Top Fertility Doctor: Artificially Created Sperm and Eggs "Will Become Normal" One Day
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

A rendering of in vitro fertilization.
Imagine two men making a baby. Or two women. Or an infertile couple. Or an older woman whose eggs are no longer viable. None of these people could have a baby today without the help of an egg or sperm donor.
Cells scraped from the inside of your cheek could one day be manipulated to become either eggs or sperm.
But in the future, it may be possible for them to reproduce using only their own genetic material, thanks to an emerging technology called IVG, or in vitro gametogenesis.
Researchers are learning how to reprogram adult human cells like skin cells to become lab-created egg and sperm cells, which could then be joined to form an embryo. In other words, cells scraped from the inside of your cheek could one day be manipulated to become either eggs or sperm, no matter your gender or your reproductive fitness.
In 2016, Japanese scientists proved that the concept could be successfully carried out in mice. Now some experts, like Dr. John Zhang, the founder and CEO of New Hope Fertility Center in Manhattan, say it's just "a matter of time" before the method is also made to work in humans.
Such a technological tour de force would upend our most basic assumptions about human reproduction and biology. Combined with techniques like gene editing, these tools could eventually enable prospective parents to have an unprecedented level of choice and control over their children's origins. It's a wildly controversial notion, and an especially timely one now that a Chinese scientist has announced the birth of the first allegedly CRISPR-edited babies. (The claims remain unverified.)
Zhang himself is no stranger to controversy. In 2016, he stunned the world when he announced the birth of a baby conceived using the DNA of three people, a landmark procedure intended to prevent the baby from inheriting a devastating neurological disease. (Zhang went to a clinic in Mexico to carry out the procedure because it is prohibited in the U.S.) Zhang's other achievements to date include helping a 49-year-old woman have a baby using her own eggs and restoring a young woman's fertility through an ovarian tissue transplant surgery.
Zhang recently sat down with our Editor-in-Chief in his New York office overlooking Columbus Circle to discuss the fertility world's latest provocative developments. Here are his top ten insights:
Clearly [gene-editing embryos] will be beneficial to mankind, but it's a matter of how and when the work is done.
1) On a Chinese scientist's claim of creating the first CRISPR-edited babies:
I'm glad that we made a first move toward a clinical application of this technology for mankind. Somebody has to do this. Whether this was a good case or not, there is still time to find out.
Clearly it will be beneficial to mankind, but it's a matter of how and when the work is done. Like any scientific advance, it has to be done in a very responsible way.
Today's response is identical to when the world's first IVF baby was announced in 1978. The major news media didn't take it seriously and thought it was evil, wanted to keep a distance from IVF. Many countries even abandoned IVF, but today you see it is a normal practice. And it took almost 40 years [for the researchers] to win a Nobel Prize.
I think we need more time to understand how this work was done medically, ethically, and let the scientist have the opportunity to present how it was done and let a scientific journal publish the paper. Before these become available, I don't think we should start being upset, scared, or giving harsh criticism.
2) On the international outcry in response to the news:
I feel we are in scientific shock, with many thinking it came too fast, too soon. We all embrace modern technology, but when something really comes along, we fear it. In an old Chinese saying, one of the masters always dreamed of seeing the dragon, and when the dragon really came, he got scared.
