New drug for schizophrenia could meet desperate need for better treatments

The field of treating schizophrenia with drugs has been stuck in a long drought but, this month, a late-stage clinical trial found a new drug called KarXT could treat a range of symptoms.
Schizophrenia is a debilitating mental health condition that affects around 24 million people worldwide. Patients experience hallucinations and delusions when they develop schizophrenia, with experts referring to these new thoughts and behaviors as positive symptoms. They also suffer from negative symptoms in which they lose important functions, suffering from dulled emotions, lack of purpose and social withdrawal.
Currently available drugs can control only a portion of these symptoms but, on August 8th, Karuna Therapeutics announced its completion of a phase 3 clinical trial that found a new drug called KarXT could treat both positive and negative symptoms of schizophrenia. It could mean substantial progress against a problem that has stymied scientists for decades.
A long-standing problem
Since the 1950s, antipsychotics have been used to treat schizophrenia. People who suffer from it are thought to have too much of a brain chemical called dopamine, and antipsychotics work by blocking dopamine receptors in the brain. They can be effective in treating positive symptoms but have little impact on the negative ones, which can be devastating for a patient’s quality of life, making it difficult to maintain employment and have successful relationships. About 30 percent of schizophrenia patients don't actually respond to antipsychotics at all. Current drugs can also have adverse side effects including elevated cholesterol, high blood pressure, diabetes and movements that patients cannot control.
The recent clinical trial heralds a new treatment approach. “We believe it marks an important advancement for patients given its new and completely different mechanism of action from current therapies,” says Andrew Miller, COO of Karuna.
Scientists have been looking to develop alternatives. However, “the field of drug treatment of schizophrenia is currently in the doldrums,” says Peter McKenna, a senior researcher at FIDMAG Research Foundation in Spain which specialises in mental health.
In the 2000s there was a major push to target a brain receptor for a chemical called glutamate. Evidence suggested that this receptor is abnormal in the brains of schizophrenia patients, but attempts to try glutamate failed in clinical trials.
After that, many pharmaceutical companies dropped out of the race for a more useful treatment. But some companies continued to search, such as Karuna Therapeutics, led by founder and Chief Operating Officer Andrew Miller and CEO Steve Paul. The recent clinical trial suggests their persistence has led to an important breakthrough with their drug, KarXT. “We believe it marks an important advancement for patients given its new and completely different mechanism of action from current therapies,” Miller says.
How it works
Neurotransmitters are chemical messengers that pass signals between neurons. To work effectively, neurotransmitters need a receptor to bind to. A neurotransmitter called acetylcholine seems to be especially important in schizophrenia. It interacts with sites called muscarinic receptors, which are involved in the network of nerves that calm your body after a stressful event. Post mortem studies in people with schizophrenia have shown that two muscarinic receptors in the brain, the M1 and M4 receptors, are activated at unusually low levels because they don’t receive enough signals from acetylcholine.
The M4 receptor appears to play a role in psychosis. The M1 receptor is also associated with psychosis but is primarily thought to be involved in cognition. KarXT, taken orally, works by activating both of these receptors to signal properly. It is this twofold action that seems to explain its effectiveness. “[The drug’s] design enables the preferential stimulation of these muscarinic receptors in the brain,” Miller says.
How it developed
It all started in the early 1990s when Paul was at pharmaceutical company Eli Lilly. He discovered that Xanomeline, the drug they were testing on Alzheimer's patients, had antipsychotic effects. It worked by stimulating M1 and M4 receptors, so he and his colleagues decided to test Xanomeline on schizophrenia patients, supported by research on the connection between muscarinic receptors and psychosis. They found that Xanomeline reduced both positive and negative symptoms.
Unfortunately, it also caused significant side effects. The problem was that stimulating the M1 and M4 receptors in the brain also stimulated muscarinic receptors in the body that led to severe vomiting, diarrhea and even the temporary loss of consciousness.
In the end, Eli Lilly discontinued the clinical trials for the drug, but Miller set up Karuna Therapeutics to develop a solution. “I was determined to find a way to harness the therapeutic benefit demonstrated in studies of Xanomeline, while eliminating side effects that limited its development,” Miller says.
