Vaccine Passports Are a Premature Solution to A Challenging Problem

Vaccine passports, if required by businesses and universities, may give people a false sense of security, one expert cautions.
Vaccines are one of the greatest public health accomplishments of all time. For centuries, public health has relied on vaccinations to prevent and control disease outbreaks for a plethora of infectious scourges, with our crowning achievement being the successful eradication of smallpox.
The purpose of vaccine documentation is to provide proof of an individual's protection from either becoming infected or transmitting a vaccine-preventable disease. Vouching for these protections requires a firm knowledge about the epidemiology of the disease, as well as scientific knowledge concerning the efficacy of the vaccine. The vaccines we currently require be documented have met these tests; the vaccine for COVID-19 has not yet been proven to do so.
Let's acknowledge that the term "vaccine passport" is a poor choice of words. Passports are a legal travel document created by nations and governed by law for identification of the bearer to control entry and exit from nation states. They often serve as legal forms of identification and as a record of international travel. They are generally very sophisticated documents that have been created in a secure manner and may include a range of electronic and, in some cases, biometric measures such as fingerprints to ensure the holder is indeed who they say they are. Vaccine passports are medical documents used to document the vaccination status of an individual. They do not undergo the same level of administrative scrutiny and cannot be used to verify that the presenter is indeed the vaccinated individual. Some companies do have electronic methods to address concerns about verification; however, most people currently have paper records that can be easily falsified.
"Vaccine passports" as currently proposed risk giving people a false sense of security.
Successful disease control from vaccination programs relies on the ability to vaccinate at a level that prevents large-scale disease spread and the ability to rapidly identify the presence of disease outbreaks. It requires reliable, safe, and effective vaccines that are easily delivered in clinical and nonclinical settings. Keeping vaccination information as a part of the medical record, and even having a separate specialized vaccine record for personal use, is a time-honored tradition.
Keeping a vaccination record provides a method to keep track of the many shots one receives and serves as a visual reminder to help ensure the appropriate vaccine shot schedule is maintained for vaccines requiring multiple doses. The vaccine record, when combined with vaccine safety monitoring systems, serves as a mechanism to track adverse events to monitor and ensure the safety of vaccines as a consumer product. The record also serves as the official record of vaccination when required for administrative or legally prescribed purposes.
"Vaccine passports" as currently proposed risk giving people a false sense of security. In the case of the COVID-19 vaccines currently approved for use, many of the essential questions remain unanswered. While we do know the current three vaccines are highly protective against severe disease and death, and there is some evidence that these vaccinations do reduce infections and virus transmission of SARS-CoV-2, we do not yet know the full degree to which this occurs.
For example, we know there have been some cases of people that have been infected in close proximity to getting their full vaccination and rare cases of breakthrough reinfections. A breakthrough infection in a restaurant is a challenge for contact tracing, but an outbreak from a movie theater exposure or a baseball game could spark a major outbreak at our current level of vaccination. Current CDC guidance recommends continued mask wearing in order to address these concerns.
We also do not yet know how long the protections will last and if or when a booster or revaccination is required. In effect, it is too soon to know. Should an annual booster shot be required, then a vaccine passport would require annual updating, a process more frequent than renewal of a driver's license.
We also know that the current SARS-CoV-2 virus is mutating briskly. While the current approved vaccines have remained effective overall, there is evidence of some degree of degradation in vaccine effectiveness against some of the circulating strains. We also have sparse data on many of the other emerging strains of concern because we have not had the surveillance capacity in the U.S. to gain an adequate sense of how the virus is changing to fully align vaccine effectiveness with viral capabilities.
The risk of people misusing these "passports" is troubling. The potential for using these documents for hiring, firing or job limitation is a serious concern. Unvaccinated workers are at risk of this form of discrimination even from well-meaning employers or supervisors. Health insurers are prohibited by the Affordable Care Act from discriminating based on preexisting conditions, but they could probably charge a higher premium for unvaccinated individuals. There also is a risk of stigmatizing individuals who are not vaccinated or have left their vaccine documentation at home. Another concern: the opportunity to discriminate based on race, gender, sexual orientation, or religion, using one's vaccination status as an excuse.
These "passports" are being discussed as a "ticket verification" for entry to many activities, including dining at restaurants, flying domestically and/or internationally, going to movie theaters and sporting events, etc. These are all activities we already are doing at reduced levels and for which wearing a mask, hand hygiene and physical distancing are effective disease control practices. COVID-19 vaccines are indeed the measure that will make the ability to totally reopen our society complete, but we are not there yet. Documentation of one's COVID-19 vaccine status may be useful in selected situations in the future. That remains to be seen.
Finally, inadequate vaccine supply and disparities in vaccine delivery have created enormous challenges in providing equal access to vaccination. Also, the amount of misinformation, disinformation, and lingering vaccine hesitancy continue to limit the speed at which we will reach the level of vaccination of the population that would make this documentation meaningful. The requirement for "vaccine passports" is already alienating people who are opposed to vaccinations for a variety of reasons, paradoxically risking reduced vaccine uptake. This politicization of the vaccination effort is of concern. There are indeed people who, due to medical contraindications or legal exemptions, will not be vaccinated, and we do not yet have a national framework on how to address this.
Vaccine passports are not the solution for reopening our society — a robust vaccination program is. The requirement to document one's vaccination status for COVID-19 may one day have its place. For now, it is an idea whose time has not yet come.
Editor's Note: This op/ed is part of a "Big Question" series on the ethics of vaccine passports. Read the flip side argument here.
In this week's Friday Five, an old diabetes drug finds an exciting new purpose. Plus, how to make the cities of the future less toxic, making old mice younger with EVs, a new reason for mysterious stillbirths - and much more.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Here is the promising research covered in this week's Friday Five:
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
- How to make cities of the future less noisy
- An old diabetes drug could have a new purpose: treating an irregular heartbeat
- A new reason for mysterious stillbirths
- Making old mice younger with EVs
- No pain - or mucus - no gain
And an honorable mention this week: How treatments for depression can change the structure of the brain
Researchers at Stanford have found that the virus that causes Covid-19 can infect fat cells, which could help explain why obesity is linked to worse outcomes for those who catch Covid-19.
Obesity is a risk factor for worse outcomes for a variety of medical conditions ranging from cancer to Covid-19. Most experts attribute it simply to underlying low-grade inflammation and added weight that make breathing more difficult.
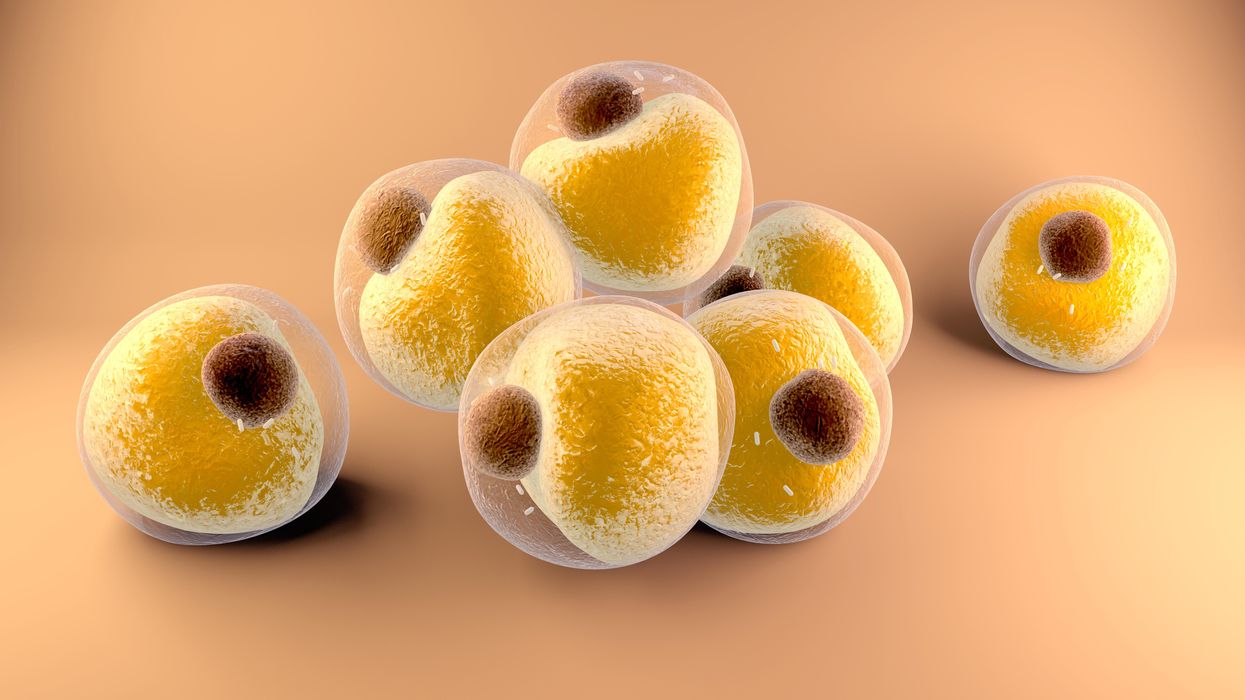
Now researchers have found a more direct reason: SARS-CoV-2, the virus that causes Covid-19, can infect adipocytes, more commonly known as fat cells, and macrophages, immune cells that are part of the broader matrix of cells that support fat tissue. Stanford University researchers Catherine Blish and Tracey McLaughlin are senior authors of the study.
