Life is Emerging: Review of Siddhartha Mukherjee’s Song of the Cell
A new book by Pulitzer-winning physician-scientist Siddhartha Mukherjee will be released from Simon & Schuster on October 25, 2022.
The DNA double helix is often the image spiraling at the center of 21st century advances in biomedicine and the growing bioeconomy. And yet, DNA is molecularly inert. DNA, the code for genes, is not alive and is not strictly necessary for life. Ought life be at the center of our communication of living systems? Is not the Cell a superior symbol of life and our manipulation of living systems?
A code for life isn’t a code without the life that instantiates it. A code for life must be translated. The cell is the basic unit of that translation. The cell is the minimal viable package of life as we know it. Therefore, cell biology is at the center of biomedicine’s greatest transformations, suggests Pulitzer-winning physician-scientist Siddhartha Mukherjee in his latest book, The Song of the Cell: The Exploration of Medicine and the New Human.
The Song of the Cell begins with the discovery of cells and of germ theory, featuring characters such as Louis Pasteur and Robert Koch, who brought the cell “into intimate contact with pathology and medicine.” This intercourse would transform biomedicine, leading to the insight that we can treat disease by thinking at the cellular level. The slightest rearrangement of sick cells might be the path toward alleviating suffering for the organism: eroding the cell walls of a bacterium while sparing our human cells; inventing a medium that coaxes sperm and egg to dance into cellular union for in vitro fertilization (IVF); designing molecular missiles that home to the receptors decorating the exterior of cancer cells; teaching adult skin cells to remember their embryonic state for regenerative medicines.
Mukherjee uses the bulk of the book to elucidate key cell types in the human body, along with their “connective relationships” that enable key organs and organ systems to function. This includes the immune system, the heart, the brain, and so on. Mukherjee’s distinctive style features compelling anecdotes and human stories that animate the scientific (and unscientific) processes that have led to our current state of understanding. In his chapter on neurons and the brain, for example, he integrates Santiago Ramon y Cajal’s meticulous black ink sketches of neurons into Mukherjee’s own personal encounter with clinical depression. In one lucid section, he interviews Dr. Helen Mayberg, a pioneering neurologist who takes seriously the descriptive power of her patients’ metaphors, as they suffer from “caves,” “holes,” “voids,” and “force fields” that render their lives gray. Dr. Mayberg aims to stimulate patients’ neuronal cells in a manner that brings back the color.
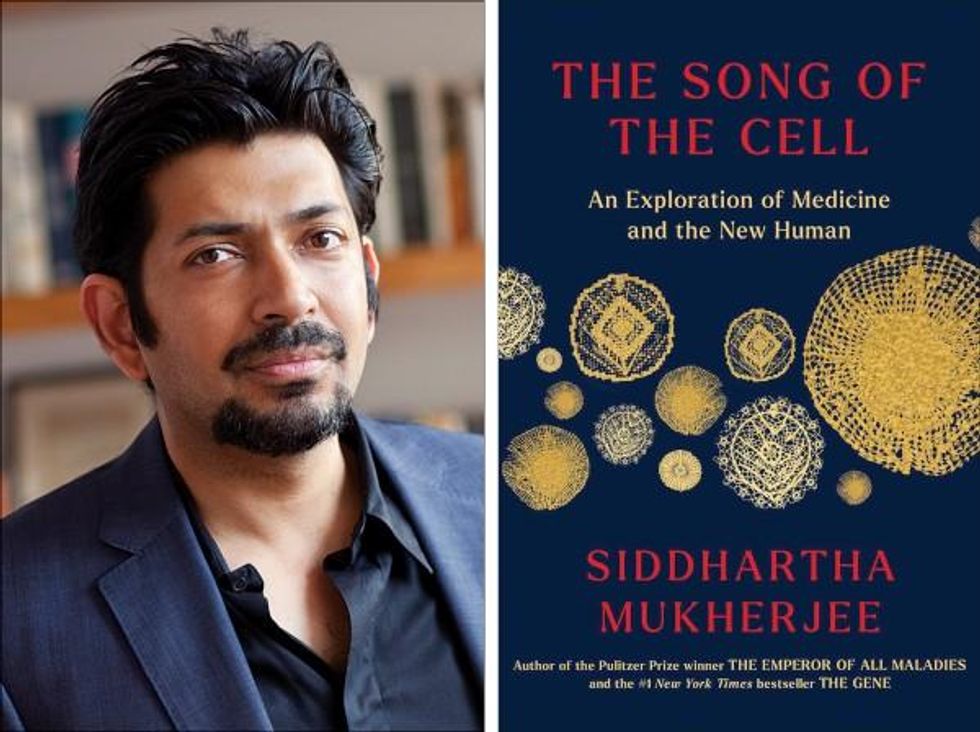
Beyond exposing the insight and inventiveness that has arisen out of cell-based thinking, it seems that Mukherjee’s bigger project is an epistemological one. The early chapters of The Song of the Cell continually hint at the potential for redefining the basic unit of biology as the cell rather than the gene. The choice to center biomedicine around cells is, above all, a conspicuous choice not to center it around genes (the subject of Mukherjee’s previous book, The Gene), because genes dominate popular science communication.
