Your Genetic Data Is The New Oil. These Startups Will Pay to Rent It.

A doctor conducts a test on DNA.
Perhaps you're one of the 12 million people who has spit into a tube in recent years to learn the secrets in your genetic code, like your ancestry, your health risks, or your carrier status for certain diseases. If you haven't participated in direct-to-consumer genetic testing, you may know someone who has.
It's for people who want more control over their genetic data--plus a share of the proceeds when and if that data is used.
Mountains of genomic data have been piling up steeply over the last several years, but according to some experts, not enough research and drug discovery is being done with the data collected, and customers rarely have a say in how their data is used. Now, a slew of ambitious startup companies are bringing together the best of blockchain technology and human genomics to help solve these problems.
But First, Why Is Your Genome So Valuable?
Access to genetic information is an obvious boon to scientific and medical progress. In the right hands, it has the potential to save lives and reduce suffering — by facilitating the development of better, safer, more targeted treatments and by shedding light on the role of genetics in countless diseases and medical conditions.
Research requiring access to direct-to-consumer (DTC) genomic data is already well underway. For example, 23andMe, the popular California-based DTC genetic testing company, has published 107 research articles so far, as of this May, using data from their five million-plus customers around the world. Their website states that, on average, of the 80 percent of their customers who have opted to share their genomic data for research purposes, each "individual contributes to 200 different research studies."
And this July, a new collaboration was announced between 23andMe and GlaxoSmithKline, the London-based pharmaceutical company. GlaxoSmithKline will be using data from 23andMe customers to develop new medical treatments, while 23andMe will receive $300 million from the four-year deal. Both companies are poised to profit significantly from their union.
Should 23andMe's customers share in the gains? Peter Pitts, president of the Center for Medicine in the Public Interest, believes they should. "Are they going to offer rebates to people who opt in, so their customers aren't paying for the privilege of 23andMe working with a for-profit company in a for-profit research project?" Pitts told NBC. So far, 23andMe has not announced any plans to share profits with their customers.
But outside of such major partnerships, many researchers are frustrated by the missed opportunities to dig deeper into the correlations between genetics and disease. That's because people's de-identified genomic information is "essentially lying fallow," siloed behind significant security blockades in the interest of preserving their anonymity. So how can both researchers and consumers come out ahead?
Putting Consumers Back in Control
For people who want more control over their genetic data -- plus a share of the proceeds when and if that data is used -- a few companies have paired consumer genomics with blockchain technology to form a new field called "blockchain genomics." Blockchain is a data storage technology that relies on a network of computers, or peer-to-peer setup, making it incredibly difficult to hack. "It's a closed loop of transactions that gets protected and encrypted, and it cannot be changed," says Tanya Woods, a blockchain thought leader and founder of Kind Village, a social impact technology platform.
The vision is to incentivize consumers to share their genomic data and empower researchers to make new breakthroughs.
"So if I agree to give you something and you agree to accept it, we make that exchange, and then that basic framework is captured in a block. … Anything that can be exchanged can be ledgered on blockchain. Anything. It could be real estate, it could be the transfer of artwork, it could be the purchase of a song or any digital content, it could be recognition of a certification," and so on.
The blockchain genomics companies' vision is to incentivize consumers to share their genomic data and empower researchers to make new breakthroughs, all while keeping the data secure and the identities of consumers anonymous.
Consumers, or "partners" as these companies call them, will have a direct say regarding which individuals or organizations can "rent" their data, and will be able to negotiate the amount they receive in exchange. But instead of fiat currency (aka "regular money") as payment, partners will either be remunerated in cryptocurrency unique to the specific company or they will be provided with individual shares of ownership in the database for contributing DNA data and other medical information.
Luna DNA, one of the blockchain genomics companies, "will allow any credible researcher or non-profit to access the databases for a nominal fee," says its president and co-founder, Dawn Barry. Luna DNA's infrastructure was designed to embrace certain conceptions of privacy and privacy law "in which individuals are in total control of their data, including the ability to have their data be 'forgotten' at any time," she said. This is nearly impossible to implement in pre-existing systems that were not designed with full control by the individual in mind.
One of the legal instruments to which Barry referred was the European Union's General Data Protection Regulation, which "states that the data collected on an individual is owned and should be controlled by that individual," she explained. Another is the California Privacy Act that echoes similar principles. "There is a global trend towards more control by the individual that has very deep implications to companies and sites that collect and aggregate data."
David Koepsell, CEO and co-founder of EncrypGen, told Forbes that "Most people are not aware that your DNA contains information about your life expectancy, your proclivity to depression or schizophrenia, your complete ethnic ancestry, your expected intelligence, maybe even your political inclinations" — information that could be misused by insurance companies and employers. And though DTC customers have been assured that their data will stay anonymous, some data can be linked back to consumers' identities. Blockchain may be the answer to these concerns.
Both blockchain technology and the DTC genetic testing arena have a glaring diversity problem.
"The security that's provided by blockchain is tremendous," Woods says. "It's a significant improvement … and as we move toward more digitized economies around the world, these kinds of solutions that are providing security, validity, trust — they're very important."
In the case of blockchain genomics companies like EncrypGen, Luna DNA, Longenesis, and Zenome, each partner who joins would bring a digital copy of their genetic readout from DTC testing companies (like 23andMe or AncestryDNA). The blockchain technology would then be used to record how and for what purposes researchers interact with it. (To learn more about blockchain, check out this helpful visual guide by Reuters.)
Obstacles in the Path to Success
The cryptocurrency approach as a method of payment could be an unattractive lure to consumers if only a limited number of people make transactions in a given currency's network. And the decade-old technology underlying it -- blockchain -- is not yet widely supported, or even well-understood, by the public at large.
"People conflate blockchain with cryptocurrency and bitcoin and all of the concerns and uncertainty thereof," Barry told us. "One can think of cryptocurrency as a single expression of the vast possibilities of the blockchain technology. Blockchain is straightforward in concept and arcane in its implementation."
But blockchain, with its Gini coefficient of 0.98, is one of the most unequal "playing fields" around. The Gini coefficient is a measure of economic inequality, where 0 represents perfect equality and 1 represents perfect inequality. Around 90 percent of bitcoin users, for example, are male, white or Asian, between the ages of 18 and 34, straight, and from middle and upper class families.
The DTC genetic testing arena, too, has a glaring diversity problem. Most DTC genetic test consumers, just like most genetic study participants, are of European descent. In the case of genetic studies, this disparity is largely explained by the fact that most research is done in Europe and North America. In addition to being over 85 percent white, individuals who purchase DTC genetic testing kits are highly educated (about half have more than a college degree), well off (43 percent have a household income of $100,000 or more per year), and are politically liberal (almost 65 percent). Only 14.5 percent of DTC genetic test consumers are non-white, and a mere 5 percent are Hispanic.
Since risk of genetic diseases often varies greatly between ethnic groups, results from DTC tests can be less accurate and less specific for those of non-European ancestry — simply due to a lack of diverse data. The bigger the genetic database, wrote Sarah Zhang for The Atlantic, the more insights 23andMe and other DTC companies "can glean from DNA. That, in turn, means the more [they] can tell customers about their ancestry and health…" Though efforts at recruiting non-white participants have been ongoing, and some successes have been made at improving ancestry tools for people of color, the benefits of genomic gathering in North America are still largely reaped by Caucasians.
So far, it's not yet clear who or how many people will choose to partake in the offerings of blockchain genomics companies.
So one chief hurdle for the blockchain genomics companies is getting the technology into the hands of those who are under-represented in both blockchain and genetic testing research. Women, in particular, may be difficult to bring on board the blockchain genomics bandwagon — though not from lack of interest. Although women make up a significant portion of DTC genetic testing customers (between 50 and 60 percent), their presence is lacking in blockchain and the biotech industry in general.
