Your Community and COVID-19: How to Make Sense of the Numbers Where You Live
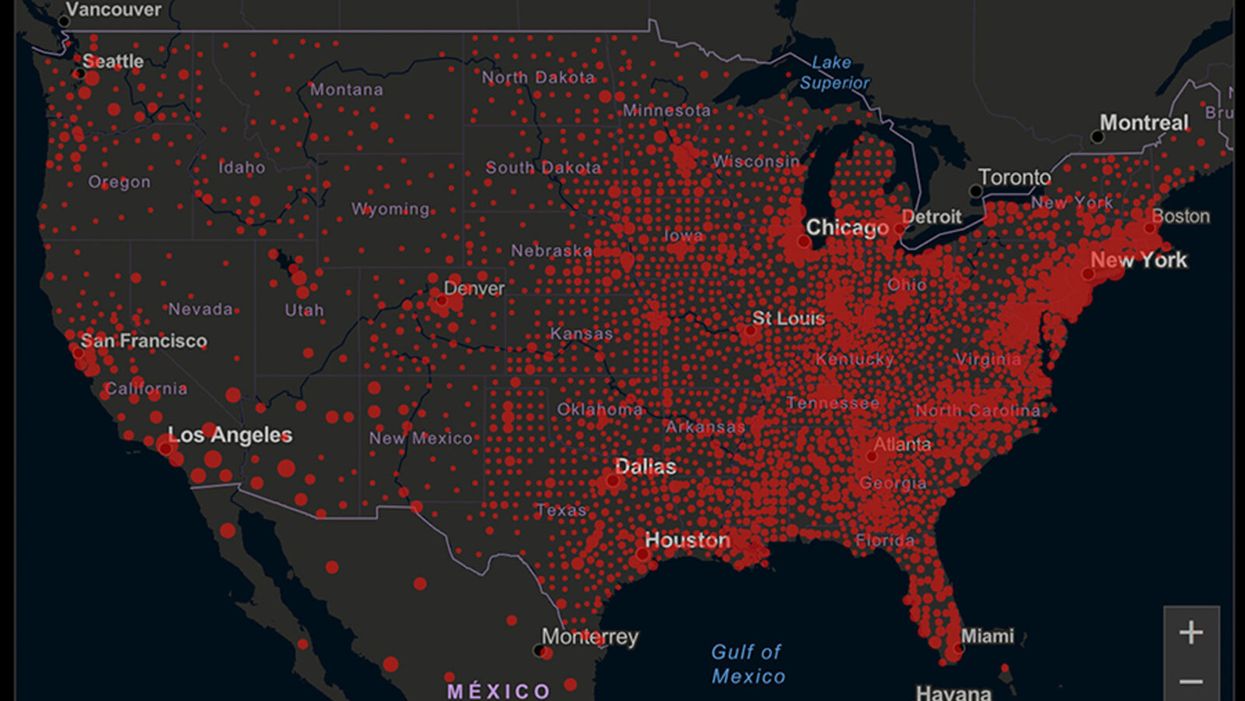
A map of cumulative known cases of COVID-19 in the U.S., as of June 12th, 2020.
Have you felt a bit like an armchair epidemiologist lately? Maybe you've been poring over coronavirus statistics on your county health department's website or on the pages of your local newspaper.
If the percentage of positive tests steadily stays under 8 percent, that's generally a good sign.
You're likely to find numbers and charts but little guidance about how to interpret them, let alone use them to make day-to-day decisions about pandemic safety precautions.
Enter the gurus. We asked several experts to provide guidance for laypeople about how to navigate the numbers. Here's a look at several common COVID-19 statistics along with tips about how to understand them.
Case Counts: Consider the Context
The number of confirmed COVID-19 cases in American counties is widely available. Local and state health departments should provide them online, or you can easily look them up at The New York Times' coronavirus database. However, you need to be cautious about interpreting them.
