What to Know about the Fast-Spreading Delta Variant
A highly contagious form of the coronavirus known as the Delta variant is spreading rapidly and becoming increasingly prevalent around the world. First identified in India in December, Delta has now been identified in 111 countries.
In the United States, the variant now accounts for 83% of sequenced COVID-19 cases, said Rochelle Walensky, director of the Centers for Disease Control and Prevention, at a July 20 Senate hearing. In May, Delta was responsible for just 3% of U.S. cases. The World Health Organization projects that Delta will become the dominant variant globally over the coming months.
So, how worried should you be about the Delta variant? We asked experts some common questions about Delta.
What is a variant?
To understand Delta, it's helpful to first understand what a variant is. When a virus infects a person, it gets into your cells and makes a copy of its genome so it can replicate and spread throughout your body.
In the process of making new copies of itself, the virus can make a mistake in its genetic code. Because viruses are replicating all the time, these mistakes — also called mutations — happen pretty often. A new variant emerges when a virus acquires one or more new mutations and starts spreading within a population.
There are thousands of SARS-CoV-2 variants, but most of them don't substantially change the way the virus behaves. The variants that scientists are most interested in are known as variants of concern. These are versions of the virus with mutations that allow the virus to spread more easily, evade vaccines, or cause more severe disease.
"The vast majority of the mutations that have accumulated in SARS-CoV-2 don't change the biology as far as we're concerned," said Jennifer Surtees, a biochemist at the University of Buffalo who's studying the coronavirus. "But there have been a handful of key mutations and combinations of mutations that have led to what we're now calling variants of concern."
One of those variants of concern is Delta, which is now driving many new COVID-19 infections.
Why is the Delta variant so concerning?
"The reason why the Delta variant is concerning is because it's causing an increase in transmission," said Alba Grifoni, an infectious disease researcher at the La Jolla Institute for Immunology. "The virus is spreading faster and people — particularly those who are not vaccinated yet — are more prone to exposure."
The Delta variant has a few key mutations that make it better at attaching to our cells and evading the neutralizing antibodies in our immune system. These mutations have changed the virus enough to make it more than twice as contagious as the original SARS-CoV-2 virus that emerged in Wuhan and about 50% more contagious than the Alpha variant, previously known as B.1.1.7, or the U.K. variant.
These mutations were previously seen in other variants on their own, but it's their combination that makes Delta so much more infectious.
Do vaccines work against the Delta variant?
The good news is, the COVID-19 vaccines made by AstraZeneca, Johnson & Johnson, Moderna, and Pfizer still work against the Delta variant. They remain more than 90% effective at preventing hospitalizations and death due to Delta. While they're slightly less protective against disease symptoms, they're still very effective at preventing severe illness caused by the Delta variant.
"They're not as good as they were against the prior strains, but they're holding up pretty well," said Eric Topol, a physician and director of the Scripps Translational Research Institute, during a July 19 briefing for journalists.
Because Delta is better at evading our immune systems, it's likely causing more breakthrough infections — COVID-19 cases in people who are vaccinated. However, breakthrough infections were expected before the Delta variant became widespread. No vaccine is 100% effective, so breakthrough infections can happen with other vaccines as well. Experts say the COVID-19 vaccines are still working as expected, even if breakthrough infections occur. The majority of these infections are asymptomatic or cause only mild symptoms.
Should vaccinated people worry about the Delta variant?
Vaccines train our immune systems to protect us against infection. They do this by spurring the production of antibodies, which stick around in our bodies to help fight off a particular pathogen in case we ever come into contact with it.
But even if the new Delta variant slips past our neutralizing antibodies, there's another component of our immune system that can help overtake the virus: T cells. Studies are showing that the COVID-19 vaccines also galvanize T cells, which help limit disease severity in people who have been vaccinated.
"While antibodies block the virus and prevent the virus from infecting cells, T cells are able to attack cells that have already been infected," Grifoni said. In other words, T cells can prevent the infection from spreading to more places in the body. A study published July 1 by Grifoni and her colleagues found that T cells were still able to recognize mutated forms of the virus — further evidence that our current vaccines are effective against Delta.
Can fully vaccinated people spread the Delta variant?
Previously, scientists believed it was unlikely for fully vaccinated individuals with asymptomatic infections to spread Covid-19. But the Delta variant causes the virus to make so many more copies of itself inside the body, and high viral loads have been found in the respiratory tracts of people who are fully vaccinated. This suggests that vaccinated people may be able to spread the Delta variant to some degree.
If you have COVID-19 symptoms, even if you're fully vaccinated, you should get tested and isolate from friends and family because you could spread the virus.
What risk does Delta pose to unvaccinated people?
The Delta variant is behind a surge in cases in communities with low vaccination rates, and unvaccinated Americans currently account for 97% of hospitalizations due to COVID-19, according to Walensky. The best thing you can do right now to prevent yourself from getting sick is to get vaccinated.
Gigi Gronvall, an immunologist and senior scholar at the Johns Hopkins Center for Health Security, said in this week's "Making Sense of Science" podcast that it's especially important to get all required doses of the vaccine in order to have the best protection against the Delta variant. "Even if it's been more than the allotted time that you were told to come back and get the second, there's no time like the present," she said.
With more than 3.6 billion COVID-19 doses administered globally, the vaccines have been shown to be incredibly safe. Serious adverse effects are rare, although scientists continue to monitor for them.
Being vaccinated also helps prevent the emergence of new and potentially more dangerous variants. Viruses need to infect people in order to replicate, and variants emerge because the virus continues to infect more people. More infections create more opportunities for the virus to acquire new mutations.
Surtees and others worry about a scenario in which a new variant emerges that's even more transmissible or resistant to vaccines. "This is our window of opportunity to try to get as many people vaccinated as possible and get people protected so that so that the virus doesn't evolve to be even better at infecting people," she said.
Does Delta cause more severe disease?
While hospitalizations and deaths from COVID-19 are increasing again, it's not yet clear whether Delta causes more severe illness than previous strains.
How can we protect unvaccinated children from the Delta variant?
With children 12 and under not yet eligible for the COVID-19 vaccine, kids are especially vulnerable to the Delta variant. One way to protect unvaccinated children is for parents and other close family members to get vaccinated.
It's also a good idea to keep masks handy when going out in public places. Due to risk Delta poses, the American Academy of Pediatrics issued new guidelines July 19 recommending that all staff and students over age 2 wear face masks in school this fall, even if they have been vaccinated.
Parents should also avoid taking their unvaccinated children to crowded, indoor locations and make sure their kids are practicing good hand-washing hygiene. For children younger than 2, limit visits with friends and family members who are unvaccinated or whose vaccination status is unknown and keep up social distancing practices while in public.
While there's no evidence yet that Delta increases disease severity in children, parents should be mindful that in some rare cases, kids can get a severe form of the disease.
"We're seeing more children getting sick and we're seeing some of them get very sick," Surtees said. "Those children can then pass on the virus to other individuals, including people who are immunocompromised or unvaccinated."
No, the New COVID Vaccine Is Not "Morally Compromised"
As the proportion of vaccinated elderly people increases, family reunions become possible again -- but not if people reject the vaccines on religious grounds.
The approval of the Johnson & Johnson COVID-19 vaccine has been heralded as a major advance. A single-dose vaccine that is highly efficacious at removing the ability of the virus to cause severe disease, hospitalization, and death (even in the face of variants) is nothing less than pathbreaking. Anyone who is offered this vaccine should take it. However, one group advises its adherents to preferentially request the Moderna or Pfizer vaccines instead in the quest for morally "irreproachable" vaccines.
Is this group concerned about lower numerical efficacy in clinical trials? No, it seems that they have deemed the J&J vaccine "morally compromised". The group is the U.S. Conference of Catholic Bishops and if something is "morally compromised" it is surely not the vaccine. (Notably Pope Francis has not taken such a stance).
