To Make Science Engaging, We Need a Sesame Street for Adults
A new kind of television series could establish the baseline narratives for novel science like gene editing, quantum computing, or artificial intelligence.
This article is part of the magazine, "The Future of Science In America: The Election Issue," co-published by LeapsMag, the Aspen Institute Science & Society Program, and GOOD.
In the mid-1960s, a documentary producer in New York City wondered if the addictive jingles, clever visuals, slogans, and repetition of television ads—the ones that were captivating young children of the time—could be harnessed for good. Over the course of three months, she interviewed educators, psychologists, and artists, and the result was a bonanza of ideas.
Perhaps a new TV show could teach children letters and numbers in short animated sequences? Perhaps adults and children could read together with puppets providing comic relief and prompting interaction from the audience? And because it would be broadcast through a device already in almost every home, perhaps this show could reach across socioeconomic divides and close an early education gap?
Soon after Joan Ganz Cooney shared her landmark report, "The Potential Uses of Television in Preschool Education," in 1966, she was prototyping show ideas, attracting funding from The Carnegie Corporation, The Ford Foundation, and The Corporation for Public Broadcasting, and co-founding the Children's Television Workshop with psychologist Lloyd Morrisett. And then, on November 10, 1969, informal learning was transformed forever with the premiere of Sesame Street on public television.
For its first season, Sesame Street won three Emmy Awards and a Peabody Award. Its star, Big Bird, landed on the cover of Time Magazine, which called the show "TV's gift to children." Fifty years later, it's hard to imagine an approach to informal preschool learning that isn't Sesame Street.
And that approach can be boiled down to one word: Entertainment.
Despite decades of evidence from Sesame Street—one of the most studied television shows of all time—and more research from social science, psychology, and media communications, we haven't yet taken Ganz Cooney's concepts to heart in educating adults. Adults have news programs and documentaries and educational YouTube channels, but no Sesame Street. So why don't we? Here's how we can design a new kind of television to make science engaging and accessible for a public that is all too often intimidated by it.
We have to start from the realization that America is a nation of high-school graduates. By the end of high school, students have decided to abandon science because they think it's too difficult, and as a nation, we've made it acceptable for any one of us to say "I'm not good at science" and offload thinking to the ones who might be. So, is it surprising that a large number of Americans are likely to believe in conspiracy theories like the 25% that believe the release of COVID-19 was planned, the one in ten who believe the Moon landing was a hoax, or the 30–40% that think the condensation trails of planes are actually nefarious chemtrails? If we're meeting people where they are, the aim can't be to get the audience from an A to an A+, but from an F to a D, and without judgment of where they are starting from.
There's also a natural compulsion for a well-meaning educator to fill a literacy gap with a barrage of information, but this is what I call "factsplaining," and we know it doesn't work. And worse, it can backfire. In one study from 2014, parents were provided with factual information about vaccine safety, and it was the group that was already the most averse to vaccines that uniquely became even more averse.
Why? Our social identities and cognitive biases are stubborn gatekeepers when it comes to processing new information. We filter ideas through pre-existing beliefs—our values, our religions, our political ideologies. Incongruent ideas are rejected. Congruent ideas, no matter how absurd, are allowed through. We hear what we want to hear, and then our brains justify the input by creating narratives that preserve our identities. Even when we have all the facts, we can use them to support any worldview.
But social science has revealed many mechanisms for hijacking these processes through narrative storytelling, and this can form the foundation of a new kind of educational television.
Could new television series establish the baseline narratives for novel science like gene editing, quantum computing, or artificial intelligence?
As media creators, we can reject factsplaining and instead construct entertaining narratives that disrupt cognitive processes. Two-decade-old research tells us when people are immersed in entertaining fiction narratives, they loosen their defenses, opening a path for new information, editing attitudes, and inspiring new behavior. Where news about hot-button issues like climate change or vaccination might trigger resistance or a backfire effect, fiction can be crafted to be absorbing and, as a result, persuasive.
But the narratives can't be stuffed with information. They must be simplified. If this feels like the opposite of what an educator should be doing, it is possible to reduce the complexity of information, without oversimplification, through "exemplification," a framing device to tell the stories of individuals in specific circumstances that can speak to the greater issue without needing to explain it all. It's a technique you've seen used in biopics. The Discovery Channel true-crime miniseries Manhunt: Unabomber does many things well from a science storytelling perspective, including exemplifying the virtues of the scientific method through a character who argues for a new field of science, forensic linguistics, to catch one of the most notorious domestic terrorists in U.S. history.
We must also appeal to the audience's curiosity. We know curiosity is such a strong driver of human behavior that it can even counteract the biases put up by one's political ideology around subjects like climate change. If we treat science information like a product—and we should—advertising research tells us we can maximize curiosity though a Goldilocks effect. If the information is too complex, your show might as well be a PowerPoint presentation. If it's too simple, it's Sesame Street. There's a sweet spot for creating intrigue about new information when there's a moderate cognitive gap.
The science of "identification" tells us that the more the main character is endearing to a viewer, the more likely the viewer will adopt the character's worldview and journey of change. This insight further provides incentives to craft characters reflective of our audiences. If we accept our biases for what they are, we can understand why the messenger becomes more important than the message, because, without an appropriate messenger, the message becomes faint and ineffective. And research confirms that the stereotype-busting doctor-skeptic Dana Scully of The X-Files, a popular science-fiction series, was an inspiration for a generation of women who pursued science careers.
With these directions, we can start making a new kind of television. But is television itself still the right delivery medium? Americans do spend six hours per day—a quarter of their lives—watching video. And even with the rise of social media and apps, science-themed television shows remain popular, with four out of five adults reporting that they watch shows about science at least sometimes. CBS's The Big Bang Theory was the most-watched show on television in the 2017–2018 season, and Cartoon Network's Rick & Morty is the most popular comedy series among millennials. And medical and forensic dramas continue to be broadcast staples. So yes, it's as true today as it was in the 1980s when George Gerbner, the "cultivation theory" researcher who studied the long-term impacts of television images, wrote, "a single episode on primetime television can reach more people than all science and technology promotional efforts put together."
We know from cultivation theory that media images can shape our views of scientists. Quick, picture a scientist! Was it an old, white man with wild hair in a lab coat? If most Americans don't encounter research science firsthand, it's media that dictates how we perceive science and scientists. Characters like Sheldon Cooper and Rick Sanchez become the model. But we can correct that by representing professionals more accurately on-screen and writing characters more like Dana Scully.
Could new television series establish the baseline narratives for novel science like gene editing, quantum computing, or artificial intelligence? Or could new series counter the misinfodemics surrounding COVID-19 and vaccines through more compelling, corrective narratives? Social science has given us a blueprint suggesting they could. Binge-watching a show like the surreal NBC sitcom The Good Place doesn't replace a Ph.D. in philosophy, but its use of humor plants the seed of continued interest in a new subject. The goal of persuasive entertainment isn't to replace formal education, but it can inspire, shift attitudes, increase confidence in the knowledge of complex issues, and otherwise prime viewers for continued learning.
[Editor's Note: To read other articles in this special magazine issue, visit the beautifully designed e-reader version.]