At the North American Bitcoin Conference in Miami earlier this year, only three women were on stage, compared to 84 men. And the after-party was held in a strip club.
"I was at that conference," Woods told us. "I don't know what happened at the strip club, I didn't observe it. That's not to say it didn't happen … but I enjoyed being at the conference and I enjoyed learning from people who are experimenting in the space and developing in it. Generally, would I have loved to see more women visible? Of course. In tech generally I want to see more women visible, but there's a whole ecosystem shifting that has to happen to make that possible."
Luna's goal is to achieve equal access to a technology (blockchain genomics) that could potentially improve health and quality of life for all involved. But in the merging of two fields that have been unequal since their inception, achieving equal access is one tall order indeed. So far, it's not yet clear who or how many people will choose to participate. LunaDNA's platform has not yet launched; EncrypGen released their beta version just last month.
Sharon Terry, president and CEO of Genetic Alliance — a nonprofit organization that advocates for access to quality genetic services — recently shared a message that reflects the zeitgeist for all those entering the blockchain genomics space: "Be authentic. Tell the truth, even about motives and profits. Be transparent. Engage us. Don't leave us out. Make this real collaboration. Be bold. Take risks. People are dying. It's time to march forward and make a difference."
Jamie Rettinger with his now fiance Amie Purnel-Davis, who helped him through the clinical trial.
Jamie Rettinger was still in his thirties when he first noticed a tiny streak of brown running through the thumbnail of his right hand. It slowly grew wider and the skin underneath began to deteriorate before he went to a local dermatologist in 2013. The doctor thought it was a wart and tried scooping it out, treating the affected area for three years before finally removing the nail bed and sending it off to a pathology lab for analysis.
"I have some bad news for you; what we removed was a five-millimeter melanoma, a cancerous tumor that often spreads," Jamie recalls being told on his return visit. "I'd never heard of cancer coming through a thumbnail," he says. None of his doctors had ever mentioned it either. "I just thought I was being treated for a wart." But nothing was healing and it continued to bleed.
A few months later a surgeon amputated the top half of his thumb. Lymph node biopsy tested negative for spread of the cancer and when the bandages finally came off, Jamie thought his medical issues were resolved.
Melanoma is the deadliest form of skin cancer. About 85,000 people are diagnosed with it each year in the U.S. and more than 8,000 die of the cancer when it spreads to other parts of the body, according to the Centers for Disease Control and Prevention (CDC).
There are two peaks in diagnosis of melanoma; one is in younger women ages 30-40 and often is tied to past use of tanning beds; the second is older men 60+ and is related to outdoor activity from farming to sports. Light-skinned people have a twenty-times greater risk of melanoma than do people with dark skin.
"When I graduated from medical school, in 2005, melanoma was a death sentence" --Diwakar Davar.
Jamie had a follow up PET scan about six months after his surgery. A suspicious spot on his lung led to a biopsy that came back positive for melanoma. The cancer had spread. Treatment with a monoclonal antibody (nivolumab/Opdivo®) didn't prove effective and he was referred to the UPMC Hillman Cancer Center in Pittsburgh, a four-hour drive from his home in western Ohio.
An alternative monoclonal antibody treatment brought on such bad side effects, diarrhea as often as 15 times a day, that it took more than a week of hospitalization to stabilize his condition. The only options left were experimental approaches in clinical trials.
Early research
"When I graduated from medical school, in 2005, melanoma was a death sentence" with a cure rate in the single digits, says Diwakar Davar, 39, an oncologist at UPMC Hillman Cancer Center who specializes in skin cancer. That began to change in 2010 with introduction of the first immunotherapies, monoclonal antibodies, to treat cancer. The antibodies attach to PD-1, a receptor on the surface of T cells of the immune system and on cancer cells. Antibody treatment boosted the melanoma cure rate to about 30 percent. The search was on to understand why some people responded to these drugs and others did not.
