A Star Surgeon Left a Trail of Dead Patients—and His Whistleblowers Were Punished

Dr. Paolo Macchiarini, then a professor of Regenerative Medicine at Karolinska Institute in Stockholm (Sweden), looks on during a plenary session at the Science of the Future international scientific conference, on September 17, 2014.
[Editor's Note: This is the first comprehensive account of the whistleblowers' side of a scandal that rocked the most hallowed halls in science – the same establishment that just last week awarded the Nobel Prize in Medicine. This still-unfolding saga is a cautionary tale about corruption, hype, and power that raises profound questions about how to uphold integrity in scientific research.]
When the world-famous Karolinska Institutet (KI) in Stockholm hired Dr. Paolo Macchiarini, he was considered a star surgeon and groundbreaking stem cell researcher. Handsome, charming and charismatic, Macchiarini was known as a trailblazer in a field that holds hope for curing a vast array of diseases.
It appeared that Macchiarini's miracle cure was working just as expected.
He claimed that he was regenerating human windpipes by seeding plastic scaffolds with stem cells from the patient's own bone marrow—a holy grail in medicine because the body will not reject its own cells. For patients who had trouble breathing due to advanced illness, a trachea made of their own cells would be a game-changer. Supposedly, the bone marrow cells repopulated the synthetic scaffolds with functioning, mucus-secreting epithelial cells, creating a new trachea that would become integrated into the patient's respiratory system as a living, breathing part. Macchiarini said as much in a dazzling presentation to his new colleagues at Karolinska, which is home to the Nobel Assembly – the body that has awarded the Nobel Prizes in Physiology or Medicine since 1901.
Karl-Henrik Grinnemo was a young cardiothoracic surgeon and researcher at Karolinska in 2010, when Macchiarini was hired. "He gave a fantastic presentation with lots of animation and everyone was impressed," Grinnemo says of his first encounter with Macchiarini. Grinnemo's own work focused on heart and aortic valve regeneration, also in the field of stem cell research. He and his colleagues were to help establish an interdisciplinary umbrella organization, under Macchiarini's leadership, called the Advanced Center for Translational Regenerative Medicine, which would aim to deliver cures from Karolinska's world-class laboratories to the bedsides of patients in desperate need.
Little did Grinnemo know that when KI hired Macchiarini, they had ignored a warning that the star surgeon had been accused of scientific misconduct by a colleague who had worked with him at the University of Florence. That blind eye would eventually cost three patients their lives in Sweden.
"A MIRACLE CURE"?
It has been said that if all you have is a hammer, everything looks like a nail, and it wasn't long before Macchiarini announced that he had a patient in dire need of one of the new artificial tracheas. The patient, a native of Eritrea who had emigrated to Iceland, had a slowly growing tumor on his trachea. Macchiarini had previously generated new windpipes from human donor tracheas outside of Sweden, but the Icelandic patient was the first to receive a synthetic trachea implant at Karolinska University Hospital. Macchiarini had already performed a similar procedure with decellularized donor tracheas on other patients around Europe, but not much was known at the time about their outcomes.
Of course, to justify a radical procedure such as removing a patient's trachea, one would need compelling evidence of effectiveness in animal studies, as well as an exhaustion of all other treatment alternatives. Macchiarini claimed that both conditions were met. He performed the implantation of the synthetic trachea as if he had received a hospital exemption. This is comparable to what the U.S. Food and Drug Administration classifies as "compassionate use," a procedure performed only in extreme circumstances, usually when the patient is terminal, and when no available alternative has worked.
Macchiarini personally invited Grinnemo to watch the all-day surgery, and, once the transplant was done after 10 grueling hours, Macchiarini asked him to close the patient. Then the 36-year-old man was transferred to another hospital, where Grinnemo and other attending physicians had little opportunity to follow his long-term recovery.
Two months later, Macchiarini approached Grinnemo with an invitation to be one of multiple co-authors on a paper about the case targeted for the New England Journal of Medicine. This was a huge opportunity for a junior researcher, and Grinnemo gladly agreed to write a one-month follow-up report on the Icelandic patient's clinical condition. He consulted the patient's medical records, which described a man with an infection in one lung but otherwise doing well, and wrote up his contribution. The patient had already been transferred back to Iceland by then and was home from the hospital. It appeared that Macchiarini's miracle cure was working just as expected.
But the ground was beginning to shake.
"We cannot find one word of evidence that points to regeneration induced by stem cells."
On September 2, 2011, three months after the Icelandic patient's surgery, a professor in Leuven, Belgium sent a written warning to KI's vice chancellor, Harriett Wallberg-Henriksson, stating that Macchiarini was guilty of prior research misconduct. This letter was forwarded to the new president at KI, professor Anders Hamsten, urging him to put a halt to more synthetic trachea implants. The accusations were grave.
Professor Pierre Delaere at Kathiolieke Universiteit asserted that synthetic tracheas coated with bone marrow cells did not, as Macchiarini had claimed, transform into living tracheas. He cited "countless" failures in animal experiments and called the outcome of Macchiarini's previous human surgeries "disastrous…half the patients died. The others are in a palliative setting….We cannot find one word of evidence that points to regeneration induced by stem cells."
Once again, KI simply ignored the warning, and Grinnemo and the 24 co-authors on the splashy academic paper about the latest surgery didn't even know about it. In the meantime, the New England Journal of Medicine rejected it for lacking a longer follow-up on the patients and missing data on how well the implants had integrated with the patient's respiratory system, so Macchiarini submitted it to The Lancet instead.
And he kept performing his experimental surgeries.
Soon there was a second transplant patient, a 30-year-old American man named Christopher Lyles. After his operation at KI, he returned to the U.S and the Swedish doctors were unable to follow his progress. Three months after his surgery, they learned that he had died at his home.

Paolo Macchiarini with Christopher Lyles, the American patient on whom he performed a trachea transplant in Stockholm in 2011. Lyles died a few months later.
