Your Digital Avatar May One Day Get Sick Before You Do

Artificial neurons in a concept of artificial intelligence.
Artificial intelligence is everywhere, just not in the way you think it is.
These networks, loosely designed after the human brain, are interconnected computers that have the ability to "learn."
"There's the perception of AI in the glossy magazines," says Anders Kofod-Petersen, a professor of Artificial Intelligence at the Norwegian University of Science and Technology. "That's the sci-fi version. It resembles the small guy in the movie AI. It might be benevolent or it might be evil, but it's generally intelligent and conscious."
"And this is, of course, as far from the truth as you can possibly get."
What Exactly Is Artificial Intelligence, Anyway?
Let's start with how you got to this piece. You likely came to it through social media. Your Facebook account, Twitter feed, or perhaps a Google search. AI influences all of those things, machine learning helping to run the algorithms that decide what you see, when, and where. AI isn't the little humanoid figure; it's the system that controls the figure.
"AI is being confused with robotics," Eleonore Pauwels, Director of the Anticipatory Intelligence Lab with the Science and Technology Innovation Program at the Wilson Center, says. "What AI is right now is a data optimization system, a very powerful data optimization system."
The revolution in recent years hasn't come from the method scientists and other researchers use. The general ideas and philosophies have been around since the late 1960s. Instead, the big change has been the dramatic increase in computing power, primarily due to the development of neural networks. These networks, loosely designed after the human brain, are interconnected computers that have the ability to "learn." An AI, for example, can be taught to spot a picture of a cat by looking at hundreds of thousands of pictures that have been labeled "cat" and "learning" what a cat looks like. Or an AI can beat a human at Go, an achievement that just five years ago Kofod-Petersen thought wouldn't be accomplished for decades.
"It's very difficult to argue that something is intelligent if it can't learn, and these algorithms are getting pretty good at learning stuff. What they are not good at is learning how to learn."
Medicine is the field where this expertise in perception tasks might have the most influence. It's already having an impact as iPhones use AI to detect cancer, Apple watches alert the wearer to a heart problem, AI spots tuberculosis and the spread of breast cancer with a higher accuracy than human doctors, and more. Every few months, another study demonstrates more possibility. (The New Yorker published an article about medicine and AI last year, so you know it's a serious topic.)
But this is only the beginning. "I personally think genomics and precision medicine is where AI is going to be the biggest game-changer," Pauwels says. "It's going to completely change how we think about health, our genomes, and how we think about our relationship between our genotype and phenotype."
The Fundamental Breakthrough That Must Be Solved
To get there, however, researchers will need to make another breakthrough, and there's debate about how long that will take. Kofod-Petersen explains: "If we want to move from this narrow intelligence to this broader intelligence, that's a very difficult problem. It basically boils down to that we haven't got a clue about what intelligence actually is. We don't know what intelligence means in a biological sense. We think we might recognize it but we're not completely sure. There isn't a working definition. We kind of agree with the biologists that learning is an aspect of it. It's very difficult to argue that something is intelligent if it can't learn, and these algorithms are getting pretty good at learning stuff. What they are not good at is learning how to learn. They can learn specific tasks but we haven't approached how to teach them to learn to learn."
In other words, current AI is very, very good at identifying that a picture of a cat is, in fact, a cat – and getting better at doing so at an incredibly rapid pace – but the system only knows what a "cat" is because that's what a programmer told it a furry thing with whiskers and two pointy ears is called. If the programmer instead decided to label the training images as "dogs," the AI wouldn't say "no, that's a cat." Instead, it would simply call a furry thing with whiskers and two pointy ears a dog. AI systems lack the explicit inference that humans do effortlessly, almost without thinking.
Pauwels believes that the next step is for AI to transition from supervised to unsupervised learning. The latter means that the AI isn't answering questions that a programmer asks it ("Is this a cat?"). Instead, it's almost like it's looking at the data it has, coming up with its own questions and hypothesis, and answering them or putting them to the test. Combining this ability with the frankly insane processing power of the computer system could result in game-changing discoveries.