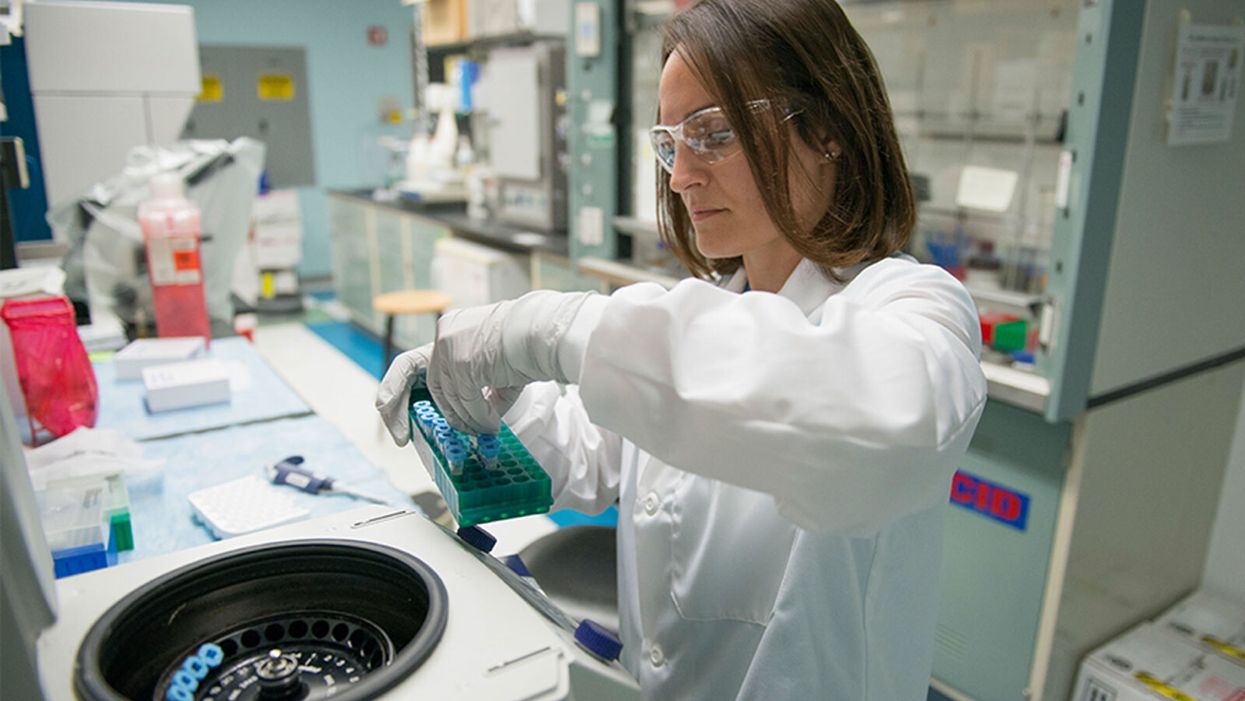
A researcher works in the lab at Alnylam Pharmaceuticals, which has pioneered the development of RNAi therapies.
In October 2006, Craig Mello received a strange phone call from Sweden at 4:30 a.m. The voice at the other end of the line told him to get dressed and that his life was about to change.
"We think this could be effective in [the early] phase, helping the body clear the virus and preventing progression to that severe hyperimmune response which occurs in some patients."
Shortly afterwards, he was informed that along with his colleague Andrew Fire, he had won the Nobel Prize in Physiology or Medicine.
Eight years earlier, biologists Fire and Mello had made a landmark discovery in the history of genetics. In a series of experiments conducted in worms, they had revealed an ancient evolutionary mechanism present in all animals that allows RNA – the structures within our cells that take genetic information from DNA and use it to make proteins – to selectively switch off genes.
At the time, scientists heralded the dawn of a new field of medical research utilizing this mechanism, known as RNA interference or RNAi, to tackle rare genetic diseases and deactivate viruses. Now, 14 years later, the pharmaceutical company Alnylam — which has pioneered the development of RNAi-based treatments over the past decade — is looking to use it to develop a groundbreaking drug for the virus that causes COVID-19.
"We can design small interfering RNAs to target regions of the viral genome and bind to them," said Akin Akinc, who manages several of Alnylam's drug development programs. "What we're learning about COVID-19 is that there's an early phase where there's lots of viral replication and a high viral load. We think this could be effective in that phase, helping the body clear the virus and preventing progression to that severe hyperimmune response which occurs in some patients."
Called ALN-COV, Alnylam's treatment hypothetically works by switching off a key gene in the virus, inhibiting its ability to replicate itself. In order to deliver it to the epithelial cells deep in the lung tissue, where the virus resides, patients will inhale a fine mist containing the RNAi molecules mixed in a saline solution, using a nebulizer.
But before human trials of the drug can begin, the company needs to convince regulators that it is both safe and effective in a series of preclinical trials. While early results appear promising - when mixed with the virus in a test tube, the drug displayed a 95 percent inhibition rate – experts are reserving judgment until it performs in clinical trials.