"Case counts are the obvious numbers to look at. But they're probably the hardest thing to sort out," said Dr. Jeff Martin, an epidemiologist at the University of California at San Francisco.
That's because case counts by themselves aren't a good window into how the coronavirus is affecting your community since they rely on testing. And testing itself varies widely from day to day and community to community.
"The more testing that's done, the more infections you'll pick up," explained Dr. F. Perry Wilson, a physician at Yale University. The numbers can also be thrown off when tests are limited to certain groups of people.
"If the tests are being mostly given to people with a high probability of having been infected -- for example, they have had symptoms or work in a high-risk setting -- then we expect lots of the tests to be positive. But that doesn't tell us what proportion of the general public is likely to have been infected," said Eleanor Murray, an epidemiologist at Boston University.
These Stats Are More Meaningful
According to Dr. Wilson, it's more useful to keep two other statistics in mind: the number of COVID tests that are being performed in your community and the percentage that turn up positive, showing that people have the disease. (These numbers may or may not be available locally. Check the websites of your community's health department and local news media outlets.)
If the number of people being tested is going up, but the percentage of positive tests is going down, Dr. Wilson said, that's a good sign. But if both numbers are going up – the number of people tested and the percentage of positive results – then "that's a sign that there are more infections burning in the community."
It's especially worrisome if the percentage of positive cases is growing compared to previous days or weeks, he said. According to him, that's a warning of a "high-risk situation."
Dr. George Rutherford, an epidemiologist at University of California at San Francisco, offered this tip: If the percentage of positive tests steadily stays under 8 percent, that's generally a good sign.
There's one more caveat about case counts. It takes an average of a week for someone to be infected with COVID-19, develop symptoms, and get tested, Dr. Rutherford said. It can take an additional several days for those test results to be reported to the county health department. This means that case numbers don't represent infections happening right now, but instead are a picture of the state of the pandemic more than a week ago.
Hospitalizations: Focus on Current Statistics
You should be able to find numbers about how many people in your community are currently hospitalized – or have been hospitalized – with diagnoses of COVID-19. But experts say these numbers aren't especially revealing unless you're able to see the number of new hospitalizations over time and track whether they're rising or falling. This number often isn't publicly available, however.
If new hospitalizations are increasing, "you may want to react by being more careful yourself."
And there's an important caveat: "The problem with hospitalizations is that they do lag," UC San Francisco's Dr. Martin said, since it takes time for someone to become ill enough to need to be hospitalized. "They tell you how much virus was being transmitted in your community 2 or 2.5 weeks ago."
Also, he said, people should be cautious about comparing new hospitalization rates between communities unless they're adjusted to account for the number of more-vulnerable older people.
Still, if new hospitalizations are increasing, he said, "you may want to react by being more careful yourself."
Deaths: They're an Even More Delayed Headline
Cable news networks obsessively track the number of coronavirus deaths nationwide, and death counts for every county in the country are available online. Local health departments and media websites may provide charts tracking the growth in deaths over time in your community.
But while death rates offer insight into the disease's horrific toll, they're not useful as an instant snapshot of the pandemic in your community because severely ill patients are typically sick for weeks. Instead, think of them as a delayed headline.
"These numbers don't tell you what's happening today. They tell you how much virus was being transmitted 3-4 weeks ago," Dr. Martin said.
'Reproduction Value': It May Be Revealing
You're not likely to find an available "reproduction value" for your community, but it is available for your state and may be useful.
A reproduction value, also known as R0 or R-naught, "tells us how many people on average we expect will be infected from a single case if we don't take any measures to intervene and if no one has been infected before," said Boston University's Murray.
As The New York Times explained, "R0 is messier than it might look. It is built on hard science, forensic investigation, complex mathematical models — and often a good deal of guesswork. It can vary radically from place to place and day to day, pushed up or down by local conditions and human behavior."
