Small changes in how a person talks could reveal Alzheimer’s earlier

In an initial study, Canary analyzed speech recordings with AI and identified early stage Alzheimer’s with 96 percent accuracy.
Dave Arnold retired in his 60s and began spending time volunteering in local schools. But then he started misplacing items, forgetting appointments and losing his sense of direction. Eventually he was diagnosed with early stage Alzheimer’s.
“Hearing the diagnosis made me very emotional and tearful,” he said. “I immediately thought of all my mom had experienced.” His mother suffered with the condition for years before passing away. Over the last year, Arnold has worked for the Alzheimer’s Association as one of its early stage advisors, sharing his insights to help others in the initial stages of the disease.
Arnold was diagnosed sooner than many others. It's important to find out early, when interventions can make the most difference. One promising avenue is looking at how people talk. Research has shown that Alzheimer’s affects a part of the brain that controls speech, resulting in small changes before people show other signs of the disease.
Now, Canary Speech, a company based in Utah, is using AI to examine elements like the pitch of a person’s voice and their pauses. In an initial study, Canary analyzed speech recordings with AI and identified early stage Alzheimer’s with 96 percent accuracy.
Developing the AI model
Canary Speech’s CEO, Henry O’Connell, met cofounder Jeff Adams about 40 years before they started the company. Back when they first crossed paths, they were both living in Bethesda, Maryland; O’Connell was a research fellow at the National Institutes of Health studying rare neurological diseases, while Adams was working to decode spy messages. Later on, Adams would specialize in building mathematical models to analyze speech and sound as a team leader in developing Amazon's Alexa.
It wasn't until 2015 that they decided to make use of the fit between their backgrounds. ““We established Canary Speech in 2017 to build a product that could be used in multiple languages in clinical environments,” O'Connell says.
The need is growing. About 55 million people worldwide currently live with Alzheimer’s, a number that is expected to double by 2050. Some scientists think the disease results from a buildup of plaque in the brain. It causes mild memory loss at first and, over time, this issue get worse while other symptoms, such as disorientation and hallucinations, can develop. Treatment to manage the disease is more effective in the earlier stages, but detection is difficult since mild symptoms are often attributed to the normal aging process.
O’Connell and Adams specialize in the complex ways that Alzheimer’s effects how people speak. Using AI, their mathematical model analyzes 15 million data points every minute, focusing on certain features of speech such as pitch, pauses and elongation of words. It also pays attention to how the vibrations of vocal cords change in different stages of the disease.
To create their model, the team used a type of machine learning called deep neural nets, which looks at multiple layers of data - in this case, the multiple features of a person’s speech patterns.
“Deep neural nets allow us to look at much, much larger data sets built out of millions of elements,” O’Connell explained. “Through machine learning and AI, we’ve identified features that are very sensitive to an Alzheimer’s patient versus [people without the disease] and also very sensitive to mild cognitive impairment, early stage and moderate Alzheimer's.” Based on their learnings, Canary is able to classify the disease stage very quickly, O’Connell said.
“When we’re listening to sublanguage elements, we’re really analyzing the direct result of changes in the brain in the physical body,” O’Connell said. “The brain controls your vocal cords: how fast they vibrate, the expansion of them, the contraction.” These factors, along with where people put their tongues when talking, function subconsciously and result in subtle changes in the sounds of speech.
Further testing is needed
In an initial trial, Canary analyzed speech recordings from phone calls to a large U.S. health insurer. They looked at the audio recordings of 651 policyholders who had early stage Alzheimer’s and 1018 who did not have the condition, aiming for a representative sample of age, gender and race. They used this data to create their first diagnostic model and found that it was 96 percent accurate in identifying Alzheimer’s.
Christian Herff, an assistant professor of neuroscience at Maastricht University in the Netherlands, praised this approach while adding that further testing is needed to assess its effectiveness.
