A Cure for Sickle Cell Disease Is Coming. Will Patients Accept It?
Many patients in the African-American community are skeptical of new experimental treatments, thanks to a history of medical exploitation in the 20th century.
If any malady proves the fragile grace of the human genome, it is sickle cell disease.
If experimental treatments receive regulatory approval, it would be a watershed breakthrough for tens of thousands of Americans.
It occurs because of a single "misspelled" letter of DNA, causing red blood cells to run low on oxygen and transforming the hemoglobin in each cell into a stiff rod. Normally round cells become rigid crescents that hamper the flow of blood throughout the body, like leaves clumping in a drain.
Strokes in toddlers are merely the beginning of the circulatory calamities this disease may inflict. Most sickled cells cannot carry oxygen through the body, causing anemia as well as excruciating chronic pain. Older patients are at risk of kidney failure, heart disease and all the other collateral damage caused by poor circulation. Few live beyond middle age.
The only way to cure it has been through a bone marrow transplant from a donor, which requires not only a closely matching volunteer, but bouts of chemotherapy to allow new stem cells to take root, as well as rounds of immunosuppressive drugs that may last for years.
Recent advances in genomic medicine may soon alter the disease's outlook, although many obstacles remain.
In one treatment under development, patient's skin cells are converted into stem cells, allowing them to be inserted into the bone marrow without the need for a donor. Another treatment known as gene therapy involves replacing the aberrant gene in the patient's body with new genetic material.
Although both remain in clinical trials -- and also require at least chemotherapy -- they have shown promise. Matthew Hsieh, a hematologist and staff scientist with the National Heart Lung and Blood Institute in Maryland, has performed about 10 gene therapy procedures over the past three years as part of a clinical trial. Ongoing tweaks in the procedure have led to the blood in more recent patients showing sickle cell trait -- not a perfect outcome, but one that leaves patients with far fewer symptoms than if they have the full-blown disease.
If one or both treatments receive regulatory approval, it would be a watershed breakthrough for the tens of thousands of Americans who suffer from the disease.
Yet it is entirely possible many patients may decline the cure.
A Painful History
The vast majority of sickle cell sufferers in the U.S. -- well beyond 90 percent -- are African-American, a population with a historically uneasy relationship toward healthcare.
"There is a lot of data on distrust between African-Americans and American medical institutions," says J. Corey Williams, a psychiatrist with the Children's Hospital of Philadelphia who has written extensively on racial disparities in healthcare. "It comes from a long legacy of feeling victimized by medicine."
"What you hear from many patients is 'I am not going to be your guinea pig, and I am not going to be experimented on.'"
As a result, Williams is among several clinicians interviewed for this story who believe a cure for sickle cell disease would be embraced reluctantly.
"What you hear from many patients is 'I am not going to be your guinea pig, and I am not going to be experimented on.' And so the history of African-Americans and research will manifest as we develop gene therapies for [these] patients," says Christopher L. Edwards, a clinical psychologist and researcher with the Maya Angelou Center for Health Equity at the Wake Forest University School of Medicine.
Fear among African-Americans of becoming guinea pigs is well-founded. The first c-sections and fistula repairs occurring in North America were performed on enslaved women -- all without consent and virtually none with anesthesia.
Modern 20th century medicine led to the Tuskegee syphilis experiments conducted by the U.S. Public Health Service. Researchers withheld treatment from some 400 African-American men from the 1930s well into the 1970s to observe how they reacted to the disease -- even though curative antibiotics had been around for decades. Only news reports ended the experiment.
The long-standing distrust of American healthcare in the African-American community is also baked into the care provided to sickle cell patients. Despite affecting one in 365 African-Americans, there is no disease registry to assist clinical trials, according to Mary Hulihan, a blood disorders epidemiologist with the Centers for Disease Control and Prevention. Edwards says many sufferers are suspicious of being monitored.
Meanwhile, only two drugs are available to alleviate the worst symptoms. The first one, hydroxyurea, received FDA approval only in 1998 -- nearly 90 years after the disease was first diagnosed. Moreover, Edwards says that some sufferers shy away from using hydroxyurea because it is also used to treat cancer. It's part of what he calls the "myth and folklore" in the African-American community about sickle cell disease.
Economics plays a role as well in the often-fragmented care such patients receive. According to CDC data, many patients rely extensively on public insurance programs such as Medicaid, whose coverage varies from state to state.