It may be impossible to find the R0 for your community. However, a website created by data specialists is providing updated estimates of a related number -- effective reproduction number, or Rt – for each state. (The R0 refers to how infectious the disease is in general and if precautions aren't taken. The Rt measures its infectiousness at a specific time – the "t" in Rt.) The site is at rt.live.
"The main thing to look at is whether the number is bigger than 1, meaning the outbreak is currently growing in your area, or smaller than 1, meaning the outbreak is currently decreasing in your area," Murray said. "It's also important to remember that this number depends on the prevention measures your community is taking. If the Rt is estimated to be 0.9 in your area and you are currently under lockdown, then to keep it below 1 you may need to remain under lockdown. Relaxing the lockdown could mean that Rt increases above 1 again."
"Whether they're on the upswing or downswing, no state is safe enough to ignore the precautions about mask wearing and social distancing."
Keep in mind that you can still become infected even if an outbreak in your community appears to be slowing. Low risk doesn't mean no risk.
Putting It All Together: Why the Numbers Matter
So you've reviewed COVID-19 statistics in your community. Now what?
Dr. Wilson suggests using the data to remind yourself that the coronavirus pandemic "is still out there. You need to take it seriously and continue precautions," he said. "Whether they're on the upswing or downswing, no state is safe enough to ignore the precautions about mask wearing and social distancing. 'My state is doing well, no one I know is sick, is it time to have a dinner party?' No."
He also recommends that laypeople avoid tracking COVID-19 statistics every day. "Check in once a week or twice a month to see how things are going," he suggested. "Don't stress too much. Just let it remind you to put that mask on before you get out of your car [and are around others]."
Scientists use AI to predict how hospital stays will go
In this week's Friday Five, research on the best time to wrap up eating for the night, how to use AI to predict how hospital stays will go, a new way to armor the shields of our livers against cancer, super neurons in super agers - and much more.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Here are the promising studies covered in this week's Friday Five:
- The problem with bedtime munching
- Scientists use AI to predict how stays in hospitals will go
- How to armor the shields of our livers against cancer
- One big step to save the world: turn one kind of plastic into another
- The perfect recipe for tiny brains
And an honorable mention this week: Bigger is better when it comes to super neurons in super agers
The Toxic Effects of Noise and What We’re Not Doing About It
Our daily soundscape is a cacophony of earsplitting jets, motorcycles, and construction sites. Engineers know how to eliminate and control noise, but other countries are ahead of the U.S. when it comes to keeping the quiet - with related health benefits.
Erica Walker had a studio in her Brookline, Mass. apartment where she worked as a bookbinder and furniture maker. That was until a family with two rowdy children moved in above her.
The kids ran amuck, disrupting her sleep and work. Ear plugs weren’t enough to blot out the commotion. Aside from anger and a sense of lost control, the noise increased her heart rate and made her stomach feel like it was dropping, she says.
That’s when Walker realized that noise is a public health problem, not merely an annoyance. She set up her own “mini study” on how the clamor was affecting her. She monitored sound levels in her apartment and sent saliva samples to a lab to measure her stress levels.
Walker ultimately sold her craft equipment and returned to school to study public health. Today she is assistant professor of epidemiology and director of the Community Noise Lab at the Brown University School of Public Health. “We treat noise like a first world problem—like a sacrifice we should have to make for modern conveniences. But it’s a serious environmental stressor,” she asserts.
Our daily soundscape is a cacophony of earsplitting jets, motorcycles, crying babies, construction sites or gunshots if you’re in the military. Noise exposure is the primary cause of preventable hearing loss. Researchers have identified links between excessive noise and a heightened risk of heart disease, metabolic disorders, anxiety, depression, sleep disorders, and impaired cognition. Even wildlife suffers. Blasting oil drills and loud shipping vessels impede the breeding, feeding and migration of whales and dolphins.
At one time, the federal government had our back… and our ears. Congress passed the Noise Control Act in 1972. The Environmental Protection Agency set up the Office of Noise Abatement and Control (ONAC) to launch research, explore solutions and establish noise emission standards. But ONAC was defunded in 1981 amidst a swirl of antiregulatory sentiment.