Only four months after Lyles died, the third patient, a 22-year-old Turkish woman, received one of Macchiarini's grafts. In all three patients, Macchiarini had claimed that they were in dire straights—terminal if not for the hope of a trachea transplant, and he claimed a hospital exemption in all three cases. In fact, Grinnemo says, all three had been in stable condition before their surgeries—a reality Macchiarini did not share with his collaborators and co-authors on two academic papers about the surgeries that were subsequently published in The Lancet.
The Turkish woman's story is especially tragic. The young woman had initially undergone surgery elsewhere to fix an unrelated problem—hand sweating--but wound up with an accidentally damaged trachea that set her on a course of utter devastation. She sought help from Macchiarini, but his graft operation left her "living in hell," says Grinnemo. In intensive care afterward, her airways were producing so much mucus that they had to be cleared every four hours around the clock. The procedure "is like someone keeping your head under water every fourth hour until you almost suffocate to death. This is something that you wouldn't wish on your worst enemy," says Grinnemo.
By the spring of 2013, six months after Macchiarini's operation, the graft began to collapse. Several metal stents were inserted into her airways, but each one only worked for a short while. Macchiarini decided to remove the first plastic trachea and implant a new one. It seemed she couldn't get any worse, but after the second transplant, the young woman further deteriorated. Her airway secretions only increased; she had to undergo thousands of bronchoscopies, where an instrument was pushed down her throat into her lungs, and hundreds of surgeries during her three-year stint in the intensive care unit. Her body couldn't tolerate much more.
The whistleblowers realized that, despite Macchiarini's claims of successful operations in several now-published papers, the patients had been mutilated.
Grinnemo, together with fellow KI physicians Matthias Corbascio, Oscar Simonson and Thomas Fux, who were all involved in the care of the Turkish woman, became alarmed when the Icelandic patient came back to their hospital in the fall of 2013 with similar complaints. They realized that, despite Macchiarini's claims of successful operations in several now-published papers, the patients had been mutilated.
Both the Icelandic patient and the Turkish woman were too incapacitated to speak for themselves, so in the late fall of 2013, Grinnemo and his three concerned colleagues reached out to the patients' relatives seeking permission to review their medical records. It took weeks to receive the permissions, but once they did, what they found stunned them.
The Icelandic patient had developed fistulas (holes) between the artificial trachea and his esophagus, and had been fitted with several stents. Soon his esophagus also had to be removed, which Macchiarini was aware of. He should have reported these complications in the articles on which he was lead author, Grinnemo contends, and also should have informed his co-authors, each of whom had been responsible for writing up discrete sections of the papers. But Macchiarini had described each transplant as a success and had greatly exaggerated, if not outright lied, about how each patient had fared.
THE WHISTLEBLOWERS FIGHT BACK
Grinnemo and several other suspicious colleagues decided to launch an investigation. The result was a 500-page report identifying the synthetic tracheas as the problem and revealing that Macchiarini had falsified data and suppressed critical information in his reporting. He had even invented biopsies of the grafts, claiming that the marrow cells had populated them with functioning epithelial cells, while there was no real evidence of the patients' cells growing to line the tracheas.
The whistleblowers also discovered that Macchiarini had never received ethical clearance from Sweden's Human Ethical Review Board, nor had he gotten approval for his plastic tracheas from the Medical Product Agency, the Swedish counterpart to the FDA. He had relied entirely on his ability to do the surgeries under the hospital exemption, which he made everyone believe that he had obtained thanks to his star power.
What Macchiarini was doing, the investigators realized, was experimentation on living human subjects; he had circumvented the normal oversight protocols that exist to protect such subjects.
At a procedural meeting with his colleagues, including Dr. Ulf Lockowandt, the head of Karolinska University Hospital's Department of Cardiothoracic Surgery, Macchiarini dismissed the patients' complications as "manageable."
But among the large interdisciplinary team whose members had knowledge only of their own discrete specialties, doubts about Macchiarini's technique were festering. Complications in the patients only worsened when the tracheas inevitably began to collapse. There was a bursting open of sutures, holes in tissues adjacent to the implants, the disintegration of tissues that clogged bronchial passages. In far more than half of all the patients Macchiarini had operated on in several countries, patients died a lingering and agonizing death.
The last thing the whistleblowers expected was for the full weight of the institution to come crashing down against them.
When Grinnemo and his fellow investigators dug all this up, they decided they had to report it to the very top of Karolinska, to the institute's president, Anders Hamsten, so that he could stop Macchiarini from performing any further transplants. The last thing the whistleblowers expected was for the full weight of the institution to come crashing down against them.
"THEY WANTED TO SILENCE EVERYTHING"
KI had ample reason to sweep criticisms of Macchiarini under the rug. Up to 100 patients were about to be recruited for an international clinical study in which Macchiarini would do his implants—a nightmarish prospect considering his track record. But KI stood to receive millions of dollars in a government grant to conduct the study across Europe and Russia.
Still other incentives existed for KI to suppress Macchiarini's record. Plans were underway to establish a stem cell center in Hong Kong with over $45 million provided by a wealthy Chinese businessman. At the center, Macchiarini would be able to do his trachea transplants on patients in Asia. And in addition to the financial incentives to keep Macchiarini's brand associated with KI, many high-powered individuals were involved in his initial recruitment and didn't want their reputations tarnished, Grinnemo says. KI not only ignored the whistleblowers' allegations; punishment against them was swift and decisive.
On March 7, 2014, Grinnemo and the other whistleblowers met with Dr. Hamsten, in addition to two of Macchiarini's supervisors and the director of KI's Regenerative Network. They presented their findings and requested an official investigation by KI, including scrutiny of the now-six published research papers in which Macchiarini had claimed the success of his implants in humans. The whistleblowers also told the leadership about some rat studies Macchiarini had published in a prestigious journal that appeared to rely on falsified data.
Instead of the welcoming reception they expected, the room bristled with hostility. "I basically forced them to agree to an investigation," Grinnemo says, "but it was a very tough meeting. The feeling I got was that they wanted to silence everything and that they would continue to silence me and the other whistleblowers. We were already feeling the backlash."