He analysed over 7,000 possible ways of mixing Xanomeline with other agents before settling on KarXT. It combines Xanomeline with a drug called Trospium Chloride, which blocks muscarinic receptors in the body – taking care of the side effects such as vomiting – but leaves them unblocked in the brain. Paul was so excited by Miller’s progress that he joined Karuna after leaving Eli Lilly and founding two previous startups.
“It's a very important approach,” says Rick Adams, Future Leaders Fellow in the Institute of Cognitive Neuroscience and Centre for Medical Image Computing at University College London. “We are in desperate need of alternative drug targets and this target is one of the best. There are other alternative targets, but not many are as close to being successful as the muscarinic receptor drug.”
Clinical Trial
Following a successful phase 2 clinical trial in 2019, the most recent trial involved 126 patients who were given KarXT, and 126 who were given a placebo. Compared to the placebo, patients taking KarXT had a significant 9.6 point reduction in the positive and negative syndrome scale (PANSS), the standard for rating schizophrenic symptoms.
KarXT also led to statistically significant declines in positive and negative symptoms compared to the placebo. “The results suggest that KarXT could be a potentially game-changing option in the management of both positive and negative symptoms of schizophrenia,” Miller says.
Robert McCutcheon, a psychiatrist and neuroscientist at Oxford University, is optimistic about the side effects but highlights the need for more safety trials.
McKenna, the researcher at FIDMAG Foundation, agrees about the drug’s potential. “The new [phase 3] study is positive,” he says. “It is reassuring that one is not dealing with a drug that works in one trial and then inexplicably fails in the next one.”
Robert McCutcheon, a psychiatrist and neuroscientist at Oxford University, said the drug is an unprecedented step forward. “KarXT is one of the first drugs with a novel mechanism of action to show promise in clinical trials.”
Even though the drug blocks muscarine receptors in the body, some patients still suffered from adverse side effects like vomiting, dizziness and diarrhea. But in general, these effects were mild to moderate, especially compared to dopamine-blocking antipsychotics or Xanomeline on its own.
McCutcheon is optimistic about the side effects but highlights the need for more safety trials. “The trial results suggest that gastrointestinal side effects appear to be manageable,” he says. “We know, however, from previous antipsychotic drugs that the full picture regarding the extent of side effects can sometimes take longer to become apparent to clinicians and patients. Careful ongoing assessment during a longer period of treatment will therefore be important.”
The Future
The team is currently conducting three other trials to evaluate the efficacy and long-term safety of KarXT. Their goal is to receive FDA approval next year.
Karuna is also conducting trials to evaluate the effectiveness of KarXT in treating psychosis in patients suffering from Alzheimer’s.
The big hope is that they will soon be able to provide a radically different drug to help many patients with schizophrenia. “We are another step closer to potentially providing the first new class of medicine in more than 50 years to the millions of people worldwide living with schizophrenia,” says Miller.
Current research pipelines in biotech could take over a decade unless the heightened attention garners more resources, experts say.
Since March, 35 patients in the care of Dr. Gregory Jicha, a neurologist at the University of Kentucky, have died of Alzheimer's disease or related dementia.
Meanwhile, with 233 active clinical trials underway to find treatments, Jicha wonders why mainstream media outlets don't do more to highlight potential solutions to the physical, emotional and economic devastation of these diseases. "Unfortunately, it's not until we're right at the cusp of a major discovery that anybody pays attention to these very promising agents," he says.
Heightened awareness would bring more resources for faster progress, according to Jicha. Otherwise, he's concerned that current research pipelines will take over a decade.
In recent years, newspapers with national readerships have devoted more technology reporting to key developments in social media, artificial intelligence, wired gadgets and telecom. Less prominent has been news about biotech—innovations based on biology research—and new medicines emerging from this technology. That's the impression of Jicha as well as Craig Lipset, former head of clinical innovation at Pfizer. "Scientists and clinicians are entirely invested [in biotech], yet no one talks about their discoveries," he says.
