A model of a human kidney.
Science's dream of creating perfect custom organs on demand as soon as a patient needs one is still a long way off. But tiny versions are already serving as useful research tools and stepping stones toward full-fledged replacements.
Although organoids cannot yet replace kidneys, they are invaluable tools for research.
The Lowdown
Australian researchers have grown hundreds of mini human kidneys in the past few years. Known as organoids, they function much like their full-grown counterparts, minus a few features due to a lack of blood supply.
Cultivated in a petri dish, these kidneys are still a shadow of their human counterparts. They grow no larger than one-sixth of an inch in diameter; fully developed organs are up to five inches in length. They contain no more than a few dozen nephrons, the kidney's individual blood-filtering unit, whereas a fully-grown kidney has about 1 million nephrons. And the dish variety live for just a few weeks.
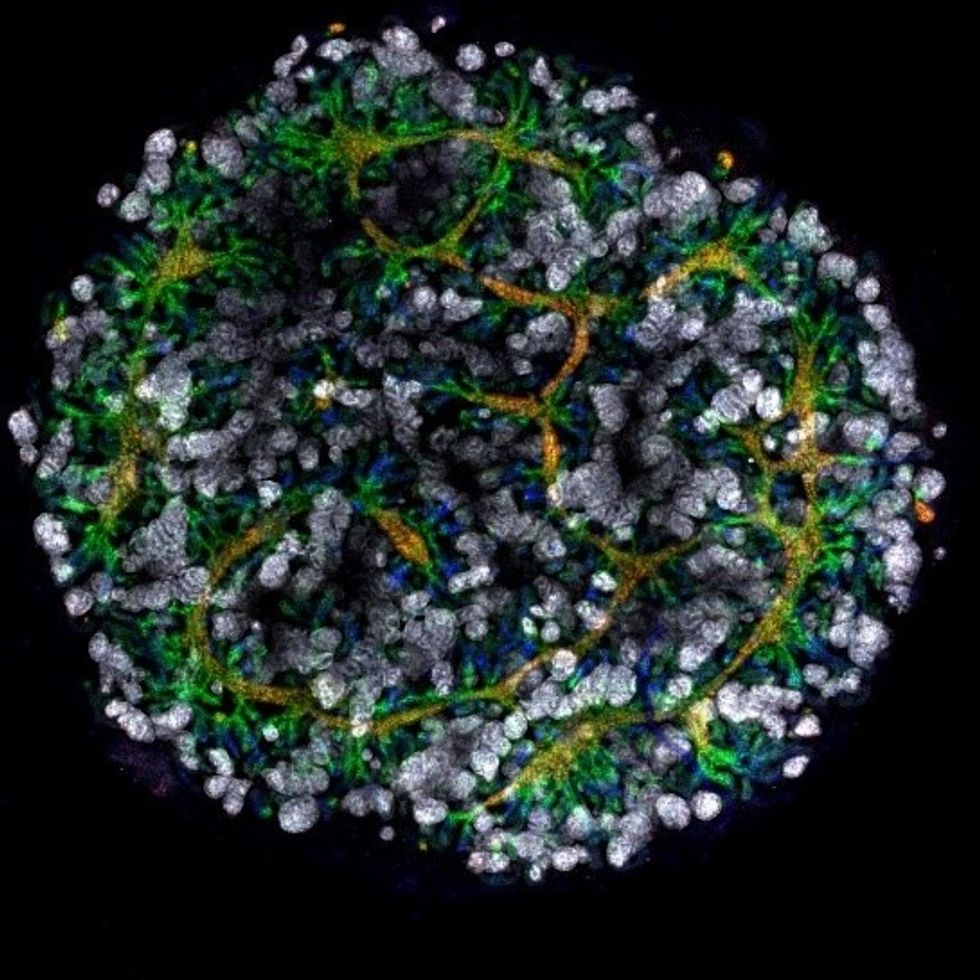
An organoid kidney created by the Murdoch Children's Institute in Melbourne, Australia.
Photo Credit: Shahnaz Khan.
But Melissa Little, head of the kidney research laboratory at the Murdoch Children's Institute in Melbourne, says these organoids are invaluable tools for research. Although renal failure is rare in children, more than half of those who suffer from such a disorder inherited it.
The mini kidneys enable scientists to better understand the progression of such disorders because they can be grown with a patient's specific genetic condition.
Mature stem cells can be extracted from a patient's blood sample and then reprogrammed to become like embryonic cells, able to turn into any type of cell in the body. It's akin to walking back the clock so that the cells regain unlimited potential for development. (The Japanese scientist who pioneered this technique was awarded the Nobel Prize in 2012.) These "induced pluripotent stem cells" can then be chemically coaxed to grow into mini kidneys that have the patient's genetic disorder.