From the left, whistleblowers Matthias Corbascio, Oscar Simonson, Thomas Fux and Karl-Henrik Grinnemo.
Previously, Grinnemo had confronted Macchiarini with questions about patients he had implanted in Russia prior to his stint at Karolinska. "Paolo Macchiarini realized we were onto something and he became very angry. He said he would do everything in his power to make my life miserable," Grinnemo recalls.
Macchiarini made good on his threat by filing a complaint about Grinnemo with the Swedish Research Council, the main funder of research in Sweden. At the time, Macchiarini and Grinnemo had jointly submitted a grant application on an aortic valve regeneration project, which the Council had approved. Macchiarini suddenly complained that Grinnemo had stolen his data on aortic valve regeneration, even though, unlike Grinnemo, Macchiarini was not a heart surgeon and had conducted no research on heart structures. In reality, all of the data had been generated by Grinnemo. The Council did a review and concluded that Grinnemo had not stolen the data, but Macchiarini spread rumors throughout KI that the young researcher was guilty of scientific misconduct. "He wanted to discredit me because he knew I was dangerous and he wanted to stop anyone from believing me," Grinnemo says.
In spite of the findings from the Council that he had committed no scientific misconduct, KI opened an investigation—not of Macchiarini, but of Grinnemo himself. It soon became clear that KI also wanted to discredit Grinnemo and to silence any possible rumors about Macchiarini's conduct. The whistleblowers continued to push forward, however, and over a period of several weeks they wrote to president Hamsten four times, asking that KI investigate the deadly transplants still being promoted by Macchiarini as some kind of miracle cure.
After four written requests, Hamsten replied that if the whistleblowers had concerns about Macchiarini, they should contact their supervisors or write a formal complaint. But the whistleblowers had already contacted several individuals in supervisory roles who had made it clear that they wanted nothing to do with the affair. It was obvious that KI would resist any investigation of Macchiarini and that no one, outside of the whistleblowers, wanted to take any responsibility for what could amount to a major scandal at one of the world's most powerful academic institutions.
The whistleblowers had another hostile and unproductive meeting with several doctors at KI with whom they shared a letter they had written to the journal Nature Communications, which published Macchiarini's article on rat experimentation, urging them to investigate whether he had falsified the data. Once again, the whistleblowers met with a wall of resistance. Grinnemo was now discredited because of the aortic valve grant application, the doctors reminded him, and no investigation or retraction of the Nature Communications article would be pursued.
In June 2014, KI made its retaliation against Grinnemo official by putting its legal counsel in charge of its investigation of his grant application. The university's ethical board then concluded that Grinnemo should have informed Macchiarini more clearly that he submitted the application to the Swedish Research Council and that he should have obtained a written acceptance from Macchiarini before proceeding with the application. KI could not find Grinnemo guilty of research misconduct, but accused him of "carelessness" regarding the usage of data—which was his own data all along.
A few years later, Grinnemo was totally cleared by both the Central Ethical Review Board and KI. However, the rumors surrounding the investigation and the finding that he hadn't "used data correctly" in a grant application had done their damage to his reputation. Since then, he has not received a single research grant. "You can't appeal the findings," Grinnemo says. "I don't know if I will ever get more research money. I'm totally dead."
The whistleblowers made multiple appeals to Dr. Lockowandt, the head of the Department of Cardiothoracic surgery, for an investigation into Macchiarini's implants, but they were stonewalled from the beginning. Lockowandt did nothing.
"The heads of departments at the KUH and KI didn't actually have that much power," Grinnemo explains. "Dr. Lockowandt thought he was fighting for his own career and position. He's basically a good person who decided to go the route of an administrator, and if you have conflicts with your superiors, your career will be over." In other words, a real investigation of Macchiarini's record could not happen with so much money and prestige riding on the continued presence of the star surgeon.
By August 11, 2014, the whistleblowers had made repeated requests of Dr. Hamsten for a meeting to present the data inconsistencies between Macchiarini's patients' medical records and what he had reported in numerous articles, all published in prestigious medical journals. When they finally received the answer—a cold instruction to submit a written notification to the heads of their departments—it was clear that KI was giving them the runaround.
But rather than simply ignore the whistleblowers, KI apparently decided to double down, trying to discredit them in an intimidation campaign.
KI even went so far as to force the chief medical officer of Karolinska University Hospital, Johan Bratt, to report the whistleblowers to Swedish police, claiming that they violated the law and the patients' privacy when they went through the patients´ charts and submitted their appeals for investigation to KI and the Central Ethical Review Board. KI claimed that their report revealed the identities of patients, even though they had been careful to anonymize all the information. The police interrogated several of the whistleblowers and concluded that they had done no wrong, but the incident made it clear how low KI would sink in its desire to harass them.
"You can't appeal the findings. I don't know if I will ever get more research money. I'm totally dead."
In private, Grinnemo's colleagues supported him, but feared coming forward out of the fear of losing their jobs. Grinnemo himself was in a tough spot. "I knew it would be difficult for me to do research but I hoped my position as a surgeon was secure," he says. "But after the New York Times article, I realized even that position was not as safe as I had thought."
THE MEDIA CATCHES ON -- WITH A PRICE
On November 24, 2014, The New York Times published a front-page story about Paolo Macchiarini based on the whistleblowers' investigation, which had leaked to the press. Officials at KI suspected one or more of the whistleblowers of being the leakers, but the publicity forced the top brass to at least appear to act. The next day they asked Dr. Bengt Gerdin, a professor of surgery at Sweden's Uppsala University, to do an investigation of Dr. Macchiarini. It's hard not to conclude that, after months of stonewalling on an institutional investigation, the Times article compelled them to do something. But KI still did not take any of the pressure off of Grinnemo and his three fellow whistleblowers.