With the popular press rightly focusing on progress with a vaccine for COVID-19 this year, notable developments in biomarkers, Alzheimer's and cancer research, gene therapies for cystic fibrosis, and therapeutics related to biological age may be going unreported. Jennifer Goldsack, Executive Director of the nonprofit Digital Medicine Society, is confused over the media's soft touch with biotech. "I'm genuinely interested in understanding what editors of technology sections think the public wants to be reading."
The Numbers on Media Coverage
A newspaper's health section is a sensible fit for biotech reporting. In 2020, these departments have concentrated largely on COVID-19—as they should—while sections on technology and science don't necessarily pick up on other biotech news. Emily Mullin, staff writer for the tech magazine OneZero, has observed a gap in newspaper coverage. "You have a lot of [niche outlets] reporting biotech on the business side for industry experts, and you have a lot of reporting heavily from the science side focused on [readers who are] scientists. But there aren't a lot of outlets doing more humanizing coverage of biotech."
Indeed, the volume of coverage by top-tier media outlets in the U.S. for non-COVID biotech has dropped 32 percent since the pandemic spiked in March, according to an analysis run for this article by Commetric, a company that looks at media reputation for clients in many sectors including biotech and artificial intelligence. Meanwhile, the volume of coverage for AI has held steady, up one percent.
Commetric's CEO, Magnus Hakansson, thinks important biotech stories were omitted from mainstream coverage even before the world fell into the grips of the virus. "Apart from COVID, it's been extremely difficult for biotech companies to push out their discoveries," he says. "People in biotech have to be quite creative when they want to communicate [progress in] different therapeutic areas, and that is a problem."
In mid-February, just before the pandemic dominated the news cycle, researchers used machine learning to find a powerful new antibiotic capable of killing strains of disease-causing bacteria that had previously resisted all known antibiotics. Science-focused outlets hailed the work as a breakthrough, but some nationally-read newspapers didn't mention it. "There is this very silent crisis around antibiotic resistance that no one is aware of," says Goldsack. "We could be 50 years away from not being able to give elective surgeries because we are at such a high risk of being unable to control infection."
Could mainstream media strike a better balance between cynicism toward biotech and hyping animal studies that probably won't ever benefit the humans reading about them?
What's to Gain from More Mainstream Biotech
A brighter public spotlight on biotech could result in greater support and faster progress with research, says Lipset. "One of the biggest delays in drug development is patient recruitment. Patients don't know about the opportunities," he said, because, "clinical research pipelines aren't talked about in the mainstream news." Only about eight percent of oncology patients participate.
The current focus on COVID-19, while warranted, could also be excluding lines of research that seem separate from the virus, but are actually relevant. In September, Nir Barzilai, director of the Institute of Aging Research at Albert Einstein College of Medicine, told me about eight different observational studies finding decreased COVID-19 severity among people taking a drug called metformin, which is believed to slow down the major hallmarks of biological aging, such as inflammation. Once a vaccine is approved and distributed, biologically older people could supplement it with metformin.
"Shining the spotlight on this research now could really be critical because COVID has shown what happens in older adults and how they're more at risk," says Jenna Bartley, a researcher of aging and immunology at the University of Connecticut, but she believes mainstream media sometimes miss stories on anti-aging therapies or portray them inaccurately.
The question remains why.
The Theranos Effect and Other Image Problems
Before the pandemic, Mullin, the biotech writer at OneZero, looked into a story for her editor about a company with a new test for infectious diseases. The company said its test, based on technology for editing genes, was fast, easy to use, and could be tailored to any pathogen. Mullin told her editor the evidence for the test's validity was impressive.
He wondered if readers would agree. "This is starting to sound like Theranos," he said.
The brainchild of entrepreneur Elizabeth Holmes, Theranos was valued at $9 billion in 2014. Time Magazine named Holmes one of its most influential people, and the blood-testing company was heavily covered by the media as a game changer for health outcomes—until Holmes was exposed by the Wall Street Journal as a fraud and criminally charged.
In the OneZero article, Mullin and her editor were careful to explain the gene-editing tech was legit, explicitly distinguishing it from Theranos. "I was like, yes—but this actually works! And they can show it works."