Impossibly Loud and Unhealthy
Daniel Fink. a physician, WHO consultant, and board chair of The Quiet Coalition, a program of the nonprofit Quiet Communities, likens the effect of noise to the invisible but cumulative harm of second-hand smoke. About 1 in 4 adults in the U.S. who report excellent to good hearing already have some hearing loss. The injury can happen after one loud concert or from years with a blaring TV. Some people are more genetically susceptible to noise-related hearing loss than others.
“People say noise isn’t a big deal but it bothers your body whether you realize it or not,” says Ted Rueter, director of Noise Free America: A Coalition to Promote Quiet. Noise can chip away at your ears or cardiovascular system even while you’re sleeping. Rueter became a “quiet advocate” while a professor at UCLA two decades ago. He was plagued by headaches, fatigue and sleep deprivation caused by the hubbub of Los Angeles, he says.
The louder a sound is, and the longer you are exposed to it, the more likely it will cause nerve damage and harmful fluid buildup in your inner ear. Normal speech is 50-60 decibels (dBs). The EPA recommends that 24-hour exposure to noise should be no higher than 70 weighted decibels over 24 hours (weighted to approximate how the human ear perceives the sound) to prevent hearing loss but a 55 dB limit is recommended to protect against other harms from noise, too.
The decibel scale is logarithmic. That means 80 dB is 10 times louder than 70 dB. Trucks and motorcycles run 90 dBs. A gas-powered leaf blower, jackhammer or snow blower will cost you 100 dBs. A rock concert is in the 110 dB range. Aircraft takeoffs or sirens? 120 dBs.
Walker, the Brown professor, says that sound measurements often use misleading metrics, though, because they don’t include low frequency sound that disturb the body. The high frequency of a screeching bus will register in decibels but the sound that makes your chest reverberate is not accounted for, she explains. ‘How loud?’ is a superficial take when it comes to noise, Walker says.

After realizing the impact of noise on her own health, Erica Walker was inspired to change careers and become director of the Community Noise Lab at the Brown University School of Public Health.
Erica Walker
Fink adds that the extent to which noise impairs hearing is underestimated. People assume hearing loss is due to age but it’s not inevitable, he says. He cites studies of older people living in quiet, isolated areas who maintain excellent hearing. Just like you can prevent wrinkles by using sunscreen, you can preserve hearing by using ear plugs when attending fireworks or hockey games.
You can enable push notifications on a Smart Watch to alert you at a bar exceeding healthy sound levels. Free apps like SoundPrint, iHEARu, or NoiseTube can do decibel checks, too, but you don’t need one, says Fink. “If you can’t carry a conversation at normal volume, it’s too loud and your auditory health is at risk,” he says.
About 40 million U.S. adults, ages 20-69, have noise-induced hearing loss. Fink is among them after experiencing tinnitus (ringing or buzzing in the ears) on leaving a raucous New Year’s Eve party in 2007. The condition is permanent and he wears earplugs now for protection.
Fewer are aware of the link between noise pollution and heart disease. Piercing noise is stressful, raising blood pressure and heart rate. If you live near a freeway or constantly barking dog, the chronic sound stress can trigger systemic inflammation and the vascular changes associated with heart attacks and stroke.
Researchers at Rutgers University’s Robert Wood Johnson Medical School, working with data from the state’s Bureau of Transportation, determined that 1 in 20 heart attacks in New Jersey during 2018 were due to noise from highways, trains and air traffic. That’s 800 heart attack hospitalizations in the state that year.
Another study showed that incidence of hypertension and hardening arteries decreased during the Covid-19 air lockdown among Poles in Krakow routinely exposed to aircraft noise. The authors, comparing their pre-pandemic 2015 results to 2020 data, concluded it was no coincidence.