“I think the general idea of identifying increased risk for cognitive impairment based on speech characteristics is very feasible, particularly when change in a user’s voice is monitored, for example, by recording speech every year,” Herff said. He noted that this can only be a first indication, not a full diagnosis. The accuracy still needs to be validated in studies that follows individuals over a period of time, he said.
Toby Walsh, a professor of artificial intelligence at the University of New South Wales, also thinks Canary’s tool has potential but highlights that Canary could diagnose some people who don’t really have the disease. “This is an interesting and promising application of AI,” he said, “but these tools need to be used carefully. Imagine the anxiety of being misdiagnosed with Alzheimer’s.”
As with many other AI tools, privacy and bias are additional issues to monitor closely, Walsh said.
Other languages
A related issue is that not everyone is fluent in English. Mahnaz Arvaneh, a senior lecturer in automatic control and systems engineering at the University of Sheffield, said this could be a blind spot.
“The system may not be very accurate for those who have English as their second language as their speaking patterns would be different, and any issue might be because of language deficiency rather than cognitive issues,” Arvaneh said.
The team is expanding to multiple languages starting with Japanese and Spanish. The elements of the model that make up the algorithm are very similar, but they need to be validated and retrained in a different language, which will require access to more data.
Recently, Canary analyzed the phone calls of 233 Japanese patients who had mild cognitive impairment and 704 healthy people. Using an English model they were able to identify the Japanese patients who had mild cognitive impairment with 78 percent accuracy. They also developed a model in Japanese that was 45 percent accurate, and they’re continuing to train it with more data.
The future
Canary is using their model to look at other diseases like Huntington’s and Parkinson’s. They’re also collaborating with pharmaceuticals to validate potential therapies for Alzheimer’s. By looking at speech patterns over time, Canary can get an indication of how well these drugs are working.

Dave Arnold and his wife dance at his nephew’s wedding in Rochester, New York, ten years ago, before his Alzheimer's diagnosis.
Dave Arnold
Ultimately, they want to integrate their tool into everyday life. “We want it to be used in a smartphone, or a teleconference call so that individuals could be examined in their home,” O’Connell said. “We could follow them over time and work with clinical teams and hospitals to improve the evaluation of patients and contribute towards an accurate diagnosis.”
Arnold, the patient with early stage Alzheimer’s, sees great promise. “The process of getting a diagnosis is already filled with so much anxiety,” he said. “Anything that can be done to make it easier and less stressful would be a good thing, as long as it’s proven accurate.”