"If successful this could be a very important milestone in the development of RNAi therapies, but virus infections are very complicated and it can be hard to predict whether a given level of inhibition in cell culture will be sufficient to have a significant impact on the course of the infection," said Si-Ping Han, who researches RNAi therapeutics at California Institute of Technology and is not involved in the development of this drug.
So far, Alnylam has had success in using RNAi to treat rare genetic diseases. It currently has treatments licensed for Hereditary ATTR Amyloidosis and Acute Hepatic Porphyria. Another treatment, for Primary Hyperoxaluria Type 1, is currently under regulatory review. But its only previous attempt to use RNAi to tackle a respiratory infection was a failed effort to develop a drug for respiratory syncytial virus (RSV) almost a decade ago.
However, the technology has advanced considerably since then. "Back then, RNAi drugs had no chemical modifications whatsoever, so they were readily degraded by the body, and they could also result in unintended immune stimulation," said Akinc. "Since then, we've learned how to chemically modify our RNAi's to make them immunosilent and give them improved potency, stability, and duration of action."
"It would be a very important milestone in the development of RNAi therapies."
But one key challenge the company will face is the sheer speed at which viruses evolve, meaning they can become drug-resistant very quickly. Scientists predict that Alnylam will ultimately have to develop a series of RNAi drugs for the coronavirus that work together.
"There's been considerable interest in using RNAi to treat viral infections, as RNA therapies can be developed more rapidly than protein therapies like monoclonal antibodies, since one only needs to know the viral genome sequence to begin to design them," said David Schaffer, professor of bioengineering at University of California, Berkeley. "But viruses can evolve their sequences rapidly around single drugs so it is likely that a combinatorial RNAi therapy may be needed."
In the meantime, Alnylam is conducting further preclinical trials over the summer and fall, with the aim of launching testing in human volunteers by the end of this year -- an ambitious aim that would represent a breakneck pace for a drug development program.
If the approach does ultimately succeed, it would represent a major breakthrough for the field as a whole, potentially opening the door to a whole new wave of RNAi treatments for different lung infections and diseases.
"It would be a very important milestone in the development of RNAi therapies," said Han, the Caltech researcher. "It would be both the first time that an RNAi drug has been successfully used to treat a respiratory infection and as far as I know, the first time that one has been successful in treating any disease in the lungs. RNAi is a platform that can be reconfigured to hit different targets, and so once the first drug has been developed, we can expect a rapid flow of variants targeting other respiratory infections or other lung diseases."
The Biggest Challenge for a COVID-19 Vaccine
As scientists race to develop a safe and effective vaccine, companies and governments must figure out how to distribute affordable doses all over the world as fast as possible.
Although no one has conducted a survey on the topic, it's safe to say that a single hope unites much of humanity at the present moment: the prospect of a vaccine for COVID-19, which has infected more than 9 million people worldwide, killed nearly 500,000, and sent the global economy into a tailspin since it first appeared in China last December.
"We've never delivered something to every corner of the world before."
Scientists are racing to make that vision a reality. As of this writing, 11 vaccine candidates are in clinical trials and over 100 others are in preclinical development, in a dozen countries. Pointing to new technology and compressed testing protocols, experts predict a winner could emerge in 12 to 18 months—a fraction of the four years it took to develop the previous record-holder, the mumps vaccine, in the 1960s. Teams at Oxford University and Boston-based Moderna Therapeutics say they could have a product ready even sooner, if the formulas they're testing prove safe and effective. A just-announced White House initiative, Operation Warp Speed, aims to fast-track multiple candidates, with the goal of delivering 100 million doses in November and another 200 million by January 2021.
These timetables could prove wildly over-optimistic. But even if the best-case scenario comes true, and a viable COVID-19 vaccine emerges this fall, a gargantuan challenge remains: getting the shot to everyone who needs it. Epidemiologists figure that at least 70 percent of Earth's population—or 5.6 billion people—would have to be inoculated to achieve "herd immunity," in which each person who catches the disease passes it to less than one other individual. "In order to stop the pandemic, we need to make the vaccine available to almost every person on the planet," Microsoft co-founder Bill Gates blogged in April, as his foundation pledged $300 million to the effort. "We've never delivered something to every corner of the world before."
The difficulties are partly logistical, partly political, and largely a combination of the two. Overcoming those obstacles will require unprecedented cooperation among national governments, international organizations, and profit-minded corporations—in an era when nationalist rivalries are rampant and global leadership is up for grabs.
That may be tougher than developing the vaccine itself.
Logistical Conundrums
Manufacturing and distributing billions of vaccine doses would be a daunting task even in the most harmonious of times. Take the packaging problem. The vaccines under development range from old-school (based on inactivated or weakened viruses) to cutting-edge (using snippets of RNA or DNA to train the immune system to attack the invader). Some may work better than others for different patient groups—the young versus the elderly, for example. All, however, must be stored in vials and administered with syringes.
Among the handful of U.S. companies that manufacture such products, many must import the special glass tubing for vials, as well as the polypropylene for syringe barrels and the rubber or silicone for stoppers and plungers. These materials are commonly sourced from China and India, where lockdowns and export bans restrict supply. Rick Bright, the ousted director of the federal Biomedical Advanced Research and Development Authority (BARDA), claims he was ignored when he warned the Trump Administration that a medical-glass shortage was looming before the coronavirus crisis hit; securing enough to vaccinate 300 million Americans, he told Congress in May, could take up to two years.
Getting the vaccine to poorer countries presents further hurdles. To begin with, there's refrigeration. Inactivated or live vaccines must be kept between 2 and 8 degrees Centigrade (or 35 to 46 degrees Fahrenheit); RNA vaccines typically require much colder temperatures—as low as -80 degrees. This makes storage and transport challenging in parts of the world that lack reliable electricity. DNA vaccines don't need cold storage, but (like RNA vaccines) they remain experimental. They've never been approved to treat any human disease.
Tracking vaccine distribution is another conundrum for low- to-middle-income countries. "Supply chain management is really about information," explains Rebecca Weintraub, assistant professor of global health and social medicine at Harvard Medical School and director of the Better Evidence project at Harvard's Ariadne Labs. "It's about leveraging data to determine demand, predict behavior, and understand the flow of the product itself." Systems for collecting and analyzing such data can be hard to find in poorer regions, she notes. What's more, many people in those areas lack any type of ID card, making it difficult to know who has or hasn't received a vaccine.
Weintraub and two coauthors published an article in April in the Harvard Business Review, suggesting solutions to these and other developing-world problems: solar direct-drive refrigerators, app-based data-capture systems, biometric digital IDs. But such measures—not to mention purchasing adequate supplies of vaccine—would require massive funding.
And that's where the logistical begins to overlap with the political.
Global Access Versus "Vaccine Nationalism"
An array of institutions have already begun laying the groundwork for achieving worldwide, equitable access to COVID-19 vaccines. In February, the World Bank and the Norway-based Coalition for Epidemic Preparedness Innovations (CEPI) cohosted a global consultation on funding vaccine development and manufacturing. In late April, the World Health Organization (WHO), in collaboration with dozens of governments, nonprofits, and industry leaders, launched a program called the Access to COVID-19 Tools Accelerator to expedite such efforts.
Soon afterward, the European Union, along with six countries and the Bill and Melinda Gates Foundation, held a Coronavirus Global Response telethon that raised $8 billion to support Gavi, the Vaccine Alliance—a public-private partnership that subsidizes immunization in low-income countries. The United States and Russia, however, chose not to participate.
This snub by the world's remaining superpower and one of its principal challengers worried many observers. "I am concerned about what I call vaccine nationalism," CEPI executive director Richard Hatchett told the Los Angeles Times. "That's the tension between obligations elected leaders will feel to protect the lives of their citizens" versus the imperative for global sharing.
Some signs point to a possible rerun of the hoarding that accompanied the 2009 H1N1 influenza pandemic, when wealthy nations bought up virtually all vaccine supplies—denying them to poorer countries, and sometimes to one another. Operation Warp Speed has declared an "America First" policy for any vaccine arising from its efforts. Pharma giant Sanofi recently suggested that it would take a similar approach, since the U.S. was first to fund the company's COVID-19 research. (Sanofi's CEO backtracked after officials in France, where the firm is headquartered, protested.) The Oxford group, which is partnering with British-based drug maker AstraZeneca, intends to prioritize Great Britain.