"The (genetic) defects are quite clear in the organoids, and they can be monitored in the dish," Little says. To date, her research team has created organoids from 20 different stem cell lines.
Medication regimens can also be tested on the organoids, allowing specific tailoring for each patient. For now, such testing remains restricted to mice, but Little says it eventually will be done on human organoids so that the results can more accurately reflect how a given patient will respond to particular drugs.
Next Steps
Although these organoids cannot yet replace kidneys, Little says they may plug a huge gap in renal care by assisting in developing new treatments for chronic conditions. Currently, most patients with a serious kidney disorder see their options narrow to dialysis or organ transplantation. The former not only requires multiple sessions a week, but takes a huge toll on patient health.
Ten percent of older patients on dialysis die every year in the U.S. Aside from the physical trauma of organ transplantation, finding a suitable donor outside of a family member can be difficult.
"This is just another great example of the potential of pluripotent stem cells."
Meanwhile, the ongoing creation of organoids is supplying Little and her colleagues with enough information to create larger and more functional organs in the future. According to Little, researchers in the Netherlands, for example, have found that implanting organoids in mice leads to the creation of vascular growth, a potential pathway toward creating bigger and better kidneys.
And while Little acknowledges that creating a fully-formed custom organ is the ultimate goal, the mini organs are an important bridge step.
"This is just another great example of the potential of pluripotent stem cells, and I am just passionate to see it do some good."
Many patients in the African-American community are skeptical of new experimental treatments, thanks to a history of medical exploitation in the 20th century.
If any malady proves the fragile grace of the human genome, it is sickle cell disease.
If experimental treatments receive regulatory approval, it would be a watershed breakthrough for tens of thousands of Americans.
It occurs because of a single "misspelled" letter of DNA, causing red blood cells to run low on oxygen and transforming the hemoglobin in each cell into a stiff rod. Normally round cells become rigid crescents that hamper the flow of blood throughout the body, like leaves clumping in a drain.
Strokes in toddlers are merely the beginning of the circulatory calamities this disease may inflict. Most sickled cells cannot carry oxygen through the body, causing anemia as well as excruciating chronic pain. Older patients are at risk of kidney failure, heart disease and all the other collateral damage caused by poor circulation. Few live beyond middle age.
The only way to cure it has been through a bone marrow transplant from a donor, which requires not only a closely matching volunteer, but bouts of chemotherapy to allow new stem cells to take root, as well as rounds of immunosuppressive drugs that may last for years.
Recent advances in genomic medicine may soon alter the disease's outlook, although many obstacles remain.
In one treatment under development, patient's skin cells are converted into stem cells, allowing them to be inserted into the bone marrow without the need for a donor. Another treatment known as gene therapy involves replacing the aberrant gene in the patient's body with new genetic material.
Although both remain in clinical trials -- and also require at least chemotherapy -- they have shown promise. Matthew Hsieh, a hematologist and staff scientist with the National Heart Lung and Blood Institute in Maryland, has performed about 10 gene therapy procedures over the past three years as part of a clinical trial. Ongoing tweaks in the procedure have led to the blood in more recent patients showing sickle cell trait -- not a perfect outcome, but one that leaves patients with far fewer symptoms than if they have the full-blown disease.
If one or both treatments receive regulatory approval, it would be a watershed breakthrough for the tens of thousands of Americans who suffer from the disease.
Yet it is entirely possible many patients may decline the cure.
A Painful History
The vast majority of sickle cell sufferers in the U.S. -- well beyond 90 percent -- are African-American, a population with a historically uneasy relationship toward healthcare.
"There is a lot of data on distrust between African-Americans and American medical institutions," says J. Corey Williams, a psychiatrist with the Children's Hospital of Philadelphia who has written extensively on racial disparities in healthcare. "It comes from a long legacy of feeling victimized by medicine."
"What you hear from many patients is 'I am not going to be your guinea pig, and I am not going to be experimented on.'"
As a result, Williams is among several clinicians interviewed for this story who believe a cure for sickle cell disease would be embraced reluctantly.
"What you hear from many patients is 'I am not going to be your guinea pig, and I am not going to be experimented on.' And so the history of African-Americans and research will manifest as we develop gene therapies for [these] patients," says Christopher L. Edwards, a clinical psychologist and researcher with the Maya Angelou Center for Health Equity at the Wake Forest University School of Medicine.
Fear among African-Americans of becoming guinea pigs is well-founded. The first c-sections and fistula repairs occurring in North America were performed on enslaved women -- all without consent and virtually none with anesthesia.
Modern 20th century medicine led to the Tuskegee syphilis experiments conducted by the U.S. Public Health Service. Researchers withheld treatment from some 400 African-American men from the 1930s well into the 1970s to observe how they reacted to the disease -- even though curative antibiotics had been around for decades. Only news reports ended the experiment.