A Tough Transition
Edwards notes that sickle cell sufferers usually receive good care when they're children because of support provided by family members. But that often breaks down in adulthood. According to CDC data, an adult sickle cell patient visits a hospital emergency room three times as often as a child patient.
The consensus is that the path to a medical cure for sickle cell will first need to be smoothed over with a talk cure.
Modupe Idowu, a hematologist with the University of Texas Health system, estimates that there are perhaps a dozen comprehensive care centers for the estimated 100,000 sickle cell patients in the U.S., including the one she operates in Houston. That means a significant proportion of those afflicted are on their own to procure care.
And since many patients are on Medicaid, "a lot of hematologists that train to take care of blood disorders, many are not interested in treating [sickle cell disease] because the reimbursement for providers is not great," Idowu says.
Hsieh acknowledges that many of his patients can be suspicious about the care they are receiving. Frustration with fragmented care is usually the biggest driver, he adds.
Meanwhile, the skepticism that patients have about the treatments they seek is often reciprocated by their caregivers.
"The patients have experiences with medication and know what works at a very young age (for their pain)," Edwards says. Such expertise demonstrated by an African-American patient often leads to them being labeled as narcotics seekers.
The Correct Path
This all begs the question of how to deploy a cure. Idowu, who regularly holds town hall-style meetings with Houston-area patients, often must allay anxieties. For example, the gene therapy approach uses a harmless virus to transport new genetic material into cells. That virus happens to be a benign version of HIV, and convincing patients they won't be infected with HIV is a fraught issue.
The consensus is that the path to a medical cure for sickle cell will first need to be smoothed over with a talk cure.
Idowu tries to hammer home the fact that patients are afforded vastly more protections than in the past. "There are a lot of committees and investigational review boards that keep track of clinical trials; things just don't happen anymore as they did in the past," she says. She also believes it helps if more providers of color communicate to patients.
Hsieh is very straightforward with his patients. He informs them about the HIV vector but assures them no one has ever tested positive for the virus as a result of its use.
Edwards notes that since many patients suffer psychosocial trauma as a result of their chronic pain, there already is some counseling infrastructure in place to help them cope. He believes such resources will have to be stretched further as a cure looms closer.
In the absence of formal mental health services, straight talk may be the best way to overcome wariness.
"If patients have misgivings, we try our best to address them, and let them know at the end of the day it is their decision to make," Hsieh says. "And even the patients who have gone through the gene therapy and it didn't work well -- they're still glad they took the chance."
DNA- and RNA-based electronic implants may revolutionize healthcare
The test tubes contain tiny DNA/enzyme-based circuits, which comprise TRUMPET, a new type of electronic device, smaller than a cell.
Implantable electronic devices can significantly improve patients’ quality of life. A pacemaker can encourage the heart to beat more regularly. A neural implant, usually placed at the back of the skull, can help brain function and encourage higher neural activity. Current research on neural implants finds them helpful to patients with Parkinson’s disease, vision loss, hearing loss, and other nerve damage problems. Several of these implants, such as Elon Musk’s Neuralink, have already been approved by the FDA for human use.
Yet, pacemakers, neural implants, and other such electronic devices are not without problems. They require constant electricity, limited through batteries that need replacements. They also cause scarring. “The problem with doing this with electronics is that scar tissue forms,” explains Kate Adamala, an assistant professor of cell biology at the University of Minnesota Twin Cities. “Anytime you have something hard interacting with something soft [like muscle, skin, or tissue], the soft thing will scar. That's why there are no long-term neural implants right now.” To overcome these challenges, scientists are turning to biocomputing processes that use organic materials like DNA and RNA. Other promised benefits include “diagnostics and possibly therapeutic action, operating as nanorobots in living organisms,” writes Evgeny Katz, a professor of bioelectronics at Clarkson University, in his book DNA- And RNA-Based Computing Systems.
While a computer gives these inputs in binary code or "bits," such as a 0 or 1, biocomputing uses DNA strands as inputs, whether double or single-stranded, and often uses fluorescent RNA as an output.
Adamala’s research focuses on developing such biocomputing systems using DNA, RNA, proteins, and lipids. Using these molecules in the biocomputing systems allows the latter to be biocompatible with the human body, resulting in a natural healing process. In a recent Nature Communications study, Adamala and her team created a new biocomputing platform called TRUMPET (Transcriptional RNA Universal Multi-Purpose GatE PlaTform) which acts like a DNA-powered computer chip. “These biological systems can heal if you design them correctly,” adds Adamala. “So you can imagine a computer that will eventually heal itself.”