At the same time, there was a growing understanding of the role that bacteria in the gut, the gut microbiome, plays in helping to train and maintain the function of the body's various immune cells. Perhaps the bacteria also plays a role in shaping the immune response to cancer therapy.
One clue came from genetically identical mice. Animals ordered from different suppliers sometimes responded differently to the experiments being performed. That difference was traced to different compositions of their gut microbiome; transferring the microbiome from one animal to another in a process known as fecal transplant (FMT) could change their responses to disease or treatment.
When researchers looked at humans, they found that the patients who responded well to immunotherapies had a gut microbiome that looked like healthy normal folks, but patients who didn't respond had missing or reduced strains of bacteria.
Davar and his team knew that FMT had a very successful cure rate in treating the gut dysbiosis of Clostridioides difficile, a persistant intestinal infection, and they wondered if a fecal transplant from a patient who had responded well to cancer immunotherapy treatment might improve the cure rate of patients who did not originally respond to immunotherapies for melanoma.
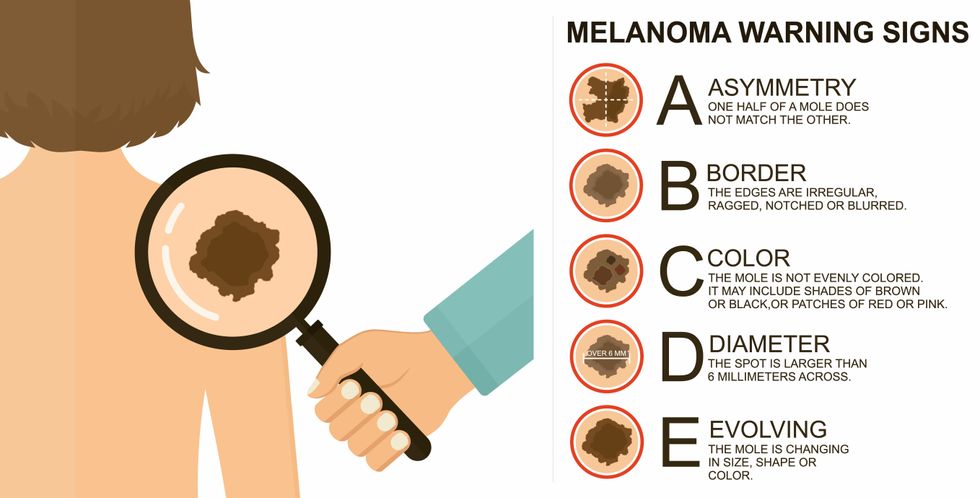
The ABCDE of melanoma detection
Adobe Stock
Clinical trial
"It was pretty weird, I was totally blasted away. Who had thought of this?" Jamie first thought when the hypothesis was explained to him. But Davar's explanation that the procedure might restore some of the beneficial bacterial his gut was lacking, convinced him to try. He quickly signed on in October 2018 to be the first person in the clinical trial.
Fecal donations go through the same safety procedures of screening for and inactivating diseases that are used in processing blood donations to make them safe for transfusion. The procedure itself uses a standard hollow colonoscope designed to screen for colon cancer and remove polyps. The transplant is inserted through the center of the flexible tube.
Most patients are sedated for procedures that use a colonoscope but Jamie doesn't respond to those drugs: "You can't knock me out. I was watching them on the TV going up my own butt. It was kind of unreal at that point," he says. "There were about twelve people in there watching because no one had seen this done before."
A test two weeks after the procedure showed that the FMT had engrafted and the once-missing bacteria were thriving in his gut. More importantly, his body was responding to another monoclonal antibody (pembrolizumab/Keytruda®) and signs of melanoma began to shrink. Every three months he made the four-hour drive from home to Pittsburgh for six rounds of treatment with the antibody drug.