One by one, each was informed that he would receive a formal warning from Dr. Lockowandt, the head of the cardiothoracic clinic, alleging that they had violated patient privacy by reading medical records. The whistleblowers countered that they had informed consents. They also asked for a meeting with Lockowandt and KI's attorneys, to which they brought a union representative and someone from the Swedish version of the American Medical Association. The union representative informed KI's attorneys that the doctors were actually required by law to consult a patient's medical records when the patient's life is in danger. Not doing so would have been a crime. Karolinska backed off on the formal warnings (which would have been the last step before actual termination) after that. But they found other ways to retaliate.
One whistleblower, Oscar Simonson, had been offered a residency at Karolinska University Hospital, but that offer was withdrawn without explanation. Grinnemo had expected to receive an advisor position in cardiothoracic surgery, but that promotion also evaporated. In addition, the number of surgeries he was tapped to perform was reduced and he was relegated to doing the "less popular" standard heart surgeries that began late in the afternoon and evenings.
The grinding day-to-day pressure on the whistleblowers never let up. On December 19, 2014, Dr. Lockowandt informed all four that they had been on the verge of being fired, but that hospital attorneys changed their minds at the last minute. By then not only were their reputations in tatters, but they had invested an estimated 10,000 hours of labor investigating Macchiarini's misconduct, appealing to KI, and defending themselves against KI's harassment.
When interviewed for this article, Grinnemo said, "I have never had a single day of vacation from this situation. In addition to dealing with it, I've been doing surgery and taking care of patients. I've had trouble sleeping, and it has affected my family. I haven't been able to focus on my family, and I feel guilty toward my kids." Of all the whistleblowers, Grinnemo seems to have received the brunt of the backlash.
KI was finally pushed to further action by yet more negative coverage of the Macchiarini affair in the media. In January 2015, Swedish National Television aired an exposé covering the Macchiarini surgeries and the desperate plight of the patients. In response, the Swedish public demanded that KI make a course correction. On February 19, KI withdrew all of its threats of formal warnings to the whistleblowers.
As the press event began, KI called the heads of the whistleblowers' departments to tell them to make sure the four didn't attend.
However, progress was incremental. On April 16, KI's ethical committee, which had done its own investigation, acquitted Macchiarini of allegations of scientific misconduct. This is the same university ethical board that had reprimanded Grinnemo over his usage of data in the aortic valve grant application.
The whistleblowers maintain that throughout the summer of 2015, KI was still far more focused on covering up the Macchiarini affair than on getting to the bottom of it. On May 13, the professor from Uppsala submitted the results of his independent investigation, in which he concluded that seven out of seven published articles in which Macchiarini was the lead author entailed the fabrication of data.
KI ignored the report. In August 2015, KI's president announced that Macchiarini had been cleared of all charges of scientific misconduct and that, magically, ethical approvals existed for the patient from Iceland. Macchiarini got a reprimand for being "a little sloppy" in his published descriptions of his patients. Then KI, eager to placate the public and salvage its reputation, held a press conference to announce the presumed innocence of its star surgeon.
As the press event began, KI called the heads of the whistleblowers' departments to tell them to make sure the four didn't attend, according to Grinnemo.
"They seemed to think we would come crashing in to the press conference and make a scene. It's ridiculous, but that's what they thought," says Grinnemo.
Around this time, KI asked that the whistleblowers compile and forward all of their correspondence with the independent investigator on the grounds that they were suspected of manipulating his investigation. The accusation went nowhere; the whistleblowers had barely spoken with him.
Then came a request from KI's IT department for the whistleblowers to compile and submit all of their emails for the preceding year. They were simply told that "an anonymous person" had made the request.
Throughout 2015, KI continued to go after the whistleblowers aggressively. That August, they were so discouraged that they felt they would never obtain any additional grants from the Swedish Research Council or any other funding organizations, and that their academic careers were over. To add insult to injury, a Swedish newspaper published an article defending Macchiarini and concluding that he was not guilty of violating the Helsinki Declaration, a statute put into effect after World War II protecting all humans from unauthorized medical experimentation.
THE TIDE TURNS, BUT REDEMPTION IS ELUSIVE
Then in November, they received a request from a Swedish filmmaker to be interviewed about the Macchiarini affair. Not knowing what angle the film was expected to take, they each put in hours in front of the camera. They wouldn't know the results of their interviews until January 2016, when the three-part documentary, "The Experiments," aired on Swedish television. The film documented the tortuous death of a Russian woman and the suffering of other patients who had received Macchiarini's implants.
That same month, a devastating article on Paolo Macchiarini was published in the American magazine Vanity Fair. Titled "The Celebrity Surgeon Who Used Love, Money and the Pope to Scam an NBC News Producer," the article revealed Macchiarini as an even more prolific fabulist and liar than anyone had remotely suspected. Not only did he fabricate data for multiple scientific papers, he had also lied about everything from his alleged medical training and celebrity connections to his personal relationship status.
Ironically, the woman who ultimately dismantled Macchiarini was Benita Alexander, a former producer for NBC News who was at one point engaged to marry him in a lavish ceremony that Macchiarini promised would be officiated by Pope Francis. Except that he didn't know the Pope, and he was already married to one woman and living with another.
Her story of heartbreak infuriated the public. The full list of people who had believed Macchiarini's almost countless fabrications may never be known—a tribute to his considerable personal charisma. But after the "The Experiments" and the Vanity Fair article, the public had had enough of Paolo Macchiarini. They demanded that KI's president step down and that Macchiarini be fired.

TV producer Benita Alexander appeared as a guest on Dr. Oz's show on February 14th, 2018 to discuss Dr. Macchiarini's deception. "He railroaded my life," she said.
In February 2016, there was a cascade of resignations and firings at KI. First, president Anders Hamsten stepped down. Then several top KI officials, including the General Secretary of the Nobel Assembly, the Dean of Research, and an advisor to KI's president, were either fired or stepped down. On March 3, several members of the board were replaced. The whistleblowers received an award for coming forward by an organization called Transparency International, but instead of heaving a sigh of relief, they only felt a continued sense of foreboding.
"We all felt very vulnerable because we knew that KI would retaliate in some way," says Grinnemo. A fellow whistleblower, Dr. Corbascio, gave an interview on a prime time news program saying that KI was a corrupt institution and should apologize to the patients' families and even pay them for their suffering. After that, both he and another colleague came under intensified scrutiny at work. They say that their supervisors, who were deeply involved in collaborations with Macchiarini, watched everything they did, apparently looking for a reason to fire them.
Grinnemo and Simonson both left KI to work for Uppsala University. But the lasting effects of the scandal followed them there. They still couldn't obtain any grants for new research, and other scientists at KI and elsewhere were unwilling to collaborate with them for fear of their own work being "tainted" by association.
On March 23, 2016, Paolo Macchiarini was finally sacked by KI. Still, the whistleblowers couldn't claim victory.
"Our aim," says Grinnemo, "was not to get him sacked but to stop the grafts, and we knew he would continue to do them in other countries. The clinical trial aiming to recruit 100 or so patients hadn't been halted. We tried to warn the Russian authorities and the EU grant office, and wanted them to stop the grant to Macchiarini. There was no response, so at that time we didn't know if the clinical trial would go forward."
Still, there was reason to hope. News of Macchiarini's scientific fraud, not to mention his personal debacle with Benita Alexander, had made its way around scientific circles in Germany and Britain, where a new investigation began.
Eventually, the entire board at Karolinska was replaced. Under its new president, the institute issued a decree this past summer finding the now thoroughly disgraced Macchiarini guilty of scientific misconduct, and concluding that six of his research papers should be retracted.
But in a cruelly ironic twist, KI took the whistleblowers' own investigation and turned it against them. KI's report found Grinnemo also guilty of scientific misconduct for apparently falling short in the care of the Icelandic patient, even though his role in the case had been minimal. It was like a punch in the gut, because the judgment cast Grinnemo as equally blameworthy to Macchiarini. It also failed to recognize that he had long ago not only withdrawn his name from the offending paper, but lobbied for years to have it retracted.
"This sends the message that whistleblowers in research will be punished. That's a serious problem."
The KI report also established the new category of "blameworthy" to describe two of the whistleblowers for their roles as co-authors in some of the papers. The whistleblowers did not receive a chance to respond to the new accusations before a decision was made to publicly reprimand them.
That decision can't be appealed.
Simonson told Science Magazine, "This sends the message that whistleblowers in research will be punished. That's a serious problem."
These days, Macchiarini is lying low but still publishing his supposed stem cell research, most recently on baboons. A paper published in March of this year in the Journal of Biomedical Materials lists his affiliation as Kazan Federal University in Russia, but in April 2017, the university fired him. He's rumored to be living in Italy and couldn't be reached for this article. He was investigated for criminal activity in Sweden and the case was closed without charges, but Grinnemo says that another prosecutor is now considering whether to bring charges against him for "aggravated manslaughter."
At KI, only Karin Dahlman Wright, who was the Institute's acting president during several months of these events, responded to a request for comment, but she claimed a near-total unawareness of the whistleblowers' narrative. Other officials there declined to be interviewed.
KI's clinical trial that was aiming to recruit new patients for biologically engineered tracheas is no longer happening. The European Commission posted on their research portal that the trial ended on March 31, 2017, stating: "Grant Agreement terminated."
As for Grinnemo, Simonson, Corbascio and Fux, they are still fighting for their careers. Grinnemo is currently suing KI for a chance to defend himself against its accusations of scientific misconduct. He's also claiming damages for lost grant funding, thousands of hours spent defending himself, and harm to his reputation. Whether he will prevail in court remains to be seen.
"KI did a very good job of destroying our careers," says Simonson. "They didn't do anything else well, but they did a very thorough job of that."
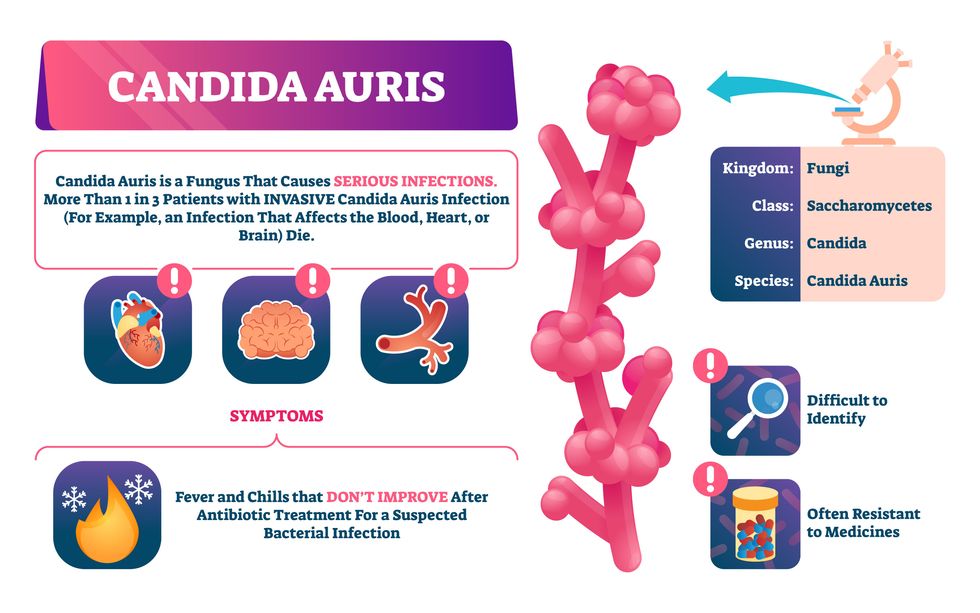
Doctors worry that fungal pathogens may cause the next pandemic.
Bacterial antibiotic resistance has been a concern in the medical field for several years. Now a new, similar threat is arising: drug-resistant fungal infections. The Centers for Disease Control and Prevention considers antifungal and antimicrobial resistance to be among the world’s greatest public health challenges.