At issue is a cell line used to manufacture the vaccine. Specifically, a cell line used to grow the adenovirus vector used in the vaccine. The purpose of the vector is to carry a genetic snippet of the coronavirus spike protein into the body, like a Trojan Horse ferrying in an enemy combatant, in order to safely trigger an immune response without any chance of causing COVID-19 itself.
It is my hope that the country's 50 million Catholics do not heed the U.S. Conference of Bishops' potentially deadly advice and instead obtain whichever vaccine is available to them as soon as possible.
The cell line of the vector, known as PER.C6, was derived from a fetus that was aborted in 1985. This cell line is prolific in biotechnology, as are other fetal-derived cell lines such as HEK-293 (human embryonic kidney), used in the manufacture of the Astra Zeneca COVID-19 vaccine. Indeed, fetal cell lines are used in the manufacture of critical vaccines directed against pathogens such as hepatitis A, rubella, rabies, chickenpox, and shingles and were used to test the Moderna and Pfizer COVID-19 vaccines (which, accordingly, the U.S. Conference of Bishops deem to only raise moral "concerns").
As such, fetal cell lines from abortions are a common and critical component of biotechnology that we all rely on to improve our health. Such cell lines have been used to help find treatments for cancer, Ebola, and many other diseases.
Dr. Andrea Gambotto, a vaccine scientist at the University of Pittsburgh School of Medicine, explained to Science magazine last year why fetal cells are so important to vaccine development: "Cultured [nonhuman] animal cells can produce the same proteins, but they would be decorated with different sugar molecules, which—in the case of vaccines—runs the risk of failing to evoke a robust and specific immune response." Thus, the fetal cells' human origins are key to their effectiveness.
So why the opposition to this life-saving technology, especially in the midst of the deadliest pandemic in over a century? How could such a technology be "morally compromised" when morality, as I understand it, is a code of values to guide human life on Earth with the purpose of enhancing well-being?
By any measure, the J&J vaccine accomplishes that, since human life, not embryonic or fetal life, is the standard of value. An embryo or fetus in the earlier stages of development, while harboring the potential to grow into a human being, is not the moral equivalent of a person. Thus, creating life-saving medical technology using cells that would have otherwise been destroyed is not in conflict with a proper moral code. To me, it is nihilistic to oppose these vaccines on the grounds cited by the U.S. Conference of Bishops.
Reason, the rational faculty, is the human means of knowledge. It is what one should wield when approaching a scientific or health issue. Appeals from clerics, devoid of any need to tether their principles to this world, should not have any bearing on one's medical decision-making.
In the Dark Ages, the Catholic Church opposed all forms of scientific inquiry, even castigating science and curiosity as the "lust of the eyes": One early Middle Ages church father reveled in his rejection of reality and evidence, proudly declaring, "I believe because it is absurd." This organization, which tyrannized scientists such as Galileo and murdered the Italian cosmologist Bruno, today has shown itself to still harbor anti-science sentiments in its ranks.
It is my hope that the country's 50 million Catholics do not heed the U.S. Conference of Bishops' potentially deadly advice and instead obtain whichever vaccine is available to them as soon as possible. When judged using the correct standard of value, vaccines using fetal cell lines in their development are an unequivocal good -- while those who attempt to undermine them deserve a different category altogether.