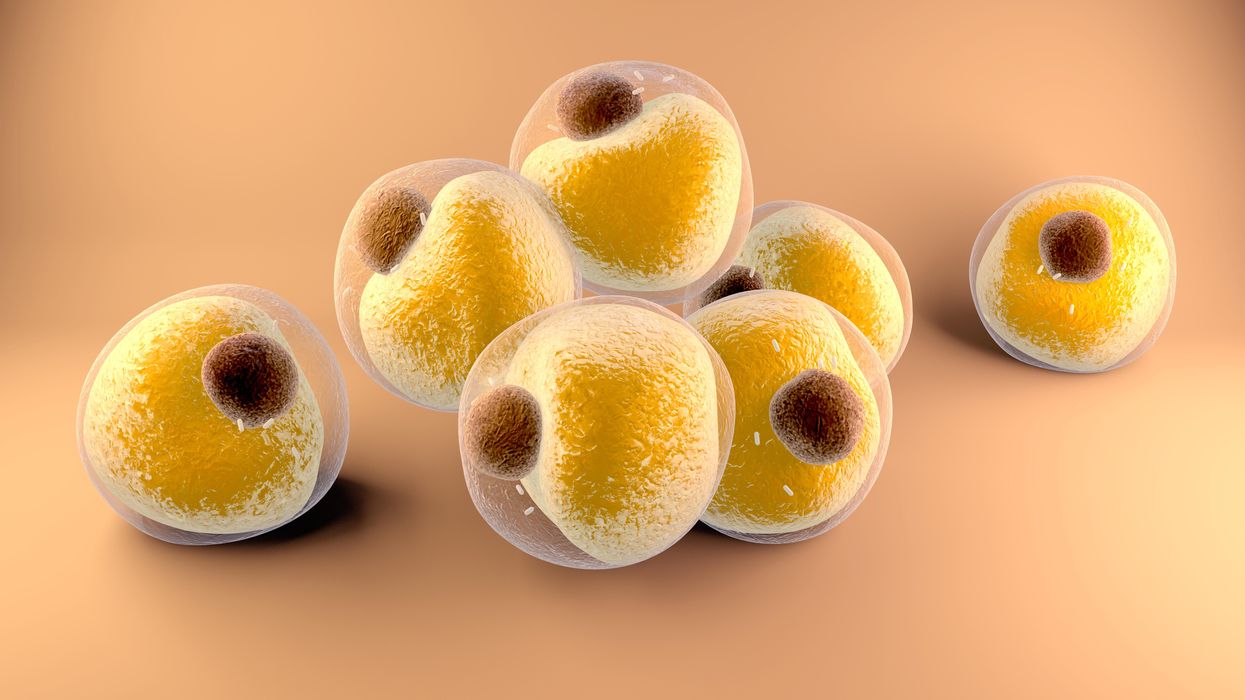
Researchers at Stanford have found that the virus that causes Covid-19 can infect fat cells, which could help explain why obesity is linked to worse outcomes for those who catch Covid-19.
Obesity is a risk factor for worse outcomes for a variety of medical conditions ranging from cancer to Covid-19. Most experts attribute it simply to underlying low-grade inflammation and added weight that make breathing more difficult.
Now researchers have found a more direct reason: SARS-CoV-2, the virus that causes Covid-19, can infect adipocytes, more commonly known as fat cells, and macrophages, immune cells that are part of the broader matrix of cells that support fat tissue. Stanford University researchers Catherine Blish and Tracey McLaughlin are senior authors of the study.
Most of us think of fat as the spare tire that can accumulate around the middle as we age, but fat also is present closer to most internal organs. McLaughlin's research has focused on epicardial fat, “which sits right on top of the heart with no physical barrier at all,” she says. So if that fat got infected and inflamed, it might directly affect the heart.” That could help explain cardiovascular problems associated with Covid-19 infections.
Looking at tissue taken from autopsy, there was evidence of SARS-CoV-2 virus inside the fat cells as well as surrounding inflammation. In fat cells and immune cells harvested from health humans, infection in the laboratory drove "an inflammatory response, particularly in the macrophages…They secreted proteins that are typically seen in a cytokine storm” where the immune response runs amok with potential life-threatening consequences. This suggests to McLaughlin “that there could be a regional and even a systemic inflammatory response following infection in fat.”
It is easy to see how the airborne SARS-CoV-2 virus infects the nose and lungs, but how does it get into fat tissue? That is a mystery and the source of ample speculation.
The macrophages studied by McLaughlin and Blish were spewing out inflammatory proteins, While the the virus within them was replicating, the new viral particles were not able to replicate within those cells. It was a different story in the fat cells. “When [the virus] gets into the fat cells, it not only replicates, it's a productive infection, which means the resulting viral particles can infect another cell,” including microphages, McLaughlin explains. It seems to be a symbiotic tango of the virus between the two cell types that keeps the cycle going.
It is easy to see how the airborne SARS-CoV-2 virus infects the nose and lungs, but how does it get into fat tissue? That is a mystery and the source of ample speculation.
Macrophages are mobile; they engulf and carry invading pathogens to lymphoid tissue in the lymph nodes, tonsils and elsewhere in the body to alert T cells of the immune system to the pathogen. Perhaps some of them also carry the virus through the bloodstream to more distant tissue.