One particular type of fungal infection caused by Candida auris is escalating rapidly throughout the world. And to make matters worse, C. auris is becoming increasingly resistant to current antifungal medications, which means that if you develop a C. auris infection, the drugs your doctor prescribes may not work. “We’re effectively out of medicines,” says Thomas Walsh, founding director of the Center for Innovative Therapeutics and Diagnostics, a translational research center dedicated to solving the antimicrobial resistance problem. Walsh spoke about the challenges at a Demy-Colton Virtual Salon, one in a series of interactive discussions among life science thought leaders.
Although C. auris typically doesn’t sicken healthy people, it afflicts immunocompromised hospital patients and may cause severe infections that can lead to sepsis, a life-threatening condition in which the overwhelmed immune system begins to attack the body’s own organs. Between 30 and 60 percent of patients who contract a C. auris infection die from it, according to the CDC. People who are undergoing stem cell transplants, have catheters or have taken antifungal or antibiotic medicines are at highest risk. “We’re coming to a perfect storm of increasing resistance rates, increasing numbers of immunosuppressed patients worldwide and a bug that is adapting to higher temperatures as the climate changes,” says Prabhavathi Fernandes, chair of the National BioDefense Science Board.
Most Candida species aren’t well-adapted to our body temperatures so they aren’t a threat. C. auris, however, thrives at human body temperatures.
Although medical professionals aren’t concerned at this point about C. auris evolving to affect healthy people, they worry that its presence in hospitals can turn routine surgeries into life-threatening calamities. “It’s coming,” says Fernandes. “It’s just a matter of time.”
An emerging global threat
“Fungi are found in the environment,” explains Fernandes, so Candida spores can easily wind up on people’s skin. In hospitals, they can be transferred from contact with healthcare workers or contaminated surfaces. Most Candida species aren’t well-adapted to our body temperatures so they aren’t a threat. C. auris, however, thrives at human body temperatures. It can enter the body during medical treatments that break the skin—and cause an infection. Overall, fungal infections cost some $48 billion in the U.S. each year. And infection rates are increasing because, in an ironic twist, advanced medical therapies are enabling severely ill patients to live longer and, therefore, be exposed to this pathogen.
The first-ever case of a C. auris infection was reported in Japan in 2009, although an analysis of Candida samples dated the earliest strain to a 1996 sample from South Korea. Since then, five separate varieties – called clades, which are similar to strains among bacteria – developed independently in different geographies: South Asia, East Asia, South Africa, South America and, recently, Iran. So far, C. auris infections have been reported in 35 countries.
In the U.S., the first infection was reported in 2016, and the CDC started tracking it nationally two years later. During that time, 5,654 cases have been reported to the CDC, which only tracks U.S. data.
What’s more notable than the number of cases is their rate of increase. In 2016, new cases increased by 175 percent and, on average, they have approximately doubled every year. From 2016 through 2022, the number of infections jumped from 63 to 2,377, a roughly 37-fold increase.
“This reminds me of what we saw with epidemics from 2013 through 2020… with Ebola, Zika and the COVID-19 pandemic,” says Robin Robinson, CEO of Spriovas and founding director of the Biomedical Advanced Research and Development Authority (BARDA), which is part of the U.S. Department of Health and Human Services. These epidemics started with a hockey stick trajectory, Robinson says—a gradual growth leading to a sharp spike, just like the shape of a hockey stick.
Another challenge is that right now medics don’t have rapid diagnostic tests for fungal infections. Currently, patients are often misdiagnosed because C. auris resembles several other easily treated fungi. Or they are diagnosed long after the infection begins and is harder to treat.
The problem is that existing diagnostics tests can only identify C. auris once it reaches the bloodstream. Yet, because this pathogen infects bodily tissues first, it should be possible to catch it much earlier before it becomes life-threatening. “We have to diagnose it before it reaches the bloodstream,” Walsh says.
The most alarming fact is that some Candida infections no longer respond to standard therapeutics.
“We need to focus on rapid diagnostic tests that do not rely on a positive blood culture,” says John Sperzel, president and CEO of T2 Biosystems, a company specializing in diagnostics solutions. Blood cultures typically take two to three days for the concentration of Candida to become large enough to detect. The company’s novel test detects about 90 percent of Candida species within three to five hours—thanks to its ability to spot minute quantities of the pathogen in blood samples instead of waiting for them to incubate and proliferate.
Unlike other Candida species C. auris thrives at human body temperatures
Adobe Stock
Tackling the resistance challenge
The most alarming fact is that some Candida infections no longer respond to standard therapeutics. The number of cases that stopped responding to echinocandin, the first-line therapy for most Candida infections, tripled in 2020, according to a study by the CDC.
Now, each of the first four clades shows varying levels of resistance to all three commonly prescribed classes of antifungal medications, such as azoles, echinocandins, and polyenes. For example, 97 percent of infections from C. auris Clade I are resistant to fluconazole, 54 percent to voriconazole and 30 percent of amphotericin. Nearly half are resistant to multiple antifungal drugs. Even with Clade II fungi, which has the least resistance of all the clades, 11 to 14 percent have become resistant to fluconazole.
Anti-fungal therapies typically target specific chemical compounds present on fungi’s cell membranes, but not on human cells—otherwise the medicine would cause damage to our own tissues. Fluconazole and other azole antifungals target a compound called ergosterol, preventing the fungal cells from replicating. Over the years, however, C. auris evolved to resist it, so existing fungal medications don’t work as well anymore.
A newer class of drugs called echinocandins targets a different part of the fungal cell. “The echinocandins – like caspofungin – inhibit (a part of the fungi) involved in making glucan, which is an essential component of the fungal cell wall and is not found in human cells,” Fernandes says. New antifungal treatments are needed, she adds, but there are only a few magic bullets that will hit just the fungus and not the human cells.
Research to fight infections also has been challenged by a lack of government support. That is changing now that BARDA is requesting proposals to develop novel antifungals. “The scope includes C. auris, as well as antifungals following a radiological/nuclear emergency, says BARDA spokesperson Elleen Kane.