In the not-too-distant future, a doctor could run diagnostics on a digital avatar, watching which medical conditions present themselves before the person gets sick in real life.
One company in China plans to develop a way to create a digital avatar of an individual person, then simulate that person's health and medical information into the future. In the not-too-distant future, a doctor could run diagnostics on a digital avatar, watching which medical conditions presented themselves – cancer or a heart condition or anything, really – and help the real-life version prevent those conditions from beginning or treating them before they became a life-threatening issue.
That, obviously, would be an incredibly powerful technology, and it's just one of the many possibilities that unsupervised AI presents. It's also terrifying in the potential for misuse. Even the term "unsupervised AI" brings to mind a dystopian landscape where AI takes over and enslaves humanity. (Pick your favorite movie. There are dozens.) This is a concern, something for developers, programmers, and scientists to consider as they build the systems of the future.
The Ethical Problem That Deserves More Attention
But the more immediate concern about AI is much more mundane. We think of AI as an unbiased system. That's incorrect. Algorithms, after all, are designed by someone or a team, and those people have explicit or implicit biases. Intentionally, or more likely not, they introduce these biases into the very code that forms the basis for the AI. Current systems have a bias against people of color. Facebook tried to rectify the situation and failed. These are two small examples of a larger, potentially systemic problem.
It's vital and necessary for the people developing AI today to be aware of these issues. And, yes, avoid sending us to the brink of a James Cameron movie. But AI is too powerful a tool to ignore. Today, it's identifying cats and on the verge of detecting cancer. In not too many tomorrows, it will be on the forefront of medical innovation. If we are careful, aware, and smart, it will help simulate results, create designer drugs, and revolutionize individualize medicine. "AI is the only way to get there," Pauwels says.
A Rare Disease Just "Messed with the Wrong Mother." Now She's Fighting to Beat It Once and For All.
Amber Freed and Maxwell near their home in Denver, Colorado.
Amber Freed felt she was the happiest mother on earth when she gave birth to twins in March 2017. But that euphoric feeling began to fade over the next few months, as she realized her son wasn't making the same developmental milestones as his sister. "I had a perfect benchmark because they were twins, and I saw that Maxwell was floppy—he didn't have muscle tone and couldn't hold his neck up," she recalls. At first doctors placated her with statements that boys sometimes develop slower than girls, but the difference was just too drastic. At 10 month old, Maxwell had never reached to grab a toy. In fact, he had never even used his hands.
Thinking that perhaps Maxwell couldn't see well, Freed took him to an ophthalmologist who was the first to confirm her worst fears. He didn't find Maxwell to have vision problems, but he thought there was something wrong with the boy's brain. He had seen similar cases before and they always turned out to be rare disorders, and always fatal. "Start preparing yourself for your child not to live," he had said.
Getting the diagnosis took months of painful, invasive procedures, as well as fighting with the health insurance to get the genetic testing approved. Finally, in June 2018, doctors at the Children's Hospital Colorado gave the Freeds their son's diagnosis—a genetic mutation so rare it didn't even have a name, just a bunch of letters jammed together into a word SLC6A1—same as the name of the mutated gene. The mutation, with only 40 cases known worldwide at the time, caused developmental disabilities, movement and speech disorders, and a debilitating form of epilepsy.
The doctors didn't know much about the disorder, but they said that Maxwell would also regress in his development when he turned three or four. They couldn't tell how long he would live. "Hopefully you would become an expert and educate us about it," they said, as they gave Freed a five-page paper on the SLC6A1 and told her to start calling scientists if she wanted to help her son in any way. When she Googled the name, nothing came up. She felt horrified. "Our disease was too rare to care."
Freed's husband, a 6'2'' college football player broke down in sobs and she realized that if anything could be done to help Maxwell, she'd have be the one to do it. "I understood that I had to fight like a mother," she says. "And a determined mother can do a lot of things."

The Freed family.