The long-standing distrust of American healthcare in the African-American community is also baked into the care provided to sickle cell patients. Despite affecting one in 365 African-Americans, there is no disease registry to assist clinical trials, according to Mary Hulihan, a blood disorders epidemiologist with the Centers for Disease Control and Prevention. Edwards says many sufferers are suspicious of being monitored.
Meanwhile, only two drugs are available to alleviate the worst symptoms. The first one, hydroxyurea, received FDA approval only in 1998 -- nearly 90 years after the disease was first diagnosed. Moreover, Edwards says that some sufferers shy away from using hydroxyurea because it is also used to treat cancer. It's part of what he calls the "myth and folklore" in the African-American community about sickle cell disease.
Economics plays a role as well in the often-fragmented care such patients receive. According to CDC data, many patients rely extensively on public insurance programs such as Medicaid, whose coverage varies from state to state.
A Tough Transition
Edwards notes that sickle cell sufferers usually receive good care when they're children because of support provided by family members. But that often breaks down in adulthood. According to CDC data, an adult sickle cell patient visits a hospital emergency room three times as often as a child patient.
The consensus is that the path to a medical cure for sickle cell will first need to be smoothed over with a talk cure.
Modupe Idowu, a hematologist with the University of Texas Health system, estimates that there are perhaps a dozen comprehensive care centers for the estimated 100,000 sickle cell patients in the U.S., including the one she operates in Houston. That means a significant proportion of those afflicted are on their own to procure care.
And since many patients are on Medicaid, "a lot of hematologists that train to take care of blood disorders, many are not interested in treating [sickle cell disease] because the reimbursement for providers is not great," Idowu says.
Hsieh acknowledges that many of his patients can be suspicious about the care they are receiving. Frustration with fragmented care is usually the biggest driver, he adds.
Meanwhile, the skepticism that patients have about the treatments they seek is often reciprocated by their caregivers.
"The patients have experiences with medication and know what works at a very young age (for their pain)," Edwards says. Such expertise demonstrated by an African-American patient often leads to them being labeled as narcotics seekers.
The Correct Path
This all begs the question of how to deploy a cure. Idowu, who regularly holds town hall-style meetings with Houston-area patients, often must allay anxieties. For example, the gene therapy approach uses a harmless virus to transport new genetic material into cells. That virus happens to be a benign version of HIV, and convincing patients they won't be infected with HIV is a fraught issue.
The consensus is that the path to a medical cure for sickle cell will first need to be smoothed over with a talk cure.
Idowu tries to hammer home the fact that patients are afforded vastly more protections than in the past. "There are a lot of committees and investigational review boards that keep track of clinical trials; things just don't happen anymore as they did in the past," she says. She also believes it helps if more providers of color communicate to patients.
Hsieh is very straightforward with his patients. He informs them about the HIV vector but assures them no one has ever tested positive for the virus as a result of its use.
Edwards notes that since many patients suffer psychosocial trauma as a result of their chronic pain, there already is some counseling infrastructure in place to help them cope. He believes such resources will have to be stretched further as a cure looms closer.
In the absence of formal mental health services, straight talk may be the best way to overcome wariness.
"If patients have misgivings, we try our best to address them, and let them know at the end of the day it is their decision to make," Hsieh says. "And even the patients who have gone through the gene therapy and it didn't work well -- they're still glad they took the chance."
How Genetic Engineering Could Save the Coral Reefs
Underwater world with corals and tropical fish.
Coral reefs are usually relegated to bit player status in television and movies, providing splashes of background color for "Shark Week," "Finding Nemo," and other marine-based entertainment.
In real life, the reefs are an absolutely crucial component of the ecosystem for both oceans and land, rivaling only the rain forests in their biological complexity. They provide shelter and sustenance for up to a quarter of all marine life, oxygenate the water, help protect coastlines from erosion, and support thousands of tourism jobs and businesses.
Genetic engineering could help scientists rebuild the reefs that have been lost, and turn those still alive into a souped-up version that can withstand warmer and even more acidic waters.
But the warming of the world's oceans -- exacerbated by an El Nino event that occurred between 2014 and 2016 -- has been putting the world's reefs under tremendous pressure. Their vibrant colors are being replaced by sepulchral whites and tans.
That's the result of bleaching -- a phenomenon that occurs when the warming waters impact the efficiency of the algae that live within the corals in a symbiotic relationship, providing nourishment via photosynthesis and eliminating waste products. The corals will often "shuffle" their resident algae, reacting in much the same way a landlord does with a non-performing tenant -- evicting them in the hopes of finding a better resident. But when better-performing algae does not appear, the corals become malnourished, eventually becoming deprived of their color and then their lives.
The situation is dire: Two-thirds of Australia's Great Barrier Reef have undergone a bleaching event in recent years, and it's believed up to half of that reef has died.