The remaining challenge is the number of patients available to participate in clinical trials. Large numbers are needed, but the available patients are quite sick and often die before trials can be completed. Consequently, few biopharmaceutical companies are developing new treatments for C. auris.
ClinicalTrials.gov reports only two drugs in development for invasive C. auris infections—those than can spread throughout the body rather than localize in one particular area, like throat or vaginal infections: ibrexafungerp by Scynexis, Inc., fosmanogepix, by Pfizer.
Scynexis’ ibrexafungerp appears active against C. auris and other emerging, drug-resistant pathogens. The FDA recently approved it as a therapy for vaginal yeast infections and it is undergoing Phase III clinical trials against invasive candidiasis in an attempt to keep the infection from spreading.
“Ibreafungerp is structurally different from other echinocandins,” Fernandes says, because it targets a different part of the fungus. “We’re lucky it has activity against C. auris.”
Pfizer’s fosmanogepix is in Phase II clinical trials for patients with invasive fungal infections caused by multiple Candida species. Results are showing significantly better survival rates for people taking fosmanogepix.
Although C. auris does pose a serious threat to healthcare worldwide, scientists try to stay optimistic—because they recognized the problem early enough, they might have solutions in place before the perfect storm hits. “There is a bit of hope,” says Robinson. “BARDA has finally been able to fund the development of new antifungal agents and, hopefully, this year we can get several new classes of antifungals into development.”
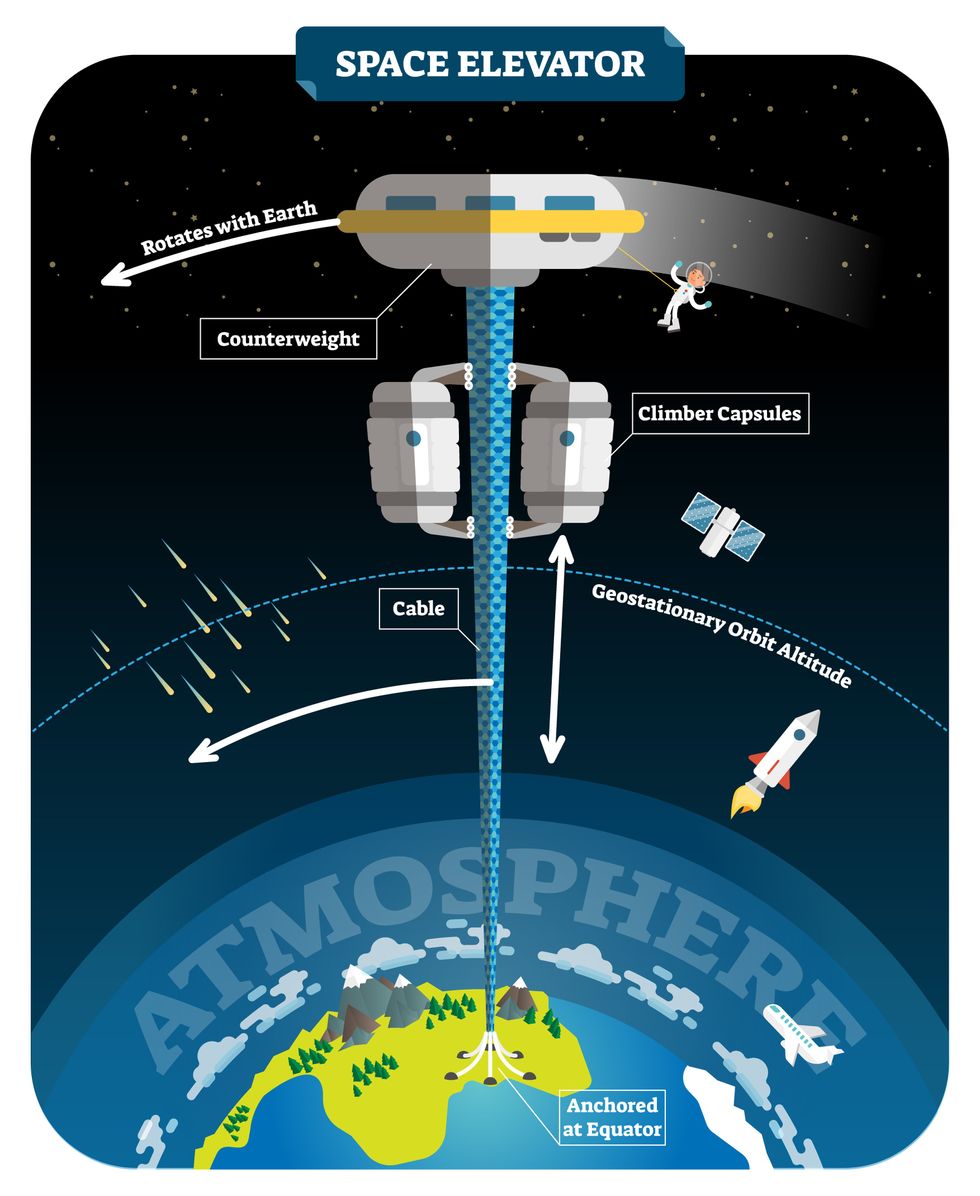
New elevators could lift up our access to space
A space elevator would be cheaper and cleaner than using rockets
Story by Big Think
When people first started exploring space in the 1960s, it cost upwards of $80,000 (adjusted for inflation) to put a single pound of payload into low-Earth orbit.
A major reason for this high cost was the need to build a new, expensive rocket for every launch. That really started to change when SpaceX began making cheap, reusable rockets, and today, the company is ferrying customer payloads to LEO at a price of just $1,300 per pound.
This is making space accessible to scientists, startups, and tourists who never could have afforded it previously, but the cheapest way to reach orbit might not be a rocket at all — it could be an elevator.
The space elevator
The seeds for a space elevator were first planted by Russian scientist Konstantin Tsiolkovsky in 1895, who, after visiting the 1,000-foot (305 m) Eiffel Tower, published a paper theorizing about the construction of a structure 22,000 miles (35,400 km) high.