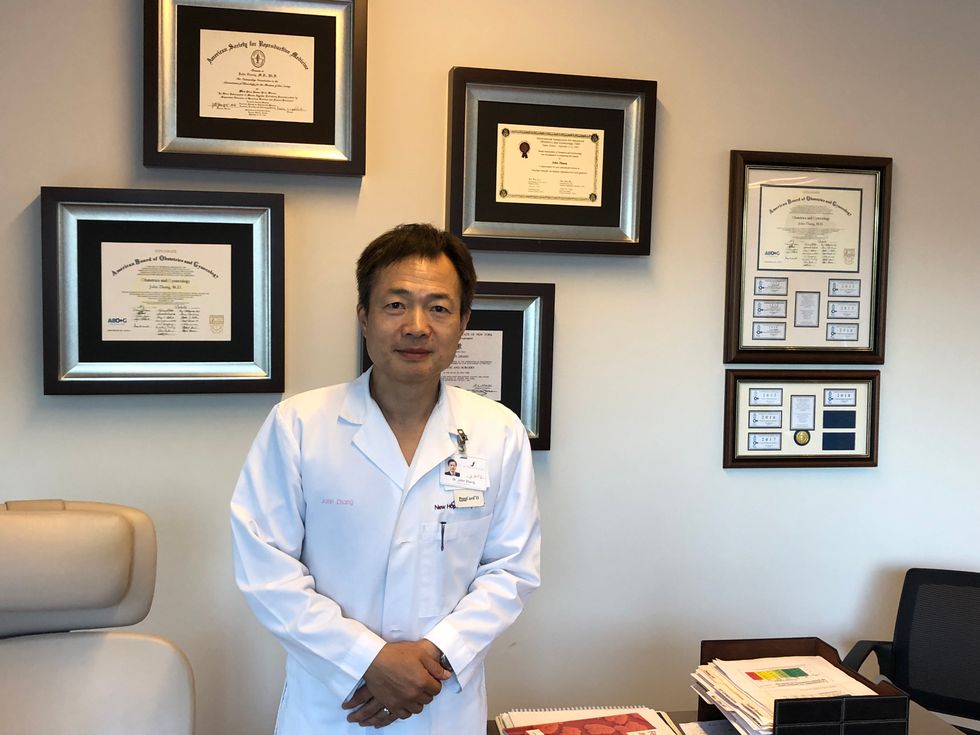
Dr. John Zhang, the founder and CEO of New Hope Fertility Center in Manhattan, pictured in his office.
3) On the Western world's perception that Chinese scientists sometimes appear to discount ethics in favor of speedy breakthroughs:
I think this perception is not fair. I don't think China is very casual. It's absolutely not what people think. I don't want people to feel that this case [of CRISPR-edited babies] will mean China has less standards over how human reproduction should be performed. Just because this happened, it doesn't mean in China you can do anything you want.
As far as the regulation of IVF clinics, China is probably the most strictly regulated of any country I know in this world.
4) On China's first public opinion poll gauging attitudes toward gene-edited babies, indicating that more than 60 percent of survey respondents supported using the technology to prevent inherited diseases, but not to enhance traits:
There is a sharp contrast between the general public and the professional world. Being a working health professional and an advocate of scientists working in this field, it is very important to be ethically responsible for what we are doing, but my own feeling is that from time to time we may not take into consideration what the patient needs.
5) On how the three-parent baby is doing today, several years after his birth:
No news is good news.
6) On the potentially game-changing research to develop artificial sperm and eggs:
First of all I think that anything that's technically possible, as long as you are not harmful to other people, to other societies, as long as you do it responsibly, and this is a legitimate desire, I think eventually it will become reality.
My research for now is really to try to overcome the very next obstacle in our field, which is how to let a lady age 44 or older have a baby with her own genetic material.
Practically 99 percent of women over age 43 will never make a baby on their own. And after age 47, we usually don't offer donor egg IVF anymore.
But with improved longevity, and quality of life, the lifespan of females continues to increase. In Japan, the average for females is about 89 years old. So for more than half of your life, you will not be able to produce a baby, which is quite significant in the animal kingdom. In most of the animal kingdom, their reproductive life is very much the same as their life, but then you can argue in the animal kingdom unlike a human being, it doesn't take such a long time for them to contribute to the society because once you know how to hunt and look for food, you're done.
"I think this will become a major ethical debate: whether we should let an older lady have a baby at a very late state of her life."
But humans are different. You need to go to college, get certain skills. It takes 20 years to really bring a human being up to become useful to society. That's why the mom and dad are not supposed to have the same reproductive life equal to their real life.
I think this will become a major ethical debate: whether we should let an older lady have a baby at a very late state of her life and leave the future generation in a very vulnerable situation in which they may lack warm caring, proper guidance, and proper education.
7) On using artificial gametes to grant more reproductive choices to gays and lesbians:
I think it is totally possible to have two sperm make a baby, and two eggs make babies.
If we have two guys, one guy to produce eggs, or two girls, one would have to become sperm. Basically you are creating artificial gametes or converting with gametes from sperm to become egg or egg to become a sperm. Which may not necessarily be very difficult. The key is to be able to do nuclear reprogramming.
So why can two sperm not make offspring now? You get exactly half of your genes from each parent. The genes have their own imprinting that say "made in mom," "made in dad." The two sperm would say "made in dad," "made in dad." If I can erase the "made in dad," and say "made in mom," then these sperm can make offspring.
8) On how close science is to creating artificial gametes for clinical use in pregnancies:
It's very hard to say until we accomplish it. It could be very quick. It could be it takes a long time. I don't want to speculate.
"I think these technologies are the solid foundation just like when we designed the computer -- we never thought a computer would become the iPhone."
9) On whether there should be ethical red lines drawn by authorities or whether the decisions should be left to patients and scientists:
I think we cannot believe a hundred percent in the scientist and the patient but it should not be 100 percent authority. It should be coming from the whole of society.
10) On his expectations for the future:
We are living in a very exciting world. I think that all these technologies can really change the way of mankind and also are not just for baby-making. The research, the experience, the mechanism we learn from these technologies, they will shine some great lights into our long-held dream of being a healthy population that is cancer-free and lives a long life, let's say 120 years.
I think these technologies are the solid foundation just like when we designed the computer -- we never thought a computer would become the iPhone. Imagine making a computer 30 years ago, that this little chip will change your life.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
In this week's Friday Five, new research that could help prevent Alzheimer's. Plus, why you should care about smart senior towns, how to reverse being drunk, money can make you happier if you're this type of person, and personalized anxiety medicine.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Here are the promising studies covered in this week's Friday Five, featuring interviews with Dr. Christopher Martens, director of the Delaware Center for Cogntiive Aging Research and professor of kinesiology and applied physiology at the University of Delaware, and Dr. Ilona Matysiak, visiting scholar at Iowa State University and associate professor of sociology at Maria Grzegorzewska University.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
- Could this supplement help prevent Alzheimer's?
- Why you should care about smart senior towns
- Here's how to reverse being drunk
- Money can make you happy - if you're this type of person
- Personalized anxiety medicine
As gene therapies and small molecule drugs are being studied in clinical trials, companies increasingly see the value in hiring patients to help explain the potential benefits.
As a child, Wendy Borsari participated in a health study at Boston Children’s Hospital. She was involved because heart disease and sudden cardiac arrest ran in her family as far back as seven generations. When she was 18, however, the study’s doctors told her that she had a perfectly healthy heart and didn’t have to worry.
A couple of years after graduating from college, though, the Boston native began to experience episodes of near fainting. During any sort of strenuous exercise, my blood pressure would drop instead of increasing, she recalls.
She was diagnosed at 24 with hypertrophic cardiomyopathy. Although HCM is a commonly inherited heart disease, Borsari’s case resulted from a rare gene mutation, the MYH7 gene. Her mother had been diagnosed at 27, and Borsari had already lost her grandmother and two maternal uncles to the condition. After her own diagnosis, Borsari spent most of her free time researching the disease and “figuring out how to have this condition and still be the person I wanted to be,” she says.
Then, her son was found to have the genetic mutation at birth and diagnosed with HCM at 15. Her daughter, also diagnosed at birth, later suffered five cardiac arrests.
That changed Borsari’s perspective. She decided to become a patient advocate. “I didn’t want to just be a patient with the condition,” she says. “I wanted to be more involved with the science and the biopharmaceutical industry so I could be active in helping to make it better for other patients.”
She consulted on patient advocacy for a pharmaceutical and two foundations before coming to a company called Tenaya in 2021.
“One of our core values as a company is putting patients first,” says Tenaya's CEO, Faraz Ali. “We thought of no better way to put our money where our mouth is than by bringing in somebody who is affected and whose family is affected by a genetic form of cardiomyopathy to have them make sure we’re incorporating the voice of the patient.”
Biomedical corporations and government research agencies are now incorporating patient advocacy more than ever, says Alice Lara, president and CEO of the Sudden Arrhythmia Death Syndromes Foundation in Salt Lake City, Utah. These organizations have seen the effectiveness of including patient voices to communicate and exemplify the benefits that key academic research institutions have shown in their medical studies.