The basics of biocomputing
Biocomputing and regular computing have many similarities. Like regular computing, biocomputing works by running information through a series of gates, usually logic gates. A logic gate works as a fork in the road for an electronic circuit. The input will travel one way or another, giving two different outputs. An example logic gate is the AND gate, which has two inputs (A and B) and two different results. If both A and B are 1, the AND gate output will be 1. If only A is 1 and B is 0, the output will be 0 and vice versa. If both A and B are 0, the result will be 0. While a computer gives these inputs in binary code or "bits," such as a 0 or 1, biocomputing uses DNA strands as inputs, whether double or single-stranded, and often uses fluorescent RNA as an output. In this case, the DNA enters the logic gate as a single or double strand.
If the DNA is double-stranded, the system “digests” the DNA or destroys it, which results in non-fluorescence or “0” output. Conversely, if the DNA is single-stranded, it won’t be digested and instead will be copied by several enzymes in the biocomputing system, resulting in fluorescent RNA or a “1” output. And the output for this type of binary system can be expanded beyond fluorescence or not. For example, a “1” output might be the production of the enzyme insulin, while a “0” may be that no insulin is produced. “This kind of synergy between biology and computation is the essence of biocomputing,” says Stephanie Forrest, a professor and the director of the Biodesign Center for Biocomputing, Security and Society at Arizona State University.
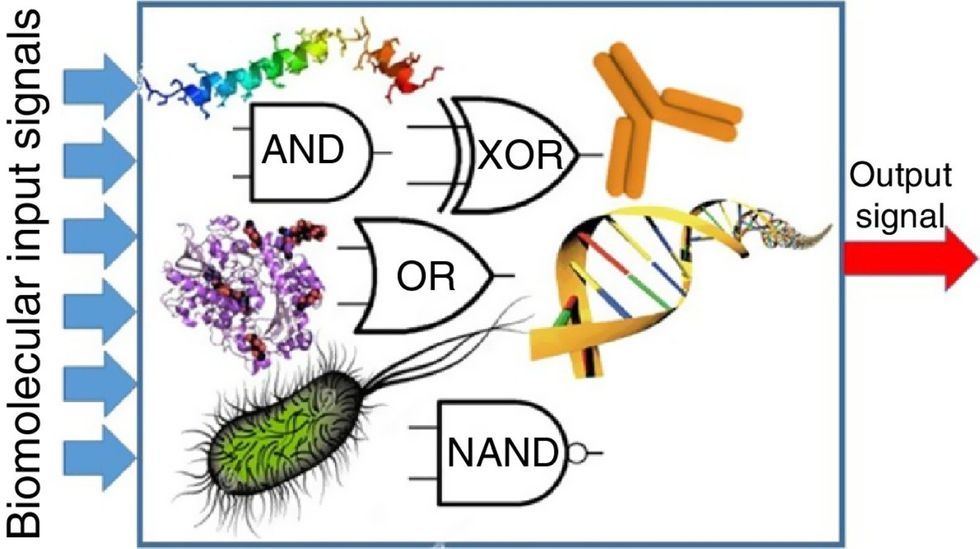
Biocomputing circles are made of DNA, RNA, proteins and even bacteria.
Evgeny Katz
The TRUMPET’s promise
Depending on whether the biocomputing system is placed directly inside a cell within the human body, or run in a test-tube, different environmental factors play a role. When an output is produced inside a cell, the cell's natural processes can amplify this output (for example, a specific protein or DNA strand), creating a solid signal. However, these cells can also be very leaky. “You want the cells to do the thing you ask them to do before they finish whatever their businesses, which is to grow, replicate, metabolize,” Adamala explains. “However, often the gate may be triggered without the right inputs, creating a false positive signal. So that's why natural logic gates are often leaky." While biocomputing outside a cell in a test tube can allow for tighter control over the logic gates, the outputs or signals cannot be amplified by a cell and are less potent.