This would provide access to geostationary orbit, an altitude where objects appear to remain fixed above Earth’s surface, but Tsiolkovsky conceded that no material could support the weight of such a tower.
We could then send electrically powered “climber” vehicles up and down the tether to deliver payloads to any Earth orbit.
In 1959, soon after Sputnik, Russian engineer Yuri N. Artsutanov proposed a way around this issue: instead of building a space elevator from the ground up, start at the top. More specifically, he suggested placing a satellite in geostationary orbit and dropping a tether from it down to Earth’s equator. As the tether descended, the satellite would ascend. Once attached to Earth’s surface, the tether would be kept taut, thanks to a combination of gravitational and centrifugal forces.
We could then send electrically powered “climber” vehicles up and down the tether to deliver payloads to any Earth orbit. According to physicist Bradley Edwards, who researched the concept for NASA about 20 years ago, it’d cost $10 billion and take 15 years to build a space elevator, but once operational, the cost of sending a payload to any Earth orbit could be as low as $100 per pound.
“Once you reduce the cost to almost a Fed-Ex kind of level, it opens the doors to lots of people, lots of countries, and lots of companies to get involved in space,” Edwards told Space.com in 2005.
In addition to the economic advantages, a space elevator would also be cleaner than using rockets — there’d be no burning of fuel, no harmful greenhouse emissions — and the new transport system wouldn’t contribute to the problem of space junk to the same degree that expendable rockets do.
So, why don’t we have one yet?
Tether troubles
Edwards wrote in his report for NASA that all of the technology needed to build a space elevator already existed except the material needed to build the tether, which needs to be light but also strong enough to withstand all the huge forces acting upon it.
The good news, according to the report, was that the perfect material — ultra-strong, ultra-tiny “nanotubes” of carbon — would be available in just two years.
“[S]teel is not strong enough, neither is Kevlar, carbon fiber, spider silk, or any other material other than carbon nanotubes,” wrote Edwards. “Fortunately for us, carbon nanotube research is extremely hot right now, and it is progressing quickly to commercial production.”Unfortunately, he misjudged how hard it would be to synthesize carbon nanotubes — to date, no one has been able to grow one longer than 21 inches (53 cm).
Further research into the material revealed that it tends to fray under extreme stress, too, meaning even if we could manufacture carbon nanotubes at the lengths needed, they’d be at risk of snapping, not only destroying the space elevator, but threatening lives on Earth.
Looking ahead
Carbon nanotubes might have been the early frontrunner as the tether material for space elevators, but there are other options, including graphene, an essentially two-dimensional form of carbon that is already easier to scale up than nanotubes (though still not easy).
Contrary to Edwards’ report, Johns Hopkins University researchers Sean Sun and Dan Popescu say Kevlar fibers could work — we would just need to constantly repair the tether, the same way the human body constantly repairs its tendons.
“Using sensors and artificially intelligent software, it would be possible to model the whole tether mathematically so as to predict when, where, and how the fibers would break,” the researchers wrote in Aeon in 2018.
“When they did, speedy robotic climbers patrolling up and down the tether would replace them, adjusting the rate of maintenance and repair as needed — mimicking the sensitivity of biological processes,” they continued.Astronomers from the University of Cambridge and Columbia University also think Kevlar could work for a space elevator — if we built it from the moon, rather than Earth.
They call their concept the Spaceline, and the idea is that a tether attached to the moon’s surface could extend toward Earth’s geostationary orbit, held taut by the pull of our planet’s gravity. We could then use rockets to deliver payloads — and potentially people — to solar-powered climber robots positioned at the end of this 200,000+ mile long tether. The bots could then travel up the line to the moon’s surface.
This wouldn’t eliminate the need for rockets to get into Earth’s orbit, but it would be a cheaper way to get to the moon. The forces acting on a lunar space elevator wouldn’t be as strong as one extending from Earth’s surface, either, according to the researchers, opening up more options for tether materials.
“[T]he necessary strength of the material is much lower than an Earth-based elevator — and thus it could be built from fibers that are already mass-produced … and relatively affordable,” they wrote in a paper shared on the preprint server arXiv.
After riding up the Earth-based space elevator, a capsule would fly to a space station attached to the tether of the moon-based one.
Electrically powered climber capsules could go up down the tether to deliver payloads to any Earth orbit.
Adobe Stock
Some Chinese researchers, meanwhile, aren’t giving up on the idea of using carbon nanotubes for a space elevator — in 2018, a team from Tsinghua University revealed that they’d developed nanotubes that they say are strong enough for a tether.
The researchers are still working on the issue of scaling up production, but in 2021, state-owned news outlet Xinhua released a video depicting an in-development concept, called “Sky Ladder,” that would consist of space elevators above Earth and the moon.
After riding up the Earth-based space elevator, a capsule would fly to a space station attached to the tether of the moon-based one. If the project could be pulled off — a huge if — China predicts Sky Ladder could cut the cost of sending people and goods to the moon by 96 percent.
The bottom line
In the 120 years since Tsiolkovsky looked at the Eiffel Tower and thought way bigger, tremendous progress has been made developing materials with the properties needed for a space elevator. At this point, it seems likely we could one day have a material that can be manufactured at the scale needed for a tether — but by the time that happens, the need for a space elevator may have evaporated.
Several aerospace companies are making progress with their own reusable rockets, and as those join the market with SpaceX, competition could cause launch prices to fall further.
California startup SpinLaunch, meanwhile, is developing a massive centrifuge to fling payloads into space, where much smaller rockets can propel them into orbit. If the company succeeds (another one of those big ifs), it says the system would slash the amount of fuel needed to reach orbit by 70 percent.
Even if SpinLaunch doesn’t get off the ground, several groups are developing environmentally friendly rocket fuels that produce far fewer (or no) harmful emissions. More work is needed to efficiently scale up their production, but overcoming that hurdle will likely be far easier than building a 22,000-mile (35,400-km) elevator to space.
This article originally appeared on Big Think, home of the brightest minds and biggest ideas of all time.