Moreover, hard corals are the ocean's redwood trees. They take centuries to grow, meaning it could take centuries or more to replace them.
Recent developments in genetic engineering -- and an accidental discovery by researchers at a Florida aquarium -- provide opportunities for scientists to potentially rebuild a large proportion of the reefs that have been lost, and perhaps turn those still alive into a souped-up version that can withstand warmer and even more acidic waters. But many questions have yet to be answered about both the biological impact on the world's oceans, and the ethics of reengineering the linchpin of its ecosystem.
How did we get here?
Coral bleaching was a regular event in the oceans even before they began to warm. As a result, natural selection weeds out the weaker species, says Rachel Levin, an American-born scientist who has performed much of her graduate work in Australia. But the current water warming trend is happening at a much higher rate than it ever has in nature, and neither the coral nor the algae can keep up.
"There is a big concern about giving one variant a huge fitness advantage, have it take over and impact the natural variation that is critical in changing environments."
In a widely-read paper published last year in the journal Frontiers in Microbiology, Levin and her colleagues put forth a fairly radical notion for preserving the coral reefs: Genetically modify their resident algae.
Levin says the focus on algae is a pragmatic decision. Unlike coral, they reproduce extremely rapidly. In theory, a modified version could quickly inhabit and stabilize a reef. About 70 percent of algae -- all part of the genus symbiodinium -- are host generalists. That means they will insert themselves into any species of coral.
In recent years, work on mapping the genomes of both algae and coral has been progressing rapidly. Scientists at Stanford University have recently been manipulating coral genomes using larvae manipulated with the CRISPR/Cas9 technology, although the experimentation has mostly been limited to its fluorescence.
Genetically modifying the coral reefs could seem like a straightforward proposition, but complications are on the horizon. Levin notes that as many as 20 different species of algae can reside within a single coral, so selecting the best ones to tweak may pose a challenge.
"The entire genus is made up of thousands of subspecies, all very genetically distinct variants. There is a huge genetic diversity, and there is a big concern about giving one variant a huge fitness advantage, have it take over and impact the natural variation that is critical in changing environments," Levin says.
Genetic modifications to an algae's thermal tolerance also poses the risk of what Levin calls an "off-target effect." That means a change to one part of the genome could lead to changes in other genes, such as those regulating growth, reproduction, or other elements crucial to its relationship with coral.
Phillip Cleves, a postdoctoral researcher at Stanford who has participated in the CRISPR/Cas9 work, says that future research will focus on studying the genes in coral that regulate the relationship with the algae. But he is so concerned about the ethical issues of genetically manipulating coral to adapt to a changing climate that he declined to discuss it in detail. And most coral species have not yet had their genomes fully mapped, he notes, suggesting that such work could still take years.
An Alternative: Coral Micro-fragmentation
In the meantime, there is another technique for coral preservation led by David Vaughan, senior scientist and program manager at the Mote Marine Laboratory and Aquarium in Sarasota, Florida.
Vaughan's research team has been experimenting in the past decade with hard coral regeneration. Their work had been slow and painstaking, since growing larvae into a coral the size of a quarter takes three years.
The micro-fragmenting process in some ways raises fewer ethical questions than genetically altering the species.
But then, one day in 2006, Vaughan accidentally broke off a tiny piece of coral in the research aquarium. That fragment grew to the size of a quarter in three months, apparently the result of the coral's ability to rapidly regenerate when injured. Further research found that breaking coral in this manner -- even to the size of a single polyp -- led to rapid growth in more than two-dozen species.
Mote is using this process, known as micro-fragmentation, to grow large numbers of coral rapidly, often fusing them on top of larger pieces of dead coral. These coral heads are then planted in the Florida Keys, which has experienced bleaching events over 12 of the last 14 years. The process has sped up almost exponentially; Mote has planted some 36,000 pieces of coral to date, but Vaughan says it's on track to plant 35,000 more pieces this year alone. That sum represents between 20 to 30 acres of restored reef. Mote is on track to plant another 100,000 pieces next year.
This rapid reproduction technique in some ways allows Mote scientists to control for the swift changes in ocean temperature, acidification and other factors. For example, using surviving pieces of coral from areas that have undergone bleaching events means these hardier strains will propagate much faster than nature allows.
Vaughan recently visited the Yucatan Peninsula to work with Mexican researchers who are going to embark on a micro-fragmenting initiative of their own.
The micro-fragmenting process in some ways raises fewer ethical questions than genetically altering the species, although Levin notes that this could also lead to fewer varieties of corals on the ocean floor -- a potential flattening of the colorful backdrops seen in television and movies.
But Vaughan has few qualms, saying this is an ecological imperative. He suggests that micro-fragmentation could serve as a stopgap until genomic technologies further advance.
"We have to use the technology at hand," he says. "This is a lot like responding when a forest burns down. We don't ask questions. We plant trees."