Your Digital Avatar May One Day Get Sick Before You Do

Artificial neurons in a concept of artificial intelligence.
Artificial intelligence is everywhere, just not in the way you think it is.
These networks, loosely designed after the human brain, are interconnected computers that have the ability to "learn."
"There's the perception of AI in the glossy magazines," says Anders Kofod-Petersen, a professor of Artificial Intelligence at the Norwegian University of Science and Technology. "That's the sci-fi version. It resembles the small guy in the movie AI. It might be benevolent or it might be evil, but it's generally intelligent and conscious."
"And this is, of course, as far from the truth as you can possibly get."
What Exactly Is Artificial Intelligence, Anyway?
Let's start with how you got to this piece. You likely came to it through social media. Your Facebook account, Twitter feed, or perhaps a Google search. AI influences all of those things, machine learning helping to run the algorithms that decide what you see, when, and where. AI isn't the little humanoid figure; it's the system that controls the figure.
"AI is being confused with robotics," Eleonore Pauwels, Director of the Anticipatory Intelligence Lab with the Science and Technology Innovation Program at the Wilson Center, says. "What AI is right now is a data optimization system, a very powerful data optimization system."
The revolution in recent years hasn't come from the method scientists and other researchers use. The general ideas and philosophies have been around since the late 1960s. Instead, the big change has been the dramatic increase in computing power, primarily due to the development of neural networks. These networks, loosely designed after the human brain, are interconnected computers that have the ability to "learn." An AI, for example, can be taught to spot a picture of a cat by looking at hundreds of thousands of pictures that have been labeled "cat" and "learning" what a cat looks like. Or an AI can beat a human at Go, an achievement that just five years ago Kofod-Petersen thought wouldn't be accomplished for decades.
"It's very difficult to argue that something is intelligent if it can't learn, and these algorithms are getting pretty good at learning stuff. What they are not good at is learning how to learn."
Medicine is the field where this expertise in perception tasks might have the most influence. It's already having an impact as iPhones use AI to detect cancer, Apple watches alert the wearer to a heart problem, AI spots tuberculosis and the spread of breast cancer with a higher accuracy than human doctors, and more. Every few months, another study demonstrates more possibility. (The New Yorker published an article about medicine and AI last year, so you know it's a serious topic.)
But this is only the beginning. "I personally think genomics and precision medicine is where AI is going to be the biggest game-changer," Pauwels says. "It's going to completely change how we think about health, our genomes, and how we think about our relationship between our genotype and phenotype."
The Fundamental Breakthrough That Must Be Solved
To get there, however, researchers will need to make another breakthrough, and there's debate about how long that will take. Kofod-Petersen explains: "If we want to move from this narrow intelligence to this broader intelligence, that's a very difficult problem. It basically boils down to that we haven't got a clue about what intelligence actually is. We don't know what intelligence means in a biological sense. We think we might recognize it but we're not completely sure. There isn't a working definition. We kind of agree with the biologists that learning is an aspect of it. It's very difficult to argue that something is intelligent if it can't learn, and these algorithms are getting pretty good at learning stuff. What they are not good at is learning how to learn. They can learn specific tasks but we haven't approached how to teach them to learn to learn."
In other words, current AI is very, very good at identifying that a picture of a cat is, in fact, a cat – and getting better at doing so at an incredibly rapid pace – but the system only knows what a "cat" is because that's what a programmer told it a furry thing with whiskers and two pointy ears is called. If the programmer instead decided to label the training images as "dogs," the AI wouldn't say "no, that's a cat." Instead, it would simply call a furry thing with whiskers and two pointy ears a dog. AI systems lack the explicit inference that humans do effortlessly, almost without thinking.
Pauwels believes that the next step is for AI to transition from supervised to unsupervised learning. The latter means that the AI isn't answering questions that a programmer asks it ("Is this a cat?"). Instead, it's almost like it's looking at the data it has, coming up with its own questions and hypothesis, and answering them or putting them to the test. Combining this ability with the frankly insane processing power of the computer system could result in game-changing discoveries.