While the Holmes scandal explains some of the mistrust, it's part of a bigger pattern. The public's hopes for biotech have been frustrated repeatedly in recent decades, fostering a media mantra of fool me twice, shame on me. A recent report by Commetric noted that after the bursting of the biotech market bubble in the early 2000s, commentators grew deeply skeptical of the field. An additional source of caution may be the number of researchers in biotech with conflicts of interest such as patents or their own startups. "It's a landmine," Mullin said. "We're conditioned to think that scientists are out for the common good, but they have their own biases."
Yet another source of uncertainty: the long regulatory road and cost for new therapies to be approved by the FDA. The process can take 15 years and over a billion dollars; the percentage of drugs actually crossing the final strand of red tape is notoriously low.
"The only time stories have reached the news is when there's a sensational headline about the cure for cancer," said Lipset, "when, in fact it's about mice, and then things drop off." Meanwhile, consumer protection hurdles for some technologies, such as computer chips, are less onerous than the FDA gauntlet for new medicines. The media may view research breakthroughs in digital tech as more impactful because they're likelier to find their way into commercially available products.
And whereas a handful of digital innovations have been democratized for widespread consumption—96 percent of Americans now own a cell phone, and 72 percent use social media—journalists at nationally-read newspapers may see biotech as less attainable for the average reader. Sure, we're all aging, but will the healthcare system grant everyone fair access to treatments for slowing the aging process? Current disparities in healthcare sow reason for doubt.
And yet. Recall Lipset's point that more press coverage would drive greater participation in clinical trials, which could accelerate them and diversify participants. Could mainstream media strike a better balance between cynicism toward biotech and hyping animal studies that probably won't ever benefit the humans reading about them?
Biotech in a Post-COVID World
Imagine it's early 2022. Hopefully, much of the population is protected from the virus through some combination of vaccines, therapeutics, and herd immunity. We're starting to bounce back from the social and economic shocks of 2020. COVID-19 headlines recede from the front pages, then disappear altogether. Gradually, certain aspects of life pick up where they left off in 2019, while a few changes forced by the pandemic prove to be more lasting, some for the better.
Among its possible legacies, the virus could usher in a new era of biotech development and press coverage, with these two trends reinforcing each other. While government has mismanaged its response to the virus, the level of innovation, collaboration and investment in pandemic-related biotech has been compared to the Manhattan Project. "There's no question that vaccine acceleration is a success story," said Kevin Schulman, a professor of medicine and economics at Stanford. "We could use this experience to build new economic models to correct market failures. It could carry over to oncology or Alzheimer's."
As Winston Churchill said, never let a good crisis go to waste.
Lipset thinks the virus has primed us to pay attention, bringing biotech into the public's consciousness like never before. He's amazed at how many neighbors and old friends from high school are coming out of the woodwork to ask him how clinical trials work. "What happens next is interesting. Does this open a window of opportunity to get more content out? People's appetites have been whetted."
High-profile wins could help to sustain interest, such as deployment of rapid tests of COVID-19 to be taken at home, a version of which the FDA authorized on November 18th. The idea bears resemblance to the Theranos concept, also designed as a portable analysis, except this test met the FDA's requirements and has a legitimate chance of changing people's lives. Meanwhile, at least two vaccines are on track to gain government approval in record time. The unprecedented speed could be a catalyst for streamlining inefficiencies in the FDA's approval process in non-emergency situations.
Tests for COVID-19 represent what some view as the future of managing diseases: early detection. This paradigm may be more feasible—and deserving of journalistic ink—than research on diseases in advanced stages, says Azra Raza, professor of medicine at Columbia University. "Journalists have to challenge this conceit of thinking we can cure end-stage cancer," says Raza, author of The First Cell. Beyond animal studies and "exercise helps" articles, she thinks writers should focus on biotech for catching the earliest footprints of cancer when it's more treatable. "Not enough people appreciate the extent of this tragedy, but journalists can help us do it. COVID-19 is a great moment of truth telling."
Another pressing truth is the need for vaccination, as half of Americans have said they'll skip them due to concerns about safety and effectiveness. It's not the kind of stumbling block faced by iPhones or social media algorithms. AI stirs plenty of its own controversy, but the public's interest in learning about AI and engaging with it seems to grow regardless. "Who are the publicists doing such a good job for AI that biotechnology is lacking?" Lipset wonders.