This choice of cells over genes is most welcome. Cells are alive. Genes are not. Letters—such as the As, Cs, Gs, and Ts that represent the nucleotides of DNA, which make up our genes—must be synthesized into a word or poem or song that offers a glimpse into deeper truths. A key idea embedded in this thinking is that of emergence. Whether in ancient myth or modern art, creation tends to be an emergent process, not a linearly coded script. The cell is our current best guess for the basic unit of life’s emergence, turning a finite set of chemical building blocks—nucleic acids, proteins, sugars, fats—into a replicative, evolving system for fighting stasis and entropy. The cell’s song is one for our times, for it is the song of biology’s emergence out of chemistry and physics, into the “frenetically active process” of homeostasis.
Re-centering our view of biology has practical consequences, too, for how we think about diagnosing and treating disease, and for inventing new medicines. Centering cells presents a challenge: which type of cell to place at the center? Rather than default to the apparent simplicity of DNA as a symbol because it represents the one master code for life, the tension in defining the diversity of cells—a mapping process still far from complete in cutting-edge biology laboratories—can help to create a more thoughtful library of cellular metaphors to shape both the practice and communication of biology.
Further, effective problem solving is often about operating at the right level, or the right scale. The cell feels like appropriate level at which to interrogate many of the diseases that ail us, because the senses that guide our own perceptions of sickness and health—the smoldering pain of inflammation, the tunnel vision of a migraine, the dizziness of a fluttering heart—are emergent.
This, unfortunately, is sort of where Mukherjee leaves the reader, under-exploring the consequences of a biology of emergence. Many practical and profound questions have to do with the ways that each scale of life feeds back on the others. In a tome on Cells and “the future human” I wished that Mukherjee had created more space for seeking the ways that cells will shape and be shaped by the future, of humanity and otherwise.
We are entering a phase of real-world bioengineering that features the modularization of cellular parts within cells, of cells within organs, of organs within bodies, and of bodies within ecosystems. In this reality, we would be unwise to assume that any whole is the mere sum of its parts.
For example, when discussing the regenerative power of pluripotent stem cells, Mukherjee raises the philosophical thought experiment of the Delphic boat, also known as the Ship of Theseus. The boat is made of many pieces of wood, each of which is replaced for repairs over the years, with the boat’s structure unchanged. Eventually none of the boat’s original wood remains: Is it the same boat?
Mukherjee raises the Delphic boat in one paragraph at the end of the chapter on stem cells, as a metaphor related to the possibility of stem cell-enabled regeneration in perpetuity. He does not follow any of the threads of potential answers. Given the current state of cellular engineering, about which Mukherjee is a world expert from his work as a physician-scientist, this book could have used an entire section dedicated to probing this question and, importantly, the ways this thought experiment falls apart.
We are entering a phase of real-world bioengineering that features the modularization of cellular parts within cells, of cells within organs, of organs within bodies, and of bodies within ecosystems. In this reality, we would be unwise to assume that any whole is the mere sum of its parts. Wholeness at any one of these scales of life—organelle, cell, organ, body, ecosystem—is what is at stake if we allow biological reductionism to assume away the relation between those scales.
In other words, Mukherjee succeeds in providing a masterful and compelling narrative of the lives of many of the cells that emerge to enliven us. Like his previous books, it is a worthwhile read for anyone curious about the role of cells in disease and in health. And yet, he fails to offer the broader context of The Song of the Cell.
As leading agronomist and essayist Wes Jackson has written, “The sequence of amino acids that is at home in the human cell, when produced inside the bacterial cell, does not fold quite right. Something about the E. coli internal environment affects the tertiary structure of the protein and makes it inactive. The whole in this case, the E. coli cell, affects the part—the newly made protein. Where is the priority of part now?” [1]
Beyond the ways that different kingdoms of life translate the same genetic code, the practical situation for humanity today relates to the ways that the different disciplines of modern life use values and culture to influence our genes, cells, bodies, and environment. It may be that humans will soon become a bit like the Delphic boat, infused with the buzz of fresh cells to repopulate different niches within our bodies, for healthier, longer lives. But in biology, as in writing, a mixed metaphor can cause something of a cacophony. For we are not boats with parts to be replaced piecemeal. And nor are whales, nor alpine forests, nor topsoil. Life isn’t a sum of parts, and neither is a song that rings true.