Yet momentum is building for more generous strategies as well. In May, over 100 current and former world leaders, along with prominent economists and public health experts, issued an open letter calling for a "people's vaccine" for COVID-19, which would be patent-free, distributed globally, and available to all countries free of charge. At the WHO's annual World Health Assembly, all 194 member states accepted a resolution urging that vaccines for the disease be made available as a "global public good"—though the U.S. dissociated itself from a clause proposing a patent pool to keep costs down, which it argued might disincentivize "innovators who will be essential to the solutions the whole world needs."
Gavi, for its part, plans to launch a mechanism designed to encourage those innovators while promoting accessibility: an advance market commitment, in which countries pledge to purchase a vaccine, with no money down. Future contributions will be based on the value of the product to their health systems and their ability to pay.
"It's essential to realize that a threat anywhere is a threat everywhere."
A few private-sector players are stepping up, too. U.S.-based Johnson & Johnson, which has received nearly half a billion dollars from the federal government for COVID-19 vaccine research, has promised to provide up to 900 million doses on a not-for-profit basis, if its trials pan out. Other companies have agreed to produce vaccines on a "cost-plus" basis, with a smaller-than-usual profit margin.
How Sharing Can Pay Off
No one knows how all this will work out if and when a vaccine becomes available. (Another wild card: Trump has announced that he is cutting U.S. ties to the WHO over its alleged favoritism toward China, which could hobble the agency's ability to coordinate distribution -- though uncertainty remains about the process of withdrawal and reversing course may still be possible.) To public health experts, however, it's clear that ensuring accessibility is not just a matter of altruism.
"A historic example is smallpox," Rebecca Weintraub observes. "When it kept getting reintroduced into high-income countries from low-income countries, the rich countries realized it was worth investing in the vaccine for countries that couldn't afford it." After a two-decade campaign led by the WHO, the last case of this ancient scourge was diagnosed in 1977.
Conversely, vaccine nationalism doesn't just hurt poor countries. During the H1N1 pandemic, which killed an estimated 284,000 people worldwide, production problems led to shortages in the United States. But Australia stopped a domestic manufacturer from exporting doses to the U.S until all Aussies had been immunized.
Such considerations, Weintraub believes, might help convince even the most reluctant rich-country leaders that an accessible vaccine—if deployed in an epidemiologically targeted way—would serve both the greater good and the national interest. "I suspect the pressures put on our politicians to act globally will be significant," she says.
Other analysts share her guarded optimism. Kelly Moore, who teaches health policy at Vanderbilt University Medical Center, oversaw Tennessee's immunization programs for more than a decade, and later became a member of the Sabin-Aspen Vaccine Science & Policy Group—a panel of international experts that in 2019 released a report titled "Accelerating the Development of a Universal Influenza Vaccine." The 117-page document provided a road map toward a long-sought goal: creating a flu shot that doesn't need to be reformulated each year to target changing viral strains.
"One lesson we learned was that it's crucial to deploy financial resources in a systematic way to support coordination among laboratories that would typically be competitors," Moore says. And that, she adds, is happening with COVID-19, despite nationalist frictions: scientists from Sanofi joining forces with those at rival GSK; researchers at other companies allying with teams at government laboratories; university labs worldwide sharing data across borders. "I have been greatly encouraged to see the amount of global collaboration involved in this enterprise. Partners are working together who would normally never be partners."
For Moore, whose 77-year-old mother survived a bout with the disease, the current pandemic has hit close to home. "It's essential to realize that a threat anywhere is a threat everywhere," she says. "Morally and ethically, we have a tremendous obligation to ensure that the most vulnerable have access to an affordable vaccine, irrespective of where they live."
[Editor's Note: This article was originally published on June 8th, 2020 as part of a standalone magazine called GOOD10: The Pandemic Issue. Produced as a partnership among LeapsMag, The Aspen Institute, and GOOD, the magazine is available for free online. For this reprinting of the article, we have updated the latest statistics on COVID-19 and related global news.]
CORRECTION: A sentence about DNA vaccines incorrectly stated that they require cold storage, like RNA vaccines. The error has been fixed.