The job description of those publicists, whoever they are, could be expanding. Scientists are increasingly using AI to measure the effects of new medicines that target diseases—including COVID-19—and the pathways of aging. Mullin noted the challenge of reporting breakthroughs in the life sciences in ways the public understands. With many newsrooms tightening budgets, fewer writers have science backgrounds, and "biotech is daunting for journalists," she says. "It's daunting for me and I work in this area." Now factor in the additional expertise required to understand biotech and AI. "I learned the ropes for how to read a biotech paper, but I have no idea how to read an AI paper."
Nevertheless, Mullin believes reporters have a duty to scrutinize whether this convergence of AI and biotech will foster better outcomes. "Is it just the shiny new tool we're employing because we can? Will algorithms help eliminate health disparities or contribute to them even more? We need to pay attention."
Blood Money: Paying for Convalescent Plasma to Treat COVID-19
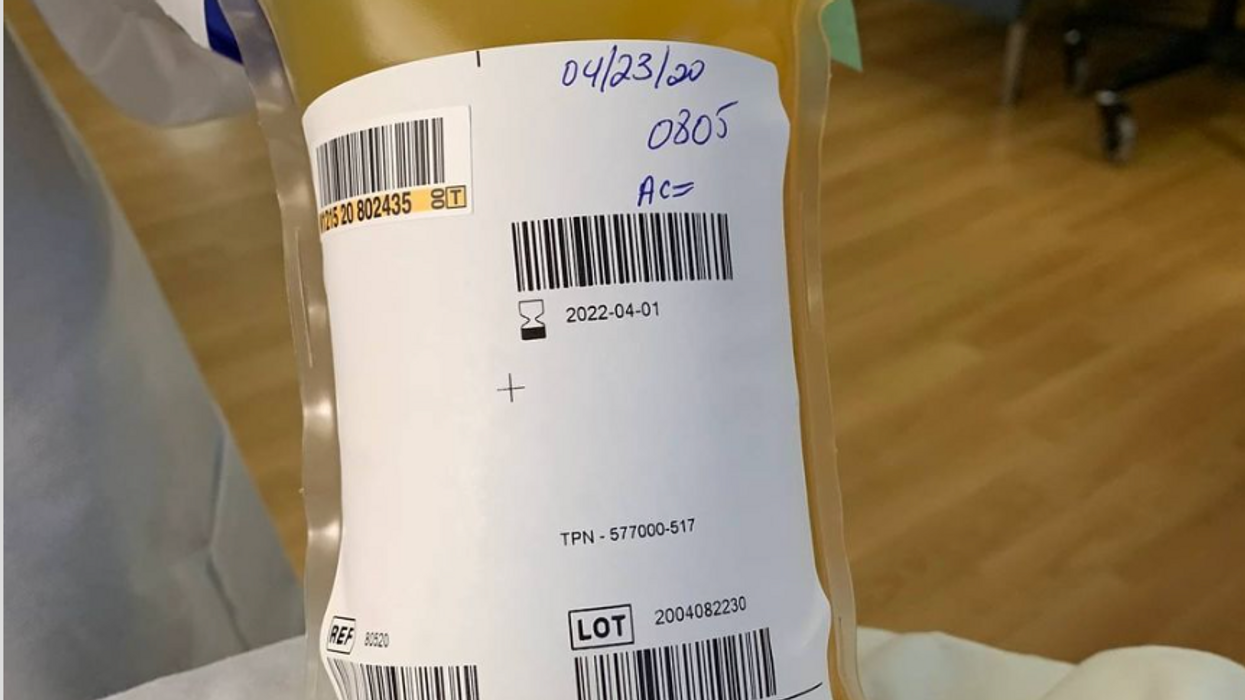
A bag of plasma that Tom Hanks donated back in April 2020 after his coronavirus infection. (He was not paid to donate.)
Convalescent plasma – first used to treat diphtheria in 1890 – has been dusted off the shelf to treat COVID-19. Does it work? Should we rely strictly on the altruism of donors or should people be paid for it?
The biologic theory is that a person who has recovered from a disease has chemicals in their blood, most likely antibodies, that contributed to their recovery, and transferring those to a person who is sick might aid their recovery. Whole blood won't work because there are too few antibodies in a single unit of blood and the body can hold only so much of it.