TRUMPET, which is smaller than a cell, taps into both cellular and non-cellular biocomputing benefits. “At its core, it is a nonliving logic gate system,” Adamala states, “It's a DNA-based logic gate system. But because we use enzymes, and the readout is enzymatic [where an enzyme replicates the fluorescent RNA], we end up with signal amplification." This readout means that the output from the TRUMPET system, a fluorescent RNA strand, can be replicated by nearby enzymes in the platform, making the light signal stronger. "So it combines the best of both worlds,” Adamala adds.
These organic-based systems could detect cancer cells or low insulin levels inside a patient’s body.
The TRUMPET biocomputing process is relatively straightforward. “If the DNA [input] shows up as single-stranded, it will not be digested [by the logic gate], and you get this nice fluorescent output as the RNA is made from the single-stranded DNA, and that's a 1,” Adamala explains. "And if the DNA input is double-stranded, it gets digested by the enzymes in the logic gate, and there is no RNA created from the DNA, so there is no fluorescence, and the output is 0." On the story's leading image above, if the tube is "lit" with a purple color, that is a binary 1 signal for computing. If it's "off" it is a 0.
While still in research, TRUMPET and other biocomputing systems promise significant benefits to personalized healthcare and medicine. These organic-based systems could detect cancer cells or low insulin levels inside a patient’s body. The study’s lead author and graduate student Judee Sharon is already beginning to research TRUMPET's ability for earlier cancer diagnoses. Because the inputs for TRUMPET are single or double-stranded DNA, any mutated or cancerous DNA could theoretically be detected from the platform through the biocomputing process. Theoretically, devices like TRUMPET could be used to detect cancer and other diseases earlier.
Adamala sees TRUMPET not only as a detection system but also as a potential cancer drug delivery system. “Ideally, you would like the drug only to turn on when it senses the presence of a cancer cell. And that's how we use the logic gates, which work in response to inputs like cancerous DNA. Then the output can be the production of a small molecule or the release of a small molecule that can then go and kill what needs killing, in this case, a cancer cell. So we would like to develop applications that use this technology to control the logic gate response of a drug’s delivery to a cell.”
Although platforms like TRUMPET are making progress, a lot more work must be done before they can be used commercially. “The process of translating mechanisms and architecture from biology to computing and vice versa is still an art rather than a science,” says Forrest. “It requires deep computer science and biology knowledge,” she adds. “Some people have compared interdisciplinary science to fusion restaurants—not all combinations are successful, but when they are, the results are remarkable.”
Crickets are low on fat, high on protein, and can be farmed sustainably. They are also crunchy.
In today’s podcast episode, Leaps.org Deputy Editor Lina Zeldovich speaks about the health and ecological benefits of farming crickets for human consumption with Bicky Nguyen, who joins Lina from Vietnam. Bicky and her business partner Nam Dang operate an insect farm named CricketOne. Motivated by the idea of sustainable and healthy protein production, they started their unconventional endeavor a few years ago, despite numerous naysayers who didn’t believe that humans would ever consider munching on bugs.
Yet, making creepy crawlers part of our diet offers many health and planetary advantages. Food production needs to match the rise in global population, estimated to reach 10 billion by 2050. One challenge is that some of our current practices are inefficient, polluting and wasteful. According to nonprofit EarthSave.org, it takes 2,500 gallons of water, 12 pounds of grain, 35 pounds of topsoil and the energy equivalent of one gallon of gasoline to produce one pound of feedlot beef, although exact statistics vary between sources.
Meanwhile, insects are easy to grow, high on protein and low on fat. When roasted with salt, they make crunchy snacks. When chopped up, they transform into delicious pâtes, says Bicky, who invents her own cricket recipes and serves them at industry and public events. Maybe that’s why some research predicts that edible insects market may grow to almost $10 billion by 2030. Tune in for a delectable chat on this alternative and sustainable protein.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Further reading:
More info on Bicky Nguyen
https://yseali.fulbright.edu.vn/en/faculty/bicky-n...
The environmental footprint of beef production
https://www.earthsave.org/environment.htm
https://www.watercalculator.org/news/articles/beef-king-big-water-footprints/
https://www.frontiersin.org/articles/10.3389/fsufs.2019.00005/full
https://ourworldindata.org/carbon-footprint-food-methane
Insect farming as a source of sustainable protein
https://www.insectgourmet.com/insect-farming-growing-bugs-for-protein/
https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/insect-farming
Cricket flour is taking the world by storm
https://www.cricketflours.com/
https://talk-commerce.com/blog/what-brands-use-cricket-flour-and-why/

Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.