“From our side of the aisle,” Lara says, “what we know as patient advocacy organizations is that educated patients do a lot better. They have a better course in their therapy and their condition, and understanding the genetics is important because all of our conditions are genetic.”
Founded in 2016, Tenaya is advancing gene therapies and small molecule drugs in clinical trials for both prevalent and rare forms of heart disease, says Ali, the CEO.
The firm's first small molecule, now in a Phase 1 clinical trial, is intended to treat heart failure with preserved ejection fraction, where the amount of blood pumped by the heart is reduced due to the heart chambers becoming weak or stiff. The condition accounts for half or more of all heart failure in the U.S., according to Ali, and is growing quickly because it's closely associated with diabetes. It’s also linked with metabolic syndrome, or a cluster of conditions including high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels.
“We have a novel molecule that is first in class and, to our knowledge, best in class to tackle that, so we’re very excited about the clinical trial,” Ali says.
The first phase of the trial is being performed with healthy participants, rather than people with the disease, to establish safety and tolerability. The researchers can also look for the drug in blood samples, which could tell them whether it's reaching its target. Ali estimates that, if the company can establish safety and that it engages the right parts of the body, it will likely begin dosing patients with the disease in 2024.
Tenaya’s therapy delivers a healthy copy of the gene so that it makes a copy of the protein missing from the patients' hearts because of their mutation. The study will start with adult patients, then pivot potentially to children and even newborns, Ali says, “where there is an even greater unmet need because the disease progresses so fast that they have no options.”
Although this work still has a long way to go, Ali is excited about the potential because the gene therapy achieved positive results in the preclinical mouse trial. This animal trial demonstrated that the treatment reduced enlarged hearts, reversed electrophysiological abnormalities, and improved the functioning of the heart by increasing the ejection fraction after the single-dose of gene therapy. That measurement remained stable to the end of the animals’ lives, roughly 18 months, Ali says.
He’s also energized by the fact that heart disease has “taken a page out of the oncology playbook” by leveraging genetic research to develop more precise and targeted drugs and gene therapies.
“Now we are talking about a potential cure of a disease for which there was no cure and using a very novel concept,” says Melind Desai of the Cleveland Clinic.
Tenaya’s second program focuses on developing a gene therapy to mitigate the leading cause of hypertrophic cardiomyopathy through a specific gene called MYPBC3. The disease affects approximately 600,000 patients in the U.S. This particular genetic form, Ali explains, affects about 115,000 in the U.S. alone, so it is considered a rare disease.
“There are infants who are dying within the first weeks to months of life as a result of this mutation,” he says. “There are also adults who start having symptoms in their 20s, 30s and 40s with early morbidity and mortality.” Tenaya plans to apply before the end of this year to get the FDA’s approval to administer an investigational drug for this disease humans. If approved, the company will begin to dose patients in 2023.
“We now understand the genetics of the heart much better,” he says. “We now understand the leading genetic causes of hypertrophic myopathy, dilated cardiomyopathy and others, so that gives us the ability to take these large populations and stratify them rationally into subpopulations.”
Melind Desai, MD, who directs Cleveland Clinic’s Hypertrophic Cardiomyopathy Center, says that the goal of Tenaya’s second clinical study is to help improve the basic cardiac structure in patients with hypertrophic cardiomyopathy related to the MYPBC3 mutation.
“Now we are talking about a potential cure of a disease for which there was no cure and using a very novel concept,” he says. “So this is an exciting new frontier of therapeutic investigation for MYPBC3 gene-positive patients with a chance for a cure.
Neither of Tenaya’s two therapies address the gene mutation that has affected Borsari and her family. But Ali sees opportunity down the road to develop a gene therapy for her particular gene mutation, since it is the second leading cause of cardiomyopathy. Treating the MYH7 gene is especially challenging because it requires gene editing or silencing, instead of just replacing the gene.