ACE2 receptors are the means by which SARS-CoV-2 latches on to and enters most cells. They are not thought to be common on fat cells, so initially most researchers thought it unlikely they would become infected.
However, while some cell receptors always sit on the surface of the cell, other receptors are expressed on the surface only under certain conditions. Philipp Scherer, a professor of internal medicine and director of the Touchstone Diabetes Center at the University of Texas Southwestern Medical Center, suggests that, in people who have obesity, “There might be higher levels of dysfunctional [fat cells] that facilitate entry of the virus,” either through transiently expressed ACE2 or other receptors. Inflammatory proteins generated by macrophages might contribute to this process.
Another hypothesis is that viral RNA might be smuggled into fat cells as cargo in small bits of material called extracellular vesicles, or EVs, that can travel between cells. Other researchers have shown that when EVs express ACE2 receptors, they can act as decoys for SARS-CoV-2, where the virus binds to them rather than a cell. These scientists are working to create drugs that mimic this decoy effect as an approach to therapy.
Do fat cells play a role in Long Covid? “Fat cells are a great place to hide. You have all the energy you need and fat cells turn over very slowly; they have a half-life of ten years,” says Scherer. Observational studies suggest that acute Covid-19 can trigger the onset of diabetes especially in people who are overweight, and that patients taking medicines to regulate their diabetes “were actually quite protective” against acute Covid-19. Scherer has funding to study the risks and benefits of those drugs in animal models of Long Covid.
McLaughlin says there are two areas of potential concern with fat tissue and Long Covid. One is that this tissue might serve as a “big reservoir where the virus continues to replicate and is sent out” to other parts of the body. The second is that inflammation due to infected fat cells and macrophages can result in fibrosis or scar tissue forming around organs, inhibiting their function. Once scar tissue forms, the tissue damage becomes more difficult to repair.
Current Covid-19 treatments work by stopping the virus from entering cells through the ACE2 receptor, so they likely would have no effect on virus that uses a different mechanism. That means another approach will have to be developed to complement the treatments we already have. So the best advice McLaughlin can offer today is to keep current on vaccinations and boosters and lose weight to reduce the risk associated with obesity.
Air pollution can lead to lung cancer. The connection suggests new ways to stop cancer in its tracks.
Researchers at Francis Crick Institute found that air pollution can "wake up" existing mutations, triggering them to turn into lung cancer. The scientists used their new understanding about this connection to prevent cancer in mice.
Forget taking a deep breath. Around the world, 99 percent of people breathe air polluted to unsafe levels, according to data from the World Health Organization. Activities such as burning fossil fuels release greenhouse gases that contribute to air pollution, which could lead to heart disease, stroke, asthma, emphysema, and some types of cancer.
“The burden of disease attributable to air pollution is now estimated to be on a par with other major global health risks such as unhealthy diet and tobacco smoking, and air pollution is now recognized as the single biggest environmental threat to human health,” wrote the authors of a 2021 WHO report.
The majority of lung cancer is attributed to smoking. But as pollution levels have increased, and anti-smoking campaigns have discouraged smoking, the proportion of lung cancers diagnosed in non-smokers has grown. The CDC estimates that 10 to 20 percent of lung cancers in the U.S. currently occur in non-smokers.
The mechanism between air pollution and the development of lung cancer has been unclear, but researchers at London’s Francis Crick Institute recently made an important breakthrough in understanding the connection. Lead investigator Charles Swanton presented this research last month at a conference in Paris.
Pollution awakens mutations
The Crick Institute scientists were able to identify a new link between common air pollutants and non-small cell lung cancer (NSCLC). They focused on pollutants called particulate matter, or PM, that are 2.5 microns wide, narrower than human cells.
Most cancer diagnosed in non-smoking people is NSCLC, but this type of cancer hasn’t received the same research attention as more common lung cancers found in smokers, according to Clare Weeden, a cancer researcher at the Crick Institute and a co-author of the study.