In the not-too-distant future, a doctor could run diagnostics on a digital avatar, watching which medical conditions present themselves before the person gets sick in real life.
One company in China plans to develop a way to create a digital avatar of an individual person, then simulate that person's health and medical information into the future. In the not-too-distant future, a doctor could run diagnostics on a digital avatar, watching which medical conditions presented themselves – cancer or a heart condition or anything, really – and help the real-life version prevent those conditions from beginning or treating them before they became a life-threatening issue.
That, obviously, would be an incredibly powerful technology, and it's just one of the many possibilities that unsupervised AI presents. It's also terrifying in the potential for misuse. Even the term "unsupervised AI" brings to mind a dystopian landscape where AI takes over and enslaves humanity. (Pick your favorite movie. There are dozens.) This is a concern, something for developers, programmers, and scientists to consider as they build the systems of the future.
The Ethical Problem That Deserves More Attention
But the more immediate concern about AI is much more mundane. We think of AI as an unbiased system. That's incorrect. Algorithms, after all, are designed by someone or a team, and those people have explicit or implicit biases. Intentionally, or more likely not, they introduce these biases into the very code that forms the basis for the AI. Current systems have a bias against people of color. Facebook tried to rectify the situation and failed. These are two small examples of a larger, potentially systemic problem.
It's vital and necessary for the people developing AI today to be aware of these issues. And, yes, avoid sending us to the brink of a James Cameron movie. But AI is too powerful a tool to ignore. Today, it's identifying cats and on the verge of detecting cancer. In not too many tomorrows, it will be on the forefront of medical innovation. If we are careful, aware, and smart, it will help simulate results, create designer drugs, and revolutionize individualize medicine. "AI is the only way to get there," Pauwels says.
Recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen as soon as 18 months from now
Like all those whose kidneys have failed, Scott Burton’s life revolves around dialysis. For nearly two decades, Burton has been hooked up (or, since 2020, has hooked himself up at home) to a dialysis machine that performs the job his kidneys normally would. The process is arduous, time-consuming, and expensive. Except for a brief window before his body rejected a kidney transplant, Burton has depended on machines to take the place of his kidneys since he was 12-years-old. His whole life, the 39-year-old says, revolves around dialysis.
“Whenever I try to plan anything, I also have to plan my dialysis,” says Burton says, who works as a freelance videographer and editor. “It’s a full-time job in itself.”
Many of those on dialysis are in line for a kidney transplant that would allow them to trade thrice-weekly dialysis and strict dietary limits for a lifetime of immunosuppressants. Burton’s previous transplant means that his body will likely reject another donated kidney unless it matches perfectly—something he’s not counting on. It’s why he’s enthusiastic about the development of artificial kidneys, small wearable or implantable devices that would do the job of a healthy kidney while giving users like Burton more flexibility for traveling, working, and more.
Still, the devices aren’t ready for testing in humans—yet. But recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen as soon as 18 months from now, according to Jonathan Himmelfarb, a nephrologist at the University of Washington.
“It would liberate people with kidney failure,” Himmelfarb says.
An engineering marvel
Compared to the heart or the brain, the kidney doesn’t get as much respect from the medical profession, but its job is far more complex. “It does hundreds of different things,” says UCLA’s Ira Kurtz.
Kurtz would know. He’s worked as a nephrologist for 37 years, devoting his career to helping those with kidney disease. While his colleagues in cardiology and endocrinology have seen major advances in the development of artificial hearts and insulin pumps, little has changed for patients on hemodialysis. The machines remain bulky and require large volumes of a liquid called dialysate to remove toxins from a patient’s blood, along with gallons of purified water. A kidney transplant is the next best thing to someone’s own, functioning organ, but with over 600,000 Americans on dialysis and only about 100,000 kidney transplants each year, most of those in kidney failure are stuck on dialysis.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. Each of the 45 different cell types in the kidney do something different.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. To build an artificial heart, Kurtz says, you basically need to engineer a pump. An artificial pancreas needs to balance blood sugar levels with insulin secretion. While neither of these tasks is simple, they are fairly straightforward. The kidney, on the other hand, does more than get rid of waste products like urea and other toxins. Each of the 45 different cell types in the kidney do something different, helping to regulate electrolytes like sodium, potassium, and phosphorous; maintaining blood pressure and water balance; guiding the body’s hormonal and inflammatory responses; and aiding in the formation of red blood cells.

There's been little progress for patients during Ira Kurtz's 37 years as a nephrologist. Artificial kidneys would change that.
UCLA
Dialysis primarily filters waste, and does so well enough to keep someone alive, but it isn’t a true artificial kidney because it doesn’t perform the kidney’s other jobs, according to Kurtz, such as sensing levels of toxins, wastes, and electrolytes in the blood. Due to the size and water requirements of existing dialysis machines, the equipment isn’t portable. Physicians write a prescription for a certain duration of dialysis and assess how well it’s working with semi-regular blood tests. The process of dialysis itself, however, is conducted blind. Doctors can’t tell how much dialysis a patient needs based on kidney values at the time of treatment, says Meera Harhay, a nephrologist at Drexel University in Philadelphia.
But it’s the impact of dialysis on their day-to-day lives that creates the most problems for patients. Only one-quarter of those on dialysis are able to remain employed (compared to 85% of similar-aged adults), and many report a low quality of life. Having more flexibility in life would make a major different to her patients, Harhay says.
“Almost half their week is taken up by the burden of their treatment. It really eats away at their freedom and their ability to do things that add value to their life,” she says.
Art imitates life
The challenge for artificial kidney designers was how to compress the kidney’s natural functions into a portable, wearable, or implantable device that wouldn’t need constant access to gallons of purified and sterilized water. The other universal challenge they faced was ensuring that any part of the artificial kidney that would come in contact with blood was kept germ-free to prevent infection.
As part of last year’s KidneyX Prize, a partnership between the U.S. Department of Health and Human Services and the American Society of Nephrology, inventors were challenged to create prototypes for artificial kidneys. Himmelfarb’s team at the University of Washington’s Center for Dialysis Innovation won the prize by focusing on miniaturizing existing technologies to create a portable dialysis machine. The backpack sized AKTIV device (Ambulatory Kidney to Increase Vitality) will recycle dialysate in a closed loop system that removes urea from blood and uses light-based chemical reactions to convert the urea to nitrogen and carbon dioxide, which allows the dialysate to be recirculated.
Himmelfarb says that the AKTIV can be used when at home, work, or traveling, which will give users more flexibility and freedom. “If you had a 30-pound device that you could put in the overhead bins when traveling, you could go visit your grandkids,” he says.
Kurtz’s team at UCLA partnered with the U.S. Kidney Research Corporation and Arkansas University to develop a dialysate-free desktop device (about the size of a small printer) as the first phase of a progression that will he hopes will lead to something small and implantable. Part of the reason for the artificial kidney’s size, Kurtz says, is the number of functions his team are cramming into it. Not only will it filter urea from blood, but it will also use electricity to help regulate electrolyte levels in a process called electrodeionization. Kurtz emphasizes that these additional functions are what makes his design a true artificial kidney instead of just a small dialysis machine.