"We were very, very lucky that the first patient had a great response," says Davar. "It allowed us to believe that even though we failed with the next six, we were on the right track. We just needed to tweak the [fecal] cocktail a little better" and enroll patients in the study who had less aggressive tumor growth and were likely to live long enough to complete the extensive rounds of therapy. Six of 15 patients responded positively in the pilot clinical trial that was published in the journal Science.
Davar believes they are beginning to understand the biological mechanisms of why some patients initially do not respond to immunotherapy but later can with a FMT. It is tied to the background level of inflammation produced by the interaction between the microbiome and the immune system. That paper is not yet published.
Surviving cancer
It has been almost a year since the last in his series of cancer treatments and Jamie has no measurable disease. He is cautiously optimistic that his cancer is not simply in remission but is gone for good. "I'm still scared every time I get my scans, because you don't know whether it is going to come back or not. And to realize that it is something that is totally out of my control."
"It was hard for me to regain trust" after being misdiagnosed and mistreated by several doctors he says. But his experience at Hillman helped to restore that trust "because they were interested in me, not just fixing the problem."
He is grateful for the support provided by family and friends over the last eight years. After a pause and a sigh, the ruggedly built 47-year-old says, "If everyone else was dead in my family, I probably wouldn't have been able to do it."
"I never hesitated to ask a question and I never hesitated to get a second opinion." But Jamie acknowledges the experience has made him more aware of the need for regular preventive medical care and a primary care physician. That person might have caught his melanoma at an earlier stage when it was easier to treat.
Davar continues to work on clinical studies to optimize this treatment approach. Perhaps down the road, screening the microbiome will be standard for melanoma and other cancers prior to using immunotherapies, and the FMT will be as simple as swallowing a handful of freeze-dried capsules off the shelf rather than through a colonoscopy. Earlier this year, the Food and Drug Administration approved the first oral fecal microbiota product for C. difficile, hopefully paving the way for more.
An older version of this hit article was first published on May 18, 2021
All organisms can repair damaged tissue, but none do it better than salamanders and newts. A surprising area of science could tell us how they manage this feat - and perhaps even help us develop a similar ability.
All organisms have the capacity to repair or regenerate tissue damage. None can do it better than salamanders or newts, which can regenerate an entire severed limb.
That feat has amazed and delighted man from the dawn of time and led to endless attempts to understand how it happens – and whether we can control it for our own purposes. An exciting new clue toward that understanding has come from a surprising source: research on the decline of cells, called cellular senescence.
Senescence is the last stage in the life of a cell. Whereas some cells simply break up or wither and die off, others transition into a zombie-like state where they can no longer divide. In this liminal phase, the cell still pumps out many different molecules that can affect its neighbors and cause low grade inflammation. Senescence is associated with many of the declining biological functions that characterize aging, such as inflammation and genomic instability.
Oddly enough, newts are one of the few species that do not accumulate senescent cells as they age, according to research over several years by Maximina Yun. A research group leader at the Center for Regenerative Therapies Dresden and the Max Planck Institute of Molecular and Cell Biology and Genetics, in Dresden, Germany, Yun discovered that senescent cells were induced at some stages of regeneration of the salamander limb, “and then, as the regeneration progresses, they disappeared, they were eliminated by the immune system,” she says. “They were present at particular times and then they disappeared.”
Senescent cells added to the edges of the wound helped the healthy muscle cells to “dedifferentiate,” essentially turning back the developmental clock of those cells into more primitive states.
Previous research on senescence in aging had suggested, logically enough, that applying those cells to the stump of a newly severed salamander limb would slow or even stop its regeneration. But Yun stood that idea on its head. She theorized that senescent cells might also play a role in newt limb regeneration, and she tested it by both adding and removing senescent cells from her animals. It turned out she was right, as the newt limbs grew back faster than normal when more senescent cells were included.