[1] Wes Jackson, "Visions and Assumptions," in Nature as Measure (p. 52-53).
You won't score many glamor points for using a neti pot, but it could be a worthwhile asset in fighting Covid-19, according to the author's experience and recent research.
Twice a day, morning and night, I use a neti pot to send a warm saltwater solution coursing through one nostril and out the other to flush out debris and pathogens. I started many years ago because of sinus congestion and infections and it has greatly reduced those problems. Along with vaccination when it became available, it seems to have helped with protecting me from developing Covid-19 symptoms despite being of an age and weight that puts me squarely at risk.
Now that supposition of protection has been backed up with evidence from a solidly designed randomized clinical trial. It found that irrigating your sinuses twice a day with a simple saltwater solution can lead to an 8.5-fold reduction in hospitalization from Covid-19. The study is another example of recent research that points to easy and inexpensive ways to help protect yourself and help control the epidemic.
Amy Baxter, the physician researcher behind the study at Augusta University, Medical College of Georgia, began the study in 2020, before a vaccine or monoclonal antibodies became available to counter the virus. She wanted to be able to offer another line of defense for people with limited access to healthcare.
The nasal cavity is the front door that the SARS-CoV-2 virus typically uses to enter the body, latching on to the ACE2 receptors on cells lining those tissue compartments to establish infection. Once the virus replicates here, infection spreads into the lungs and often other parts of the body, including the brain and gut. Some studies have shown that a mouthwash could reduce the viral load, but any effect on disease progression was less clear. Baxter reasoned that reducing the amount of virus in the nose might give the immune system a better chance to react and control that growth before it got out of hand.
She decided to test this approach in patients who had just tested positive for Covid-19, were over 55 years of age, and often had other risk factors for developing serious symptoms. It was the quickest and easiest way to get results. A traditional prevention study would have required many more volunteers, taken a longer period of follow up, and cost money she did not have.
The trial enrolled 79 participants within 24 hours of testing positive for Covid-19, and they agreed to follow the regimen of twice daily nasal irrigation. They were followed for 28 days. One patient was hospitalized; a 1.27% rate compared with 11% in a national sample control group of similar age people who tested positive for Covid-19. Patients who strictly adhered to nasal irrigation had fewer, shorter and less severe symptoms than people in the study who missed some of their saline rinses.
Baxter initially made the results of her clinical trial available as a preprint in the summer of 2021 and was dismayed when many of the comments were from anti-vaxxers who argued this was a reason why you did not need to get vaccinated. That was not her intent.
There are several mechanisms that explain why warm saltwater is so effective. First and most obvious is the physical force of the water that sweeps away debris just as a rainstorm sends trash into a street gutter and down a storm drain. It also lubricates the cilia, small hair-like structures whose job it is to move detritus away from cells for expulsion. Cilia are rich in ACE2 receptors and keeping them moving makes it harder for the virus to latch on to the receptors.
It turns out the saline has a direct effect on the virus itself. SARS-CoV-2 becomes activated when an enzyme called furin snips off part of its molecular structure, which allows the virus to grab on to the ACE2 receptor, but saline inhibits this process. Once inside a cell the virus replicates best in a low salt environment, but nasal cells absorb salt from the irrigation, which further slows viral replication, says Baxter.
Finally, “salt improves the jellification of liquid, it makes better and stickier mucus so that you can get those virus out,” she explains, lamenting, “Nobody cares about snot. I do now.”
She initially made the results of her clinical trial available as a preprint in the summer of 2021 and was dismayed when many of the comments were from anti-vaxxers who argued this was a reason why you did not need to get vaccinated. That was not her intent. Two journals rejected the paper, and Baxter believes getting caught up in the polarizing politics of Covid-19 was an important part of the reason why. She says that editors “didn't want to be associated with something that was being used by anti-vaxxers.” She strongly supports vaccination but realizes that additional and alternative approaches also are needed.
Premeasured packets of saline are inexpensive and can be purchased at any drug store. They are safe to use several times a day. Say you’re vaccinated but were in a situation where you fear you might have been exposed to SARS-CoV-2; an extra irrigation will clear out your sinuses and may reduce the risk of that possible exposure.
Baxter plans no further study in this area. She is returning to her primary research focus, which is pain control and reducing opioid use, but she hopes that others will expand on what she had done.
A couple holds up a picture of their ultrasound.
By now you have probably heard something about CRISPR, the simple and relatively inexpensive method of precisely editing the genomes of plants, animals, and humans.
The treatment of disease in fetuses, the liminal category of life between embryos and humans, poses the next frontier.
Through CRISPR and other methods of gene editing, scientists have produced crops to be more nutritious, better able to resist pests, and tolerate droughts; engineered animals ranging from fruit flies to monkeys to make them better suited for scientific study; and experimentally treated the HIV virus, Hepatitis B, and leukemia in human patients.