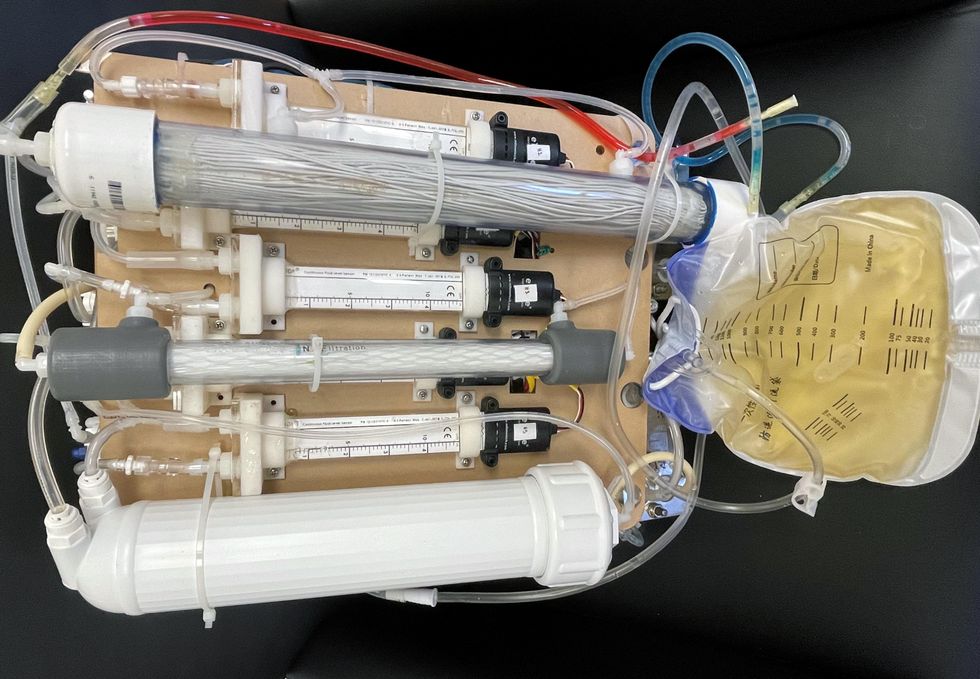
One version of an artificial kidney.
UCLA
“It doesn't have just a static function. It has a bank of sensors that measure chemicals in the blood and feeds that information back to the device,” Kurtz says.
Other startups are getting in on the game. Nephria Bio, a spinout from the South Korean-based EOFlow, is working to develop a wearable dialysis device, akin to an insulin pump, that uses miniature cartridges with nanomaterial filters to clean blood (Harhay is a scientific advisor to Nephria). Ian Welsford, Nephria’s co-founder and CTO, says that the device’s design means that it can also be used to treat acute kidney injuries in resource-limited settings. These potentials have garnered interest and investment in artificial kidneys from the U.S. Department of Defense.
For his part, Burton is most interested in an implantable device, as that would give him the most freedom. Even having a regular outpatient procedure to change batteries or filters would be a minor inconvenience to him.
“Being plugged into a machine, that’s not mimicking life,” he says.
Today’s more than 20,000 mental health apps have a wide range of functionalities and business models. Many of them can be useful for depression.
Even before the pandemic created a need for more telehealth options, depression was a hot area of research for app developers. Given the high prevalence of depression and its connection to suicidality — especially among today’s teenagers and young adults who grew up with mobile devices, use them often, and experience these conditions with alarming frequency — apps for depression could be not only useful but lifesaving.
“For people who are not depressed, but have been depressed in the past, the apps can be helpful for maintaining positive thinking and behaviors,” said Andrea K. Wittenborn, PhD, director of the Couple and Family Therapy Doctoral Program and a professor in human development and family studies at Michigan State University. “For people who are mildly to severely depressed, apps can be a useful complement to working with a mental health professional.”
Health and fitness apps, in general, number in the hundreds of thousands. These are driving a market expected to reach $102.45 billion by next year. The mobile mental health app market is a small part of this but still sizable at $500 million, with revenues generated through user health insurance, employers, and direct payments from individuals.
Apps can provide data that health professionals cannot gather on their own. People’s constant interaction with smartphones and wearable devices yields data on many health conditions for millions of patients in their natural environments and while they go about their usual activities. Compared with the in-office measurements of weight and blood pressure and the brevity of doctor-patient interactions, the thousands of data points gathered unobtrusively over an extended time period provide a far better and more detailed picture of the person and their health.