Plasma comprises about 55 percent of whole blood and is what's left once you take out the red blood cells that carry oxygen and the white blood cells of the immune system. Most of it is water but the rest is a complex mix of fats, salts, signaling molecules and proteins produced by the immune system, including antibodies.
A process called apheresis circulates the donors' blood through a machine that separates out the desired parts of blood and returns the rest to the donor. It takes several times the length of a regular whole blood donation to cycle through enough blood for the process. The end product is a yellowish concentration called convalescent plasma.
Recent History
It was used extensively during the great influenza epidemic off 1918 but fell out of favor with the development of antibiotics. Still, whenever a new disease emerges – SARS, MERS, Ebola, even antibiotic-resistant bacteria – doctors turn to convalescent plasma, often as a stopgap until more effective antibiotic and antiviral drugs are developed. The process is certainly safe when standard procedures for handling blood products are followed, and historically it does seem to be beneficial in at least some patients if administered early enough in the disease.
With few good treatment options for COVID-19, doctors have given convalescent plasma to more than a hundred thousand Americans and tens of thousand of people elsewhere, to mixed results. Placebo-controlled trials could give a clearer picture of plasma's value but it is difficult to enroll patients facing possible death when the flip of a coin will determine who will receive a saline solution or plasma.
And the plasma itself isn't some uniform pill stamped out in a factory, it's a natural product that is shaped by the immune history of the donor's body and its encounter not just with SARS-CoV-2 but a lifetime of exposure to different pathogens.
Researchers believe antibodies in plasma are a key factor in directly fighting the virus. But the variety and quantity of antibodies vary from donor to donor, and even over time from the same donor because once the immune system has cleared the virus from the body, it stops putting out antibodies to fight the virus. Often the quality and quantity of antibodies being given to a patient are not measured, making it somewhat hit or miss, which is why several companies have recently developed monoclonal antibodies, a single type of antibody found in blood that is effective against SARS-CoV-2 and that is multiplied in the lab for use as therapy.
Plasma may also contain other unknown factors that contribute to fighting disease, say perhaps signaling molecules that affect gene expression, which might affect the movement of immune cells, their production of antiviral molecules, or the regulation of inflammation. The complexity and lack of standardization makes it difficult to evaluate what might be working or not with a convalescent plasma treatment. Thus researchers are left with few clues about how to make it more effective.
Industrializing Plasma
Many Americans living along the border with Mexico regularly head south to purchase prescription drugs at a significant discount. Less known is the medical traffic the other way, Mexicans who regularly head north to be paid for plasma donations, which are prohibited in their country; the U.S. allows payment for plasma donations but not whole blood. A typical payment is about $35 for a donation but the sudden demand for convalescent plasma from people who have recovered from COVID-19 commands a premium price, sometimes as high as $200. These donors are part of a fast-growing plasma industry that surpassed $25 billion in 2018. The U.S. supplies about three-quarters of the world's needs for plasma.
Payment for whole blood donation in the U.S. is prohibited, and while payment for plasma is allowed, there is a stigma attached to payment and much plasma is donated for free.
The pharmaceutical industry has shied away from natural products they cannot patent but they have identified simpler components from plasma, such as clotting factors and immunoglobulins, that have been turned into useful drugs from this raw material of plasma. While some companies have retooled to provide convalescent plasma to treat COVID-19, often paying those donors who have recovered a premium of several times the normal rate, most convalescent plasma has come as donations through traditional blood centers.
In April the Mayo Clinic, in cooperation with the FDA, created an expanded access program for convalescent plasma to treat COVID-19. It was meant to reduce the paperwork associated with gaining access to a treatment not yet approved by the FDA for that disease. Initially it was supposed to be for 5000 units but it quickly grew to more than twenty times that size. Michael Joyner, the head of the program, discussed that experience in an extended interview in September.
The Centers for Medicare and Medicaid Services (CMS) also created associated reimbursement codes, which became permanent in August.