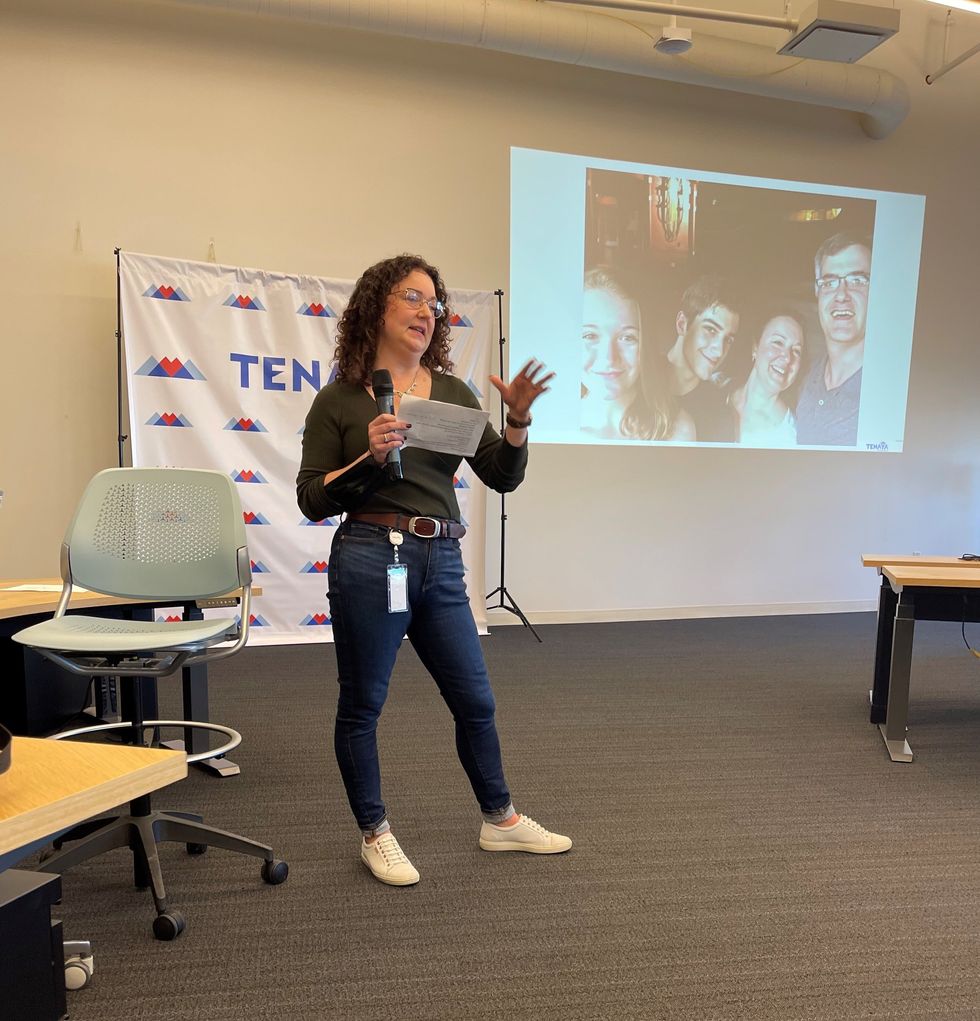
Wendy Borsari was diagnosed at age 24 with a commonly inherited heart disease. She joined Tenaya as a patient advocate in 2021.
Wendy Borsari
“If you add a healthy gene it will produce healthy copies,” Ali explains, “but it won’t stop the bad effects of the mutant protein the gene produces. You can only do that by silencing the gene or editing it out, which is a different, more complicated approach.”
Euan Ashley, professor of medicine and genetics at Stanford University and founding director of its Center for Inherited Cardiovascular Disease, is confident that we will see genetic therapies for heart disease within the next decade.
“We are at this really exciting moment in time where we have diseases that have been under-recognized and undervalued now being attacked by multiple companies with really modern tools,” says Ashley, author of The Genome Odyssey. “Gene therapies are unusual in the sense that they can reverse the cause of the disease, so we have the enticing possibility of actually reversing or maybe even curing these diseases.”
Although no one is doing extensive research into a gene therapy for her particular mutation yet, Borsari remains hopeful, knowing that companies such as Tenaya are moving in that direction.
“I know that’s now on the horizon,” she says. “It’s not just some pipe dream, but will happen hopefully in my lifetime or my kids’ lifetime to help them.”