At their most advanced level, apps for mental health, including depression, passively gather data on how the user touches and interacts with the mobile device through changes in digital biomarkers that relate to depressive symptoms and other conditions.
Building on three decades of research since early “apps” were used for delivering treatment manuals to health professionals, today’s more than 20,000 mental health apps have a wide range of functionalities and business models. Many of these apps can be useful for depression.
Some apps primarily provide a virtual connection to a group of mental health professionals employed or contracted by the app. Others have options for meditation, sleeping or, in the case of industry leaders Calm and Headspace, overall well-being. On the cutting edge are apps that detect changes in a person’s use of mobile devices and their interactions with them.
Apps such as AbleTo, Happify Health, and Woebot Health focus on cognitive behavioral therapy, a type of counseling with proven potential to change a person’s behaviors and feelings. “CBT has been demonstrated in innumerable studies over the last several decades to be effective in the treatment of behavioral health conditions such as depression and anxiety disorders,” said Dr. Reena Pande, chief medical officer at AbleTo. “CBT is intended to be delivered as a structured intervention incorporating key elements, including behavioral activation and adaptive thinking strategies.”
These CBT skills help break the negative self-talk (rumination) common in patients with depression. They are taught and reinforced by some self-guided apps, using either artificial intelligence or programmed interactions with users. Apps can address loneliness and isolation through connections with others, even when a symptomatic person doesn’t feel like leaving the house.
At their most advanced level, apps for mental health, including depression, passively gather data on how the user touches and interacts with the mobile device through changes in “digital biomarkers” that can be associated with onset or worsening of depressive symptoms and other cognitive conditions. In one study, Mindstrong Health gathered a year’s worth of data on how people use their smartphones, such as scrolling through articles, typing and clicking. Mindstrong, whose founders include former leaders of the National Institutes of Health, modeled the timing and order of these actions to make assessments that correlated closely with gold-standard tests of cognitive function.
National organizations of mental health professionals have been following the expanding number of available apps over the years with keen interest. App Advisor is an initiative of the American Psychiatric Association that helps psychiatrists and other mental health professionals navigate the issues raised by mobile health technology. App Advisor does not rate or recommend particular apps but rather provides guidance about why apps should be assessed and how health professionals can do this.
A website that does review mental health apps is One Mind Psyber Guide, an independent nonprofit that partners with several national organizations. One Mind users can select among numerous search terms for the condition and therapeutic approach of interest. Apps are rated on a five-point scale, with reviews written by professionals in the field.
Do mental health apps related to depression have the kind of safety and effectiveness data required for medications and other medical interventions? Not always — and not often. Yet the overall results have shown early promise, Wittenborn noted.
“Studies that have attempted to detect depression from smartphone and wearable sensors [during a single session] have ranged in accuracy from about 86 to 89 percent,” Wittenborn said. “Studies that tried to predict changes in depression over time have been less accurate, with accuracy ranging from 59 to 85 percent.”
The Food and Drug Administration encourages the development of apps and has approved a few of them—mostly ones used by health professionals—but it is generally “hands off,” according to the American Psychiatric Association. The FDA has published a list of examples of software (including programming of apps) that it does not plan to regulate because they pose low risk to the public. First on the list is software that helps patients with diagnosed psychiatric conditions, including depression, maintain their behavioral coping skills by providing a “Skill of the Day” technique or message.
On its App Advisor site, the American Psychiatric Association says mental health apps can be dangerous or cause harm in multiple ways, such as by providing false information, overstating the app’s therapeutic value, selling personal data without clearly notifying users, and collecting data that isn’t relevant to mental health.
Although there is currently reason for caution, patients may eventually come to expect mental health professionals to recommend apps, especially as their rating systems, features and capabilities expand. Through such apps, patients might experience more and higher quality interactions with their mental health professionals. “Apps will continue to be refined and become more effective through future research,” said Wittenborn. “They will become more integrated into practice over time.”