There are also currently FDA-approved trials to treat blindness, cancer, and sickle cell disease in humans using gene editing, and there is consensus that CRISPR's therapeutic applications will grow significantly in the coming years.
While the treatment of human disease through use of gene editing is not without its medical and ethical concerns, the avoidance of disease in embryos is far more fraught. Nonetheless, Naturereported in November that He Jiankui, a scientist in China, had edited twin embryos to disable a gene called CCR5 in hopes of avoiding transmission of HIV from their HIV-positive father.
Though there are questions about the effectiveness and necessity of this therapy, He reported that sequencing has proven his embryonic gene edits were successful and the twins were "born normal and healthy," although his claims have not been independently verified.
More recently, Denis Rebrikov, a Russian scientist, announced his plans to disable the same gene in embryos to be implanted in HIV-positive women later this year. Futuristic as it may seem, prenatal gene editing is already here.
The treatment of disease in fetuses, the liminal category of life between embryos and humans, poses the next frontier. Numerous conditions—some minor, some resulting in a lifetime of medical treatment, some incompatible with life outside of the womb—can be diagnosed through use of prenatal diagnostic testing. There is promising research suggesting doctors will soon be able to treat or mitigate at least some of them through use of fetal gene editing.
This research could soon present women carrying genetically anomalous fetuses a third option aside from termination or birthing a child who will likely face a challenging and uncertain medical future: Whether to undergo a fetal genetic intervention.
However, genetic intervention will open the door to a host of ethical considerations, particularly with respect to the relationship between pregnant women and prenatal genetic counselors. Current counselors theoretically provide objective information and answer questions rather than advise their pregnant client whether to continue with her pregnancy, despite the risks, or to have an abortion.
In practice, though, prenatal genetic counseling is most often directive, and the nature of the counseling pregnant women receive can depend on numerous factors, including their religious and cultural beliefs, their perceived ability to handle a complicated pregnancy and subsequent birth, and their financial status. Introducing the possibility of a fetal genetic intervention will exacerbate counselor reliance upon these considerations and in some cases lead to counseling that is even more directive.
Some women in the near future will face the choice of whether to abort, keep, or treat a genetically anomalous fetus.
Future counselors will have to figure out under what circumstances it is even appropriate to broach the subject. Should they only discuss therapies that are FDA-approved, or should they mention experimental treatments? What about interventions that are available in Europe or Asia, but banned in the United States? Or even in the best case of scenario of an FDA-approved treatment, should a counselor make reference to it if she knows for a fact that her client cannot possibly afford it?
Beyond the basic question of what information to share, counselors will have to confront the fact that the very notion of fixing or "editing" offspring will be repugnant to many women, and inherent in the suggestion is the stigmatization of individuals with disabilities. Prenatal genetic counselors will be on the forefront of debates surrounding which fetuses should remain as they are and which ones should be altered.
Despite these concerns, some women in the near future will face the choice of whether to abort, keep, or treat a genetically anomalous fetus in utero. Take, for example, a woman who learns during prenatal testing that her fetus has Angelman syndrome, a genetic disorder characterized by intellectual disability, speech impairment, loss of muscle control, epilepsy, and a small head. There is currently no human treatment for Angelman syndrome, which is caused by a loss of function in a single gene, UBE3A.
But scientists at the University of North Carolina have been able to treat Angelman syndrome in fetal mice by reactivating UBE3A through use of a single injection. The therapy has also proven effective in cultured human brain cells. This suggests that a woman might soon have to consider injecting her fetus's brain with a CRISPR concoction custom-designed to target UBE3A, rather than terminate her pregnancy or bring her fetus to term unaltered.
Assuming she receives the adequate information to make an informed choice, she too will face an ethical conundrum. There will be the inherent risks of injecting anything into a developing fetus's brain, including the possibility of infection, brain damage, and miscarriage. But there are also risks specific to gene editing, such as so-called off-target effects, the possibility of impacting genes other than the intended one. Such effects are highly unpredictable and can be difficult to detect. So too is it impossible to predict how altering UBE3A might lead to other genetic and epigenetic changes once the baby is born.
There are no easy answers to the many questions that will arise in this space.
A woman deciding how to act in this scenario must balance these risks against the potential benefits of the therapy, layered on top of her belief system, resources, and personal ethics. The calculus will be different for every woman, and even the same woman might change her mind from one pregnancy to the next based on the severity of the condition diagnosed and other available medical options.
Her genetic counselor, meanwhile, must be sensitive to all of these concerns in helping her make her decision, keeping up to date on the possible new treatments, and carefully choosing which information to disclose in striving to be neutral. There are no easy answers to the many questions that will arise in this space, but better to start thinking about them now, before it is too late.