Courtesy Amber Freed
She quit her job as an equity analyst the day of the diagnosis and became a full-time SLC6A1 citizen scientist looking for researchers studying mutations of this gene. In the wee hours of the morning, she called scientists in Europe. As the day progressed, she called researchers on the East Coast, followed by the West in the afternoon. In the evening, she switched to Asia and Australia. She asked them the same question. "Can you help explain my gene and how do we fix it?"
Scientists need money to do research, so Freed launched Milestones for Maxwell fundraising campaign, and a SLC6A1 Connect patient advocacy nonprofit, dedicated to improving the lives of children and families battling this rare condition. And then it became clear that the mutation wasn't as rare as it seemed. As other parents began to discover her nonprofit, the number of known cases rose from 40 to 100, and later to 400, Freed says. "The disease is only rare until it messes with the wrong mother."
It took one mother to find another to start looking into what's happening inside Maxwell's brain. Freed came across Jeanne Paz, a Gladstone Institutes researcher who studies epilepsy with particular interest in absence or silent seizures—those that don't manifest by convulsions, but rather make patients absently stare into space—and that's one type of seizures Maxwell has. "It's like a brief period of silence in the brain during which the person doesn't pay attention to what's happening, and as soon as they come out of the seizure they are back to life," Paz explains. "It's like a pause button on consciousness." She was working to understand the underlying biology.
To understand how seizures begin, spread and stop, Paz uses optogenetics in mice. From words "genetic" and "optikós," which means visible in Greek, the optogenetics technique involves two steps. First, scientists introduce a light-sensitive gene into a specific brain cell type—for example into excitatory neurons that release glutamate, a neurotransmitter, which activates other cells in the brain. Then they implant a very thin optical fiber into the brain area where they forged these light-sensitive neurons. As they shine the light through the optical fiber, researchers can make excitatory neurons to release glutamate—or instead tell them to stop being active and "shut up". The ability to control what these neurons of interest do, quite literally sheds light onto where seizures start, how they propagate and what cells are involved in stopping them.
"Let's say a seizure started and we shine the light that reduces the activity of specific neurons," Paz explains. "If that stops the seizure, we know that activating those cells was necessary to maintain the seizure." Likewise, shutting down their activity will make the seizure stop.
Freed reached out to Paz in 2019 and the two women had an instant connection. They were both passionate about brain and seizures research, even if for different reasons. Freed asked Paz if she would study her son's seizures and Paz agreed.
To do that, Paz needed mice that carried the SLC6A1 mutation, so Freed found a company in China that created them to specs. The company replaced a mouse SLC6A1 gene with a human mutated one and shipped them over to Paz's lab. "We call them Maxwell mice," Paz says, "and we are now implanting electrodes into them to see which brain regions generate seizures." That would help them understand what goes wrong and what brain cells are malfunctioning in the SLC6A1 mice—and help scientists better understand what might cause seizures in children.
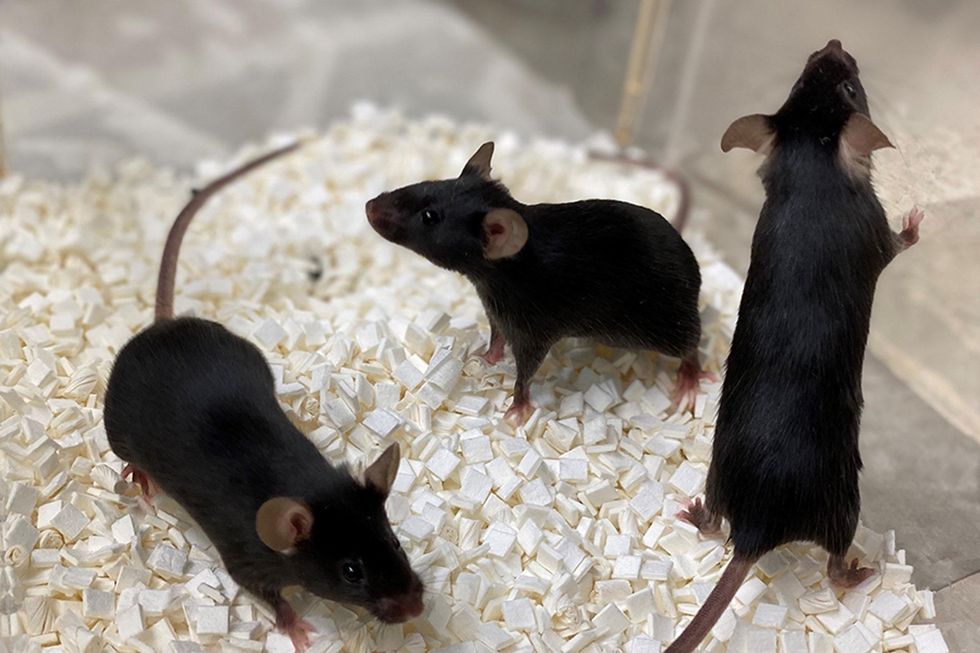
Bred to carry SLC6A1 mutation, these "Maxwell mice" will help better understand this debilitating genetic disease. (These mice are from Vanderbilt University, where researchers are also studying SLC6A1.)