Mayo published an analysis of the first 35,000 patients as a preprint in August. It concluded, "The relationships between mortality and both time to plasma transfusion, and antibody levels provide a signature that is consistent with efficacy for the use of convalescent plasma in the treatment of hospitalized COVID-19 patients."
It seemed to work best when given early in infection and in larger doses; a similar pattern has been seen in studies of monoclonal antibodies. A revised version will soon be published in a major medical journal. Some criticized the findings as not being from a randomized clinical trial.
Convalescent plasma is not the only intervention that seems to work better when used earlier in the course of disease. Recently the pharmaceutical company Eli Lilly stopped a clinical trial of a monoclonal antibody in hospitalized COVID-19 patients when it became apparent it wasn't helping. It is continuing trials for patients who are less sick and begin treatment earlier, as well as in persons who have been exposed to the virus but not yet diagnosed as infected, to see if it might prevent infection. In November the FDA eased access to this drug outside of clinical trials, though it is not yet approved for sale.
Show Me the Money
The antibodies that seem to give plasma its curative powers are fragile proteins that the body produces to fight the virus. Production shuts down once the virus is cleared and the remaining antibodies survive only for a few weeks before the levels fade. [Vaccines are used to train immune cells to produce antibodies and other defenses to respond to exposure to future pathogens.] So they can be usefully harvested from a recovered patient for only a few short weeks or months before they decline precipitously. The question becomes, how does one mobilize this resource in that short window of opportunity?
The program run by the Mayo Clinic explains the process and criteria for donating convalescent plasma for COVID-19, as well as links to local blood centers equipped to handle those free donations. Commercial plasma centers also are advertising and paying for donations.
A majority of countries prohibit paying donors for blood or blood products, including India. But an investigation by India Today touted a black market of people willing to donate convalescent plasma for the equivalent of several hundred dollars. Officials vowed to prosecute, saying donations should be selfless.
But that enforcement threat seemed to be undercut when the health minister of the state of Assam declared "plasma donors will get preference in several government schemes including the government job interview." It appeared to be a form of compensation that far surpassed simple cash.
The small city of Rexburg, Idaho, with a population a bit over 50,000, overwhelmingly Mormon and home to a campus of Brigham Young University, at one point had one of the highest per capita rates of COVID-19 in the current wave of infection. Rumors circulated that some students were intentionally trying to become infected so they could later sell their plasma for top dollar, potentially as much as $200 a visit.
Troubled university officials investigated the allegations but could come up with nothing definitive; how does one prove intentionality with such an omnipresent yet elusive virus? They chalked it up to idle chatter, perhaps an urban legend, which might be associated with alcohol use on some other campus.
Doctors, hospitals, and drug companies are all rightly praised for their altruism in the fight against COVID-19, but they also get paid. Payment for whole blood donation in the U.S. is prohibited, and while payment for plasma is allowed, there is a stigma attached to payment and much plasma is donated for free. "Why do we expect the donors [of convalescent plasma] to be the only uncompensated people in the process? It really makes no sense," argues Mark Yarborough, an ethicist at the UC Davis School of Medicine in Sacramento.
"When I was in grad school, two of my closest friends, at least once a week they went and gave plasma. That was their weekend spending money," Yarborough recalls. He says upper and middle-income people may have the luxury of donating blood products but prohibiting people from selling their plasma is a bit paternalistic and doesn't do anything to improve the economic status of poor people.
"Asking people to dedicate two hours a week for an entire year in exchange for cookies and milk is demonstrably asking too much," says Peter Jaworski, an ethicist who teaches at Georgetown University.
He notes that companies that pay plasma donors have much lower total costs than do operations that rely solely on uncompensated donations. The companies have to spend less to recruit and retain donors because they increase payments to encourage regular repeat donations. They are able to more rationally schedule visits to maximize use of expensive apheresis equipment and medical personnel used for the collection.
It seems that COVID-19 has been with us forever, but in reality it is less than a year. We have learned much over that short time, can now better manage the disease, and have lower mortality rates to prove it. Just how much convalescent plasma may have contributed to that remains an open question. Access to vaccines is months away for many people, and even then some people will continue to get sick. Given the lack of proven treatments, it makes sense to keep plasma as part of the mix, and not close the door to any legitimate means to obtain it.