Dr. Adalja is focused on emerging infectious disease, pandemic preparedness, and biosecurity. He has served on US government panels tasked with developing guidelines for the treatment of plague, botulism, and anthrax in mass casualty settings and the system of care for infectious disease emergencies, and as an external advisor to the New York City Health and Hospital Emergency Management Highly Infectious Disease training program, as well as on a FEMA working group on nuclear disaster recovery. Dr. Adalja is an Associate Editor of the journal Health Security. He was a coeditor of the volume Global Catastrophic Biological Risks, a contributing author for the Handbook of Bioterrorism and Disaster Medicine, the Emergency Medicine CorePendium, Clinical Microbiology Made Ridiculously Simple, UpToDate's section on biological terrorism, and a NATO volume on bioterrorism. He has also published in such journals as the New England Journal of Medicine, the Journal of Infectious Diseases, Clinical Infectious Diseases, Emerging Infectious Diseases, and the Annals of Emergency Medicine. He is a board-certified physician in internal medicine, emergency medicine, infectious diseases, and critical care medicine. Follow him on Twitter: @AmeshAA
Donna Shirley pictured at her home in Tulsa, with a model of the Sojourner rover she was in charge of that explored Mars.
When NASA's Perseverance rover landed successfully on Mars on February 18, 2021, calling it "one giant leap for mankind" – as Neil Armstrong said when he set foot on the moon in 1969 – would have been inaccurate. This year actually marked the fifth time the U.S. space agency has put a remote-controlled robotic exploration vehicle on the Red Planet. And it was a female engineer named Donna Shirley who broke new ground for women in science as the manager of both the Mars Exploration Program and the 30-person team that built Sojourner, the first rover to land on Mars on July 4, 1997.
For Shirley, the Mars Pathfinder mission was the climax of her 32-year career at NASA's Jet Propulsion Laboratory (JPL) in Pasadena, California. The Oklahoma-born scientist, who earned her Master's degree in aerospace engineering from the University of Southern California, saw her profile skyrocket with media appearances from CNN to the New York Times, and her autobiography Managing Martians came out in 1998. Now 79 and living in a Tulsa retirement community, she still embraces her status as a female pioneer.
"Periodically, I'll hear somebody say they got into the space program because of me, and that makes me feel really good," Shirley told Leaps.org. "I look at the mission control area, and there are a lot of women in there. I'm quite pleased I was able to break the glass ceiling."
Her $25-million, 25-pound microrover – powered by solar energy and designed to get rock samples and test soil chemistry for evidence of life – was named after Sojourner Truth, a 19th-century Black abolitionist and women's rights activist. Unlike Mars Pathfinder, Shirley didn't have to travel more than 131 million miles to reach her goal, but her path to scientific fame as a woman sometimes resembled an asteroid field.