Courtesy Amber Freed
This information—along with other research Amber is funding in other institutions—will inform the development of a novel genetic treatment, in which scientists would deploy a harmless virus to deliver a healthy, working copy of the SLC6A1 gene into the mice brains. They would likely deliver the therapeutic via a spinal tap infusion, and if it works and doesn't produce side effects in mice, the human trials will follow.
In the meantime, Freed is raising money to fund other research of various stop-gap measures. On April 22, 2021, she updated her Milestone for Maxwell page with a post that her nonprofit is funding yet another effort. It is a trial at Weill Cornell Medicine in New York City, in which doctors will use an already FDA-approved drug, which was recently repurposed for the SLC6A1 condition to treat epilepsy in these children. "It will buy us time," Freed says—while the gene therapy effort progresses.
Freed is determined to beat SLC6A1 before it beats down her family. She hopes to put an end to this disease—and similar genetic diseases—once and for all. Her goal is not only to have scientists create a remedy, but also to add the mutation to a newborn screening panel. That way, children born with this condition in the future would receive gene therapy before they even leave the hospital.
"I don't want there to be another Maxwell Freed," she says, "and that's why I am fighting like a mother." The gene therapy trial still might be a few years away, but the Weill Cornell one aims to launch very soon—possibly around Mother's Day. This is yet another milestone for Maxwell, another baby step forward—and the best gift a mother can get.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
On May 13th, scientific and medical experts will discuss and answer questions about the vaccine for those under 16.
This virtual event convened leading scientific and medical experts to address the public's questions and concerns about Covid-19 vaccines in kids and teens. Highlight video below.
DATE:
Thursday, May 13th, 2021
12:30 p.m. - 1:45 p.m. EDT
Dr. H. Dele Davies, M.D., MHCM

Senior Vice Chancellor for Academic Affairs and Dean for Graduate Studies at the University of Nebraska Medical (UNMC). He is an internationally recognized expert in pediatric infectious diseases and a leader in community health.
Dr. Emily Oster, Ph.D.

Professor of Economics at Brown University. She is a best-selling author and parenting guru who has pioneered a method of assessing school safety.
Dr. Tina Q. Tan, M.D.

Professor of Pediatrics at the Feinberg School of Medicine, Northwestern University. She has been involved in several vaccine survey studies that examine the awareness, acceptance, barriers and utilization of recommended preventative vaccines.
Dr. Inci Yildirim, M.D., Ph.D., M.Sc.
Associate Professor of Pediatrics (Infectious Disease); Medical Director, Transplant Infectious Diseases at Yale School of Medicine; Associate Professor of Global Health, Yale Institute for Global Health. She is an investigator for the multi-institutional COVID-19 Prevention Network's (CoVPN) Moderna mRNA-1273 clinical trial for children 6 months to 12 years of age.
About the Event Series
This event is the second of a four-part series co-hosted by Leaps.org, the Aspen Institute Science & Society Program, and the Sabin–Aspen Vaccine Science & Policy Group, with generous support from the Gordon and Betty Moore Foundation and the Howard Hughes Medical Institute.
:
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

