either actively infected with or recently cleared that virus. PCR is quite sensitive, meaning that it is able to detect the presence of a virus' genetic material very accurately.
But although PCR is the gold-standard for diagnostics, it's also the most labor-intensive way to test for a virus and takes a relatively long time to produce results. That's not a good match for stopping super-spreader events during an unchecked pandemic. PCR is also not great at identifying the infected people when they are most at risk of potentially transmitting the virus to others.
That's because the viral threshold at which PCR can detect a positive result is so low, that it's actually too sensitive for the purposes of telling whether someone is contagious.
"The majority of time someone is PCR positive, those [genetic] remnants do not indicate transmissible virus," epidemiologist Michael Mina recently Tweeted. "They indicate remnants of a recently cleared infection."
To stop the chain of transmission for COVID-19, he says, "We need a more accurate test than PCR, that turns positive when someone is able to transmit."
In other words, we need a test that is better at detecting whether a person is contagious, as opposed to whether a small amount of virus can be detected in their nose or saliva. This kind of test is especially critical given the research showing that asymptomatic and pre-symptomatic people have high viral loads and are spreading the virus undetected.
The critical question for contagiousness testing, then, is how big a dose of SARS-CoV-2, the virus that causes COVID, does it take to infect most people? Researchers are still actively trying to answer this. As Angela Rasmussen, a coronavirus expert at Columbia University, told STAT: "We don't know the amount that is required to cause an infection, but it seems that it's probably not a really, really small amount, like measles."
Amesh Adalja, an infectious disease physician and a senior scholar at the Johns Hopkins University Center for Health Security, told LeapsMag: "It's still unclear what viral load is associated with contagiousness but it is biologically plausible that higher viral loads, in general, are associated with more efficient transmission especially in symptomatic individuals. In those without symptoms, however, the same relationship may not hold and this may be one of the reasons young children, despite their high viral loads, are not driving outbreaks."
"Antigen tests work best when there's high viral loads. They're catching people who are super spreaders."
Mina and colleagues estimate that widespread use of weekly cheap, rapid tests that are 100 times less sensitive than PCR tests would prevent outbreaks -- as long as the people who are positive self-isolate.
So why can't we buy e25Bio's test at a drugstore right now? Ironically, it's barred for the very reason that it's useful in the first place: Because it is not sensitive enough to satisfy the U.S. Food and Drug Administration, according to the company.
"We're ready to go," says Carlos-Henri Ferré, senior associate of operations and communications at e25. "We've applied to FDA, and now it's in their hands."
The problem, he said, is that the FDA is evaluating applications for antigen tests based on criteria for assessing diagnostics, like PCR, even when the tests serve a different purpose -- as a screening tool.
"Antigen tests work best when there's high viral loads," Ferré says. "They're catching people who are super spreaders, that are capable of continuing the spread of disease … FDA criteria is for diagnostics and not this."
FDA released guidance on July 29th -- 140 days into the pandemic -- recommending that at-home tests should perform with at least 80 percent sensitivity if ordered by prescription, and at least 90 percent sensitivity if purchased over the counter. "The danger of a false negative result is that it can contribute to the spread of COVID-19," according to an FDA spokesperson. "However, oversight of a health care professional who reviews the results, in combination with the patient's symptoms and uses their clinical judgment to recommend additional testing, if needed, among other things, can help mitigate some risks."
Crucially, the 90 percent sensitivity recommendation is judged upon comparison to PCR tests, meaning that if a PCR test is able to detect virus in 100 samples, the at-home antigen test would need to detect virus in at least 90 of those samples. Since antigen tests only detect high viral loads, frustrated critics like Mina say that such guidance is "unreasonable."
"The FDA at this moment is not understanding the true potential for wide-scale frequent testing. In some ways this is not their fault," Mina told LeapsMag. "The FDA does not have any remit to evaluate tests that fall outside of medical diagnostic testing. The proposal I have put forth is not about diagnostic testing (leave that for symptomatic cases reporting to their physician and getting PCR tests)....Daily rapid tests are not about diagnosing people and they are not about public health surveillance and they are not about passports to go to school, out to dinner or into the office. They are about reducing population-level transmission given a similar approach as vaccines."