“This is a really underserved and under-researched population that we really need to tackle, as well as lung cancers that occur in smokers,” she says. “Lung cancer is the number one cancer killer worldwide.”
In the past, some researchers believed air pollution caused mutations that led to cancer. Others believed these mutations could remain dormant without any detriment to health until pollutants or other stressors triggered them to become cancerous. Reviving the latter hypothesis that carcinogens may activate pre-existing mutations, instead of directly causing them, the Crick researchers analyzed samples from 463,679 people in the UK and parts of Asia, noting mutations and comparing changes in gene expression in mice and human cells.
“The mutation can exist in a nascent clone without causing cancer,” says Emilia Lim, a bioinformatics expert and a co-first author of the Crick study. “It is the carcinogen that promotes a conducive environment for this one little clone to grow and expand into cancer. Through our work, we were able to revive excitement for this hypothesis and bring it to light.”
The study explains a confusing pattern of lung cancer developing, particularly in women, despite a lack of environmental risk factors like smoking, secondhand smoke, or radon exposure. The culprit in these cases may have been too much PM 2.5 exposure.
Other researchers had previously identified a link between mutations in certain genes that control epidermal growth factor receptors, or EGFR mutations, and the development of NSCLC. In a 2019 study of 250 people with this type of cancer, about 32 percent had the mutation. Women are more likely to have EGFR mutations than men.
Not everyone who has the EGFR mutation will develop lung cancer. Respirologist Stephen Lam studies lung cancer at the BC Cancer Research Centre in Vancouver, Canada, but was not involved in the Crick Institute research. He says the study explains a confusing pattern of lung cancer developing, particularly in women, despite a lack of environmental risk factors like smoking, secondhand smoke, or radon exposure. The culprit in these cases may have been too much PM 2.5 exposure.
More exposure leads to inflammation and lesions
The Crick researchers found that an excess of PM 2.5 in the air sparked an inflammatory process in cells within the lung. This inflammation set the stage for NSCLC to develop in people and mice with existing EGFR mutations.
The researchers also exposed mice without EGFR mutations to PM 2.5 pollution—an experiment that couldn’t be ethically conducted in humans—to link pollution exposure to NSCLC. The mice experiments also showed that NSCLC is dose-dependent; higher levels of exposure were associated with higher number of cancerous lesions forming.
Ultimately, the study “fundamentally changed how we view lung cancer in people who have never smoked,” said Swanton in a Crick Institute press release. “Cells with cancer-causing mutations accumulate naturally as we age, but they are normally inactive. We’ve demonstrated that air pollution wakes these cells up in the lungs, encouraging them to grow and potentially form tumors.”
Preventing cancer before it begins
Targeted therapies already exist for people with EGFR mutations who’ve developed NSCLC, but they have many side effects, according to Weeden. Researchers hope that making more definitive links between pollutants and cancer could help prevent people with EGFR or other mutations from developing lung cancer in the first place.
Along those lines, as an additional component of their study presented last month, the Crick researchers were able to prevent cancer in mice that had the EGFR mutations by blocking inflammation. They used an antibody to inhibit a protein called interleukin 1 beta, which plays a key role in inflammation. Scientists could eventually use such antibodies or other therapies to make a drug treatment that people can take to stop cancer in its tracks, even if they live in highly polluted areas.
Such potential could reach beyond lung cancer; in the past, Crick and other researchers have also found associations between exposure to air pollution and mesothelioma, as well as cancers of the small intestine, lip, mouth, and throat. These links could be meaningful to a growing number of people as climate change intensifies, and with increases in air pollution from fossil fuel combustion and natural disasters like forest fires.
Plus, air pollution is just one external condition that can flip the switch of these inflammatory pathways. Identifying a link between pollution and cancer “has wide ramifications for many other environmental factors that may [play] similar roles,” Weedon says. She hopes that the Crick study and future research in this area will offer some hope for non-smokers frustrated by cancer diagnoses.