Most of us think of fat as the spare tire that can accumulate around the middle as we age, but fat also is present closer to most internal organs. McLaughlin's research has focused on epicardial fat, “which sits right on top of the heart with no physical barrier at all,” she says. So if that fat got infected and inflamed, it might directly affect the heart.” That could help explain cardiovascular problems associated with Covid-19 infections.
Looking at tissue taken from autopsy, there was evidence of SARS-CoV-2 virus inside the fat cells as well as surrounding inflammation. In fat cells and immune cells harvested from health humans, infection in the laboratory drove "an inflammatory response, particularly in the macrophages…They secreted proteins that are typically seen in a cytokine storm” where the immune response runs amok with potential life-threatening consequences. This suggests to McLaughlin “that there could be a regional and even a systemic inflammatory response following infection in fat.”
It is easy to see how the airborne SARS-CoV-2 virus infects the nose and lungs, but how does it get into fat tissue? That is a mystery and the source of ample speculation.
The macrophages studied by McLaughlin and Blish were spewing out inflammatory proteins, While the the virus within them was replicating, the new viral particles were not able to replicate within those cells. It was a different story in the fat cells. “When [the virus] gets into the fat cells, it not only replicates, it's a productive infection, which means the resulting viral particles can infect another cell,” including microphages, McLaughlin explains. It seems to be a symbiotic tango of the virus between the two cell types that keeps the cycle going.
It is easy to see how the airborne SARS-CoV-2 virus infects the nose and lungs, but how does it get into fat tissue? That is a mystery and the source of ample speculation.
Macrophages are mobile; they engulf and carry invading pathogens to lymphoid tissue in the lymph nodes, tonsils and elsewhere in the body to alert T cells of the immune system to the pathogen. Perhaps some of them also carry the virus through the bloodstream to more distant tissue.
ACE2 receptors are the means by which SARS-CoV-2 latches on to and enters most cells. They are not thought to be common on fat cells, so initially most researchers thought it unlikely they would become infected.
However, while some cell receptors always sit on the surface of the cell, other receptors are expressed on the surface only under certain conditions. Philipp Scherer, a professor of internal medicine and director of the Touchstone Diabetes Center at the University of Texas Southwestern Medical Center, suggests that, in people who have obesity, “There might be higher levels of dysfunctional [fat cells] that facilitate entry of the virus,” either through transiently expressed ACE2 or other receptors. Inflammatory proteins generated by macrophages might contribute to this process.
Another hypothesis is that viral RNA might be smuggled into fat cells as cargo in small bits of material called extracellular vesicles, or EVs, that can travel between cells. Other researchers have shown that when EVs express ACE2 receptors, they can act as decoys for SARS-CoV-2, where the virus binds to them rather than a cell. These scientists are working to create drugs that mimic this decoy effect as an approach to therapy.
Do fat cells play a role in Long Covid? “Fat cells are a great place to hide. You have all the energy you need and fat cells turn over very slowly; they have a half-life of ten years,” says Scherer. Observational studies suggest that acute Covid-19 can trigger the onset of diabetes especially in people who are overweight, and that patients taking medicines to regulate their diabetes “were actually quite protective” against acute Covid-19. Scherer has funding to study the risks and benefits of those drugs in animal models of Long Covid.
McLaughlin says there are two areas of potential concern with fat tissue and Long Covid. One is that this tissue might serve as a “big reservoir where the virus continues to replicate and is sent out” to other parts of the body. The second is that inflammation due to infected fat cells and macrophages can result in fibrosis or scar tissue forming around organs, inhibiting their function. Once scar tissue forms, the tissue damage becomes more difficult to repair.
Current Covid-19 treatments work by stopping the virus from entering cells through the ACE2 receptor, so they likely would have no effect on virus that uses a different mechanism. That means another approach will have to be developed to complement the treatments we already have. So the best advice McLaughlin can offer today is to keep current on vaccinations and boosters and lose weight to reduce the risk associated with obesity.