A reasonable standard, he added, would be to follow the World Health Organization's Target Product Profiles, which are documents to help developers build desirable and minimally acceptable testing products. "A decent limit," Mina says, "is a 70% or 80% sensitivity (if they truly require sensitivity as a metric) to detect virus at Ct values less than 25. This coincides with detection of the most transmissible people, which is important."
(A Ct value is a type of measurement that corresponds inversely to the amount of viral load in a given sample. Researchers have found that Ct values of 13-17 indicate high viral load, whereas Ct values greater than 34 indicate a lack of infectious virus.)
"We believe this should be an at-home test, but [if FDA approval comes through] the first rollout is to do this in laboratories, hospitals, and clinics."
"We believe that population screening devices have an immediate place and use in helping beat the virus," says Ferré. "You can have a significant impact even with a test at 60% sensitivity if you are testing frequently."
When presented with criticism of its recommendations, the FDA indicated that it will not automatically deny any at-home test that fails to meet the 90 percent sensitivity guidance.
"FDA is always open to alternative proposals from developers, including strategies for serial testing with less sensitive tests," a spokesperson wrote in a statement. "For example, it is possible that overall sensitivity of the strategy could be considered cumulatively rather than based on one-time testing….In the case of a manufacturer with an at-home test that can only detect people with COVID-19 when they have a high viral load, we encourage them to talk with us so we can better understand their test, how they propose to use it, and the validation data they have collected to support that use."
However, the FDA's actions so far conflict with its stated openness. e25 ended up adding a step to the protocol in order to better meet FDA standards for sensitivity, but that extra step—sending samples to a laboratory for results—will undercut the test's ability to work as an at-home screening tool.
"We believe this should be an at-home test, but [if FDA approval comes through] the first rollout is to do this in laboratories, hospitals, and clinics," Ferré says.
According to the FDA, no test developers have approached them with a request for an emergency use authorization that proposes an alternate testing paradigm, such as serial testing, to mitigate test sensitivity below 80 percent.
From a scientific perspective, antigen tests like e25Bio's are not the only horse in the race for a simple rapid test with potential for at-home use. CRISPR technology has long been touted as fertile ground for diagnostics, and in an eerily prescient interview with LeapsMag in November, CRISPR pioneer Feng Zhang spoke of its potential application as an at-home diagnostic for an infectious disease specifically.
"I think in the long run it will be great to see this for, say, at-home disease testing, for influenza and other sorts of important public health [concerns]," he said in the fall. "To be able to get a readout at home, people can potentially quarantine themselves rather than traveling to a hospital and then carrying the risk of spreading that disease to other people as they get to the clinic."
Zhang's company Sherlock Biosciences is now working on scaled-up manufacturing of a test to detect SARS CoV-2. Mammoth Biosciences, which secured funding from the National Institutes of Health's Rapid Acceleration of Diagnostics program, is also working on a CRISPR diagnostic for SARS CoV-2. Both would check the box for rapid testing, but so far not for at-home testing, as they would also require laboratory infrastructure to provide results.
If any at-home tests can clear the regulatory hurdles, they would also need to be manufactured on a large scale and be cheap enough to entice people to actually use them. In the world of at-home diagnostics, pregnancy tests have become the sole mainstream victor because they're simple to use, small to carry, easy to interpret, and costs about seven or eight dollars at any ubiquitous store, like Target or Walmart. By comparison, the at-home COVID collection tests that don't even offer diagnostics—you send away your sample to an external lab—all cost over $100 to take just one time.
For the time being, the only available diagnostics for COVID require a lab or an expensive dedicated machine to process. This disconnect could prolong the world's worst health crisis in a century.
"Daily rapid tests have enormous potential to sever transmission chains and create herd effects similar to herd immunity," Mina says. "We all recognize that vaccines and infections can result in herd immunity when something around half of people are no longer susceptible.
"The same thing exists with these tests. These are the intervention to stop the virus. If half of people choose to use these tests every other day, then we can stop transmission faster than a vaccine can. The technology exists, the theory and mathematics back it up, the epidemiology is sound. There is no reason we are not approaching this as strongly as we would be approaching vaccines."
--Additional reporting by Julia Sklar
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Coronavirus Risk Calculators: What You Need to Know
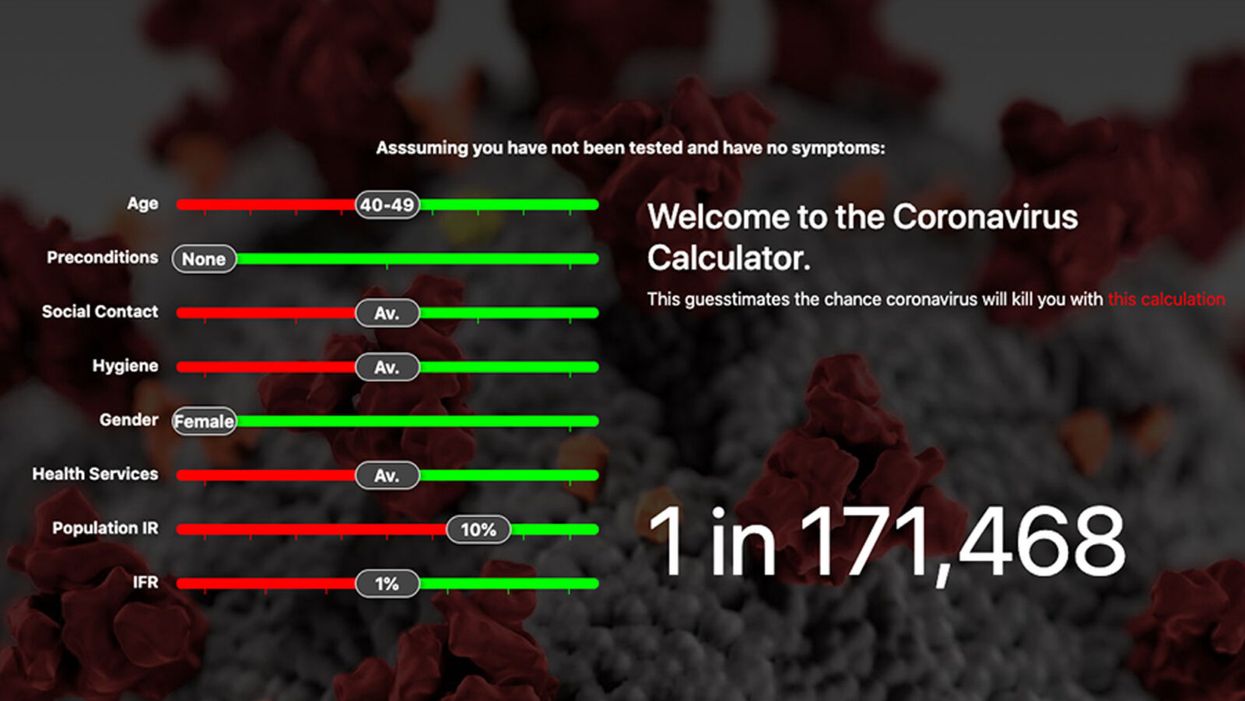
A screenshot of one coronavirus risk calculator.
People in my family seem to develop every ailment in the world, including feline distemper and Dutch elm disease, so I naturally put fingers to keyboard when I discovered that COVID-19 risk calculators now exist.
"It's best to look at your risk band. This will give you a more useful insight into your personal risk."
But the results – based on my answers to questions -- are bewildering.
A British risk calculator developed by the Nexoid software company declared I have a 5 percent, or 1 in 20, chance of developing COVID-19 and less than 1 percent risk of dying if I get it. Um, great, I think? Meanwhile, 19 and Me, a risk calculator created by data scientists, says my risk of infection is 0.01 percent per week, or 1 in 10,000, and it gave me a risk score of 44 out of 100.
Confused? Join the club. But it's actually possible to interpret numbers like these and put them to use. Here are five tips about using coronavirus risk calculators:
1. Make Sure the Calculator Is Designed For You
Not every COVID-19 risk calculator is designed to be used by the general public. Cleveland Clinic's risk calculator, for example, is only a tool for medical professionals, not sick people or the "worried well," said Dr. Lara Jehi, Cleveland Clinic's chief research information officer.