Mental health takes a hit, too. Chronic noise can provoke anxiety, depression and violence. Cognitively, there is ample evidence that noise disturbance lowers student achievement and worker productivity, and hearing loss among older people can speed up cognitive decline.
Noise also contributes to health disparities. People in neighborhoods with low socioeconomic status and a higher percentage of minority residents bear the brunt of noise. Affluent people have the means to live far from airports, factories, and honking traffic.
Out, Out, Damn Noise
Europe is ahead of the U.S. in tackling noise pollution. The World Health Organization developed policy guidelines used by the European Environment Agency to establish noise regulations and standards, and progress reports are issued.
Americans are relying too much on personal protective equipment (PPE) instead of eliminating or controlling noise. The Centers of Disease Control and Prevention rank PPE as the least useful response. Earplugs and muffs are effective, says Walker, but these devices are “a band-aid on a waterfall.”
Editing out noise during product design is the goal. Engineers have an arsenal of techniques and know-how for that. The problem is that these solutions aren’t being applied.
A better way to lower the volume is by maintaining or substituting equipment intended for common use. Piercing building alarms can be replaced with visual signals that flash alerts. Clanking chain and gear drives can be swapped out with belt drives. Acoustical barriers can wall off highway noise. Hospitals can soften beeping monitors and limit loudspeaker blasts. Double paned windows preserve quiet.
Editing out noise during product design is the goal. Engineers have an arsenal of techniques and know-how for that. The problem is that these solutions aren’t being applied, says Jim Thompson, an engineer and editor of the Noise Control Engineering Journal, published by the Institute of Noise Control Engineering of the USA
Engineers have materials to insulate, absorb, reflect, block, seal or diffuse noise. Building walls can be padded. Metal gears and parts can be replaced with plastic. Clattering equipment wheels can be rubberized. In recent years, building certifications such as LEED have put more emphasis on designs that minimize harmful noise.
Walker faults urban planners, too. A city’s narrow streets and taller buildings create a canyon effect which intensifies noise. City planners could use bypasses, rerouting, and other infrastructure strategies to pump down traffic volume. Sound-absorbing asphalt pavement exists, too.
Some municipalities are taking innovative measures on their own. Noise cameras have been installed in Knoxville, Miami and New York City this year and six California cities will join suit next year. If your muffler or audio system registers 86 dB or higher, you may receive a warning, fine or citation, similar to how a red-light camera works. Rueter predicts these cameras will become commonplace.
Based on understanding how metabolic processes affect noise-induced hearing loss in animal models, scientists are exploring whether pharmacological interventions might work to inhibit cellular damage or improve cellular defenses against noise.
Washington, DC, and the University of Southern California have banned gas-powered leaf blowers in lieu of quieter battery-powered models to reduce both noise and air pollution. California will be the first state to ban the sale of gas-powered lawn equipment starting 2024.
New York state legislators enacted the SLEEP (Stop Loud and Excessive Exhaust Pollution) Act in 2021. This measure increases enforcement and fines against motorists and repair shops that illegally modify mufflers and exhaust systems for effect.
“A lot more basic science and application research is needed [to control noise],” says Thompson, noting that funding for this largely dried up after the 1970s. Based on understanding how metabolic processes affect noise-induced hearing loss in animal models, scientists are exploring whether pharmacological interventions might work to inhibit cellular damage or improve cellular defenses against noise.
Studying biochemical or known genetic markers for noise risk could lead to other methods for preventing hearing loss. This would offer an opportunity to identify people with significant risk so those more susceptible to hearing loss could start taking precautions to avoid noise or protect their ears in childhood.
These efforts could become more pressing in the near future, with the anticipated onslaught of drones, rising needs for air conditioners, and urban sprawl boding poorly for the soundscape. This, as deforestation destroys natural carbon absorption reservoirs and removes sound-buffering trees.
“Local and state governments don’t have a plan to deal with [noise] now or in the future,” says Walker. “We need to think about this with intentionality.”