Senescent cells added to the edges of the wound helped the healthy muscle cells to “dedifferentiate,” essentially turning back the developmental clock of those cells into more primitive states, which could then be turned into progenitors, a cell type in between stem cells and specialized cells, needed to regrow the muscle tissue of the missing limb. “We think that this ability to dedifferentiate is intrinsically a big part of why salamanders can regenerate all these very complex structures, which other organisms cannot,” she explains.
Yun sees regeneration as a two part problem. First, the cells must be able to sense that their neighbors from the lost limb are not there anymore. Second, they need to be able to produce the intermediary progenitors for regeneration, , to form what is missing. “Molecularly, that must be encoded like a 3D map,” she says, otherwise the new tissue might grow back as a blob, or liver, or fin instead of a limb.
Wound healing
Another recent study, this time at the Mayo Clinic, provides evidence supporting the role of senescent cells in regeneration. Looking closely at molecules that send information between cells in the wound of a mouse, the researchers found that senescent cells appeared near the start of the healing process and then disappeared as healing progressed. In contrast, persistent senescent cells were the hallmark of a chronic wound that did not heal properly. The function and significance of senescence cells depended on both the timing and the context of their environment.
The paper suggests that senescent cells are not all the same. That has become clearer as researchers have been able to identify protein markers on the surface of some senescent cells. The patterns of these proteins differ for some senescent cells compared to others. In biology, such physical differences suggest functional differences, so it is becoming increasingly likely there are subsets of senescent cells with differing functions that have not yet been identified.
There are disagreements within the research community as to whether newts have acquired their regenerative capacity through a unique evolutionary change, or if other animals, including humans, retain this capacity buried somewhere in their genes.
Scientists initially thought that senescent cells couldn’t play a role in regeneration because they could no longer reproduce, says Anthony Atala, a practicing surgeon and bioengineer who leads the Wake Forest Institute for Regenerative Medicine in North Carolina. But Yun’s study points in the other direction. “What this paper shows clearly is that these cells have the potential to be involved in tissue regeneration [in newts]. The question becomes, will these cells be able to do the same in humans.”
As our knowledge of senescent cells increases, Atala thinks we need to embrace a new analogy to help understand them: humans in retirement. They “have acquired a lot of wisdom throughout their whole life and they can help younger people and mentor them to grow to their full potential. We're seeing the same thing with these cells,” he says. They are no longer putting energy into their own reproduction, but the signaling molecules they secrete “can help other cells around them to regenerate.”
There are disagreements within the research community as to whether newts have acquired their regenerative capacity through a unique evolutionary change, or if other animals, including humans, retain this capacity buried somewhere in their genes. If so, it seems that our genes are unable to express this ability, perhaps as part of a tradeoff in acquiring other traits. It is a fertile area of research.
Dedifferentiation is likely to become an important process in the field of regenerative medicine. One extreme example: a lab has been able to turn back the clock and reprogram adult male skin cells into female eggs, a potential milestone in reproductive health. It will be more difficult to control just how far back one wishes to go in the cell's dedifferentiation – part way or all the way back into a stem cell – and then direct it down a different developmental pathway. Yun is optimistic we can learn these tricks from newts.
Senolytics
A growing field of research is using drugs called senolytics to remove senescent cells and slow or even reverse disease of aging.
“Senolytics are great, but senolytics target different types of senescence,” Yun says. “If senescent cells have positive effects in the context of regeneration, of wound healing, then maybe at the beginning of the regeneration process, you may not want to take them out for a little while.”
“If you look at pretty much all biological systems, too little or too much of something can be bad, you have to be in that central zone” and at the proper time, says Atala. “That's true for proteins, sugars, and the drugs that you take. I think the same thing is true for these cells. Why would they be different?”
Our growing understanding that senescence is not a single thing but a variety of things likely means that effective senolytic drugs will not resemble a single sledge hammer but more a carefully manipulated scalpel where some types of senescent cells are removed while others are added. Combinations and timing could be crucial, meaning the difference between regenerating healthy tissue, a scar, or worse.