Unfortunately, the risk calculator's web page fails to explicitly identify its target audience. But there are hints that it's not for lay people such as its references to "platelets" and "chlorides."
The 19 and Me or the Nexoid risk calculators, in contrast, are both designed for use by everyone, as is a risk calculator developed by Emory University.
2. Take a Look at the Calculator's Privacy Policy
COVID-19 risk calculators ask for a lot of personal information. The Nexoid calculator, for example, wanted to know my age, weight, drug and alcohol history, pre-existing conditions, blood type and more. It even asked me about the prescription drugs I take.
It's wise to check the privacy policy and be cautious about providing an email address or other personal information. Nexoid's policy says it provides the information it gathers to researchers but it doesn't release IP addresses, which can reveal your location in certain circumstances.
John-Arne Skolbekken, a professor and risk specialist at Norwegian University of Science and Technology, entered his own data in the Nexoid calculator after being contacted by LeapsMag for comment. He noted that the calculator, among other things, asks for information about use of recreational drugs that could be illegal in some places. "I have given away some of my personal data to a company that I can hope will not misuse them," he said. "Let's hope they are trustworthy."
The 19 and Me calculator, by contrast, doesn't gather any data from users, said Cindy Hu, data scientist at Mathematica, which created it. "As soon as the window is closed, that data is gone and not captured."
The Emory University risk calculator, meanwhile, has a long privacy policy that states "the information we collect during your assessment will not be correlated with contact information if you provide it." However, it says personal information can be shared with third parties.
3. Keep an Eye on Time Horizons
Let's say a risk calculator says you have a 1 percent risk of infection. That's fairly low if we're talking about this year as a whole, but it's quite worrisome if the risk percentage refers to today and jumps by 1 percent each day going forward. That's why it's helpful to know exactly what the numbers mean in terms of time.
Unfortunately, this information isn't always readily available. You may have to dig around for it or contact a risk calculator's developers for more information. The 19 and Me calculator's risk percentages refer to this current week based on your behavior this week, Hu said. The Nexoid calculator, by contrast, has an "infinite timeline" that assumes no vaccine is developed, said Jonathon Grantham, the company's managing director. But your results will vary over time since the calculator's developers adjust it to reflect new data.
When you use a risk calculator, focus on this question: "How does your risk compare to the risk of an 'average' person?"
4. Focus on the Big Picture
The Nexoid calculator gave me numbers of 5 percent (getting COVID-19) and 99.309 percent (surviving it). It even provided betting odds for gambling types: The odds are in favor of me not getting infected (19-to-1) and not dying if I get infected (144-to-1).
However, Grantham told me that these numbers "are not the whole story." Instead, he said, "it's best to look at your risk band. This will give you a more useful insight into your personal risk." Risk bands refer to a segmentation of people into five categories, from lowest to highest risk, according to how a person's result sits relative to the whole dataset.
The Nexoid calculator says I'm in the "lowest risk band" for getting COVID-19, and a "high risk band" for dying of it if I get it. That suggests I'd better stay in the lowest-risk category because my pre-existing risk factors could spell trouble for my survival if I get infected.
Michael J. Pencina, a professor and biostatistician at Duke University School of Medicine, agreed that focusing on your general risk level is better than focusing on numbers. When you use a risk calculator, he said, focus on this question: "How does your risk compare to the risk of an 'average' person?"
The 19 and Me calculator, meanwhile, put my risk at 44 out of 100. Hu said that a score of 50 represents the typical person's risk of developing serious consequences from another disease – the flu.
5. Remember to Take Action
Hu, who helped develop the 19 and Me risk calculator, said it's best to use it to "understand the relative impact of different behaviors." As she noted, the calculator is designed to allow users to plug in different answers about their behavior and immediately see how their risk levels change.
This information can help us figure out if we should change the way we approach the world by, say, washing our hands more or avoiding more personal encounters.
"Estimation of risk is only one part of prevention," Pencina said. "The other is risk factors and our ability to reduce them." In other words, odds, percentages and risk bands can be revealing, but it's what we do to change them that matters.