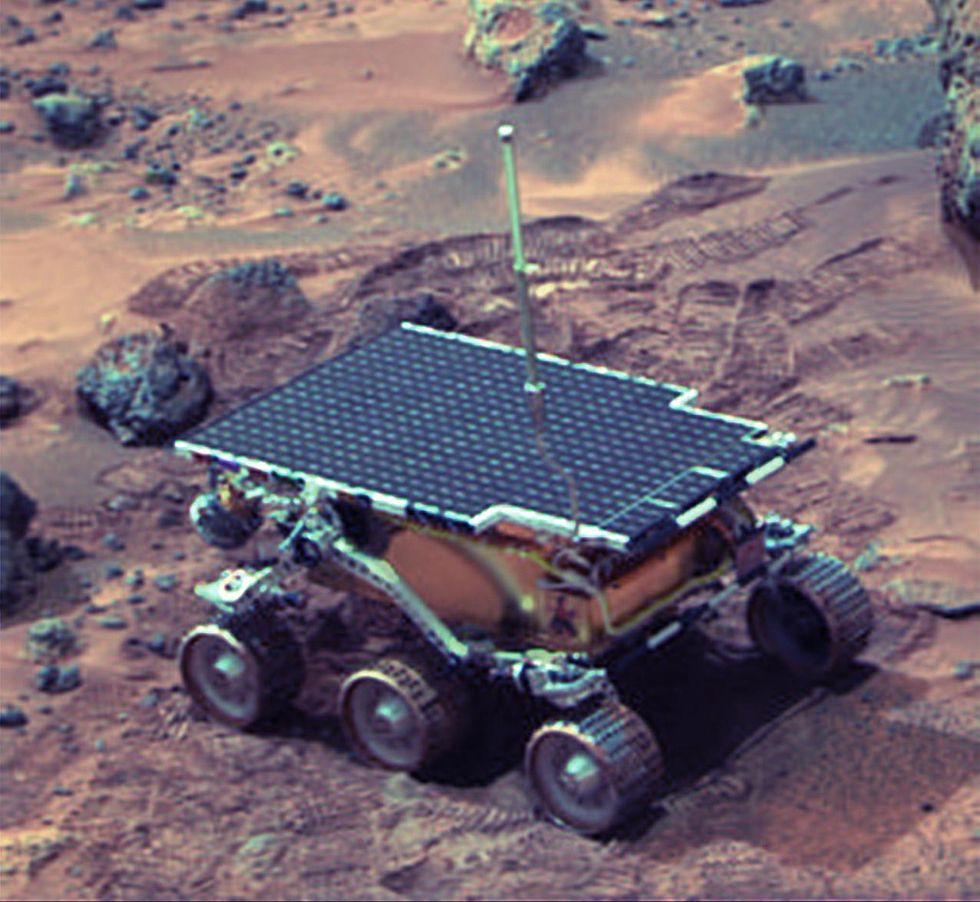 The Sojourner Rover in 1997 on Mars.NASA/JPL
The Sojourner Rover in 1997 on Mars.NASA/JPLAs a high-IQ tomboy growing up in Wynnewood, Oklahoma (pop. 2,300), Shirley yearned to escape. She decided to become an engineer at age 10 and took flying lessons at 15. Her extraterrestrial aspirations were fueled by Ray Bradbury's The Martian Chronicles and Arthur C. Clarke's The Sands of Mars. Yet when she entered the University of Oklahoma (OU) in 1958, her freshman academic advisor initially told her: "Girls can't be engineers." She ignored him.
Years later, Shirley would combat such archaic thinking, succeeding at JPL with her creative, collaborative management style. "If you look at the literature, you'll find that teams that are either led by or heavily involved with women do better than strictly male teams," she noted.
However, her career trajectory stalled at OU. Burned out by her course load and distracted by a broken engagement to marry a fellow student, she switched her major to professional writing. After graduation, she applied her aeronautical background as a McDonnell Aircraft technical writer, but her boss, she says, harassed her and she faced gender-based hostility from male co-workers.
Returning to OU, Shirley finished off her engineering degree and became a JPL aerodynamist in 1966 after answering an ad in the St. Louis Post-Dispatch. At first, she was the only female engineer among the research center's 2,000-odd engineers. She wore many hats, from designing planetary atmospheric entry vehicles to picking the launch date of November 4, 1973 for Mariner 10's mission to Venus and Mercury.
By the mid-1980's, she was managing teams that focused on robotics and Mars, delivering creative solutions when NASA budget cuts loomed. In 1989, the same year the Sojourner microrover concept was born, President George H.W. Bush announced his Space Exploration Initiative, including plans for a human mission to Mars by 2019.
That target, of course, wasn't attained, despite huge advances in technology and our understanding of the Martian environment. Today, Shirley believes humans could land on Mars by 2030. She became the founding director of the Science Fiction Museum and Hall of Fame in Seattle in 2004 after leaving NASA, and to this day, she enjoys checking out pop culture portrayals of Mars landings – even if they're not always accurate.
After the novel The Martian was published in 2011, which later was adapted into the hit film starring Matt Damon, Shirley phoned author Andy Weir: "You've got a major mistake in here. It says there's a storm that tries to blow the rocket over. But actually, the Mars atmosphere is so thin, it would never blow a rocket over!"
Fearlessly speaking her mind and seeking the stars helped Donna Shirley make history. However, a 2019 Washington Post story noted: "Women make up only about a third of NASA's workforce. They comprise just 28 percent of senior executive leadership positions and are only 16 percent of senior scientific employees." Whether it's traveling to Mars or trending toward gender equality, we've still got a long way to go.

