Advances Bring First True Hope to Spinal Cord Injury Patients

Jeff Marquis and Kelly Thomas, fellow research participants and spinal cord injury patients, in a rehab session.
Seven years ago, mountain biking near his home in Whitefish, Montana, Jeff Marquis felt confident enough to try for a jump he usually avoided. But he hesitated just a bit as he was going over. Instead of catching air, Marquis crashed.
Researchers' major new insight is that recovery is still possible, even years after an injury.
After 18 days on a ventilator in intensive care and two-and-a-half months in a rehabilitation hospital, Marquis was able to move his arms and wrists, but not his fingers or anything below his chest. Still, he was determined to remain as independent as possible. "I wasn't real interested in having people take care of me," says Marquis, now 35. So, he dedicated the energy he formerly spent biking, kayaking, and snowboarding toward recovering his own mobility.
For generations, those like Marquis with severe spinal cord injuries dreamt of standing and walking again – with no realistic hope of achieving these dreams. But now, a handful of people with such injuries, including Marquis, have stood on their own and begun to learn to take steps again. "I'm always trying to improve the situation but I'm happy with where I'm at," Marquis says.
The recovery Marquis and a few of his fellow patients have achieved proves that our decades-old understanding of the spinal cord was wrong. Researchers' major new insight is that recovery is still possible, even years after an injury. Only a few thousand nerve cells actually die when the spinal cord is injured. The other neurons still have the ability to generate signals and movement on their own, says Susan Harkema, co-principal investigator at the Kentucky Spinal Cord Injury Research Center, where Marquis is being treated.
"The spinal cord has much more responsibility for executing movement than we thought before," Harkema says. "Successful movement can happen without those connections from the brain." Nerve cell circuits remaining after the injury can control movement, she says, but leaving people sitting in a wheelchair doesn't activate those sensory circuits. "When you sit down, you lose all the sensory information. The whole circuitry starts discombobulating."
Harkema and others use a two-pronged approach – both physical rehabilitation and electrical stimulation – to get those spinal cord circuits back into a functioning state. Several research groups are still honing this approach, but a few patients have already taken steps under their own power, and others, like Marquis, can now stand unassisted – both of which were merely fantasies for spinal cord injury patients just five years ago.
"This really does represent a leap forward in terms of how we think about the capacity of the spinal cord to be repaired after injury," says Susan Howley, executive vice president for research for the Christopher & Dana Reeve Foundation, which supports research for spinal cord injuries.

Jeff Marquis biking on a rock before his accident.
This new biological understanding suggests the need for a wholesale change in how people are treated after a spinal cord injury, Howley says. But today, most insurance companies cover just 30-40 outpatient rehabilitation sessions per year, whether you've sprained your ankle or severed your spinal cord. To deliver the kind of therapy that really makes a difference for spinal cord injury patients requires "60-80-90 or 150 sessions," she says, adding that she thinks insurance companies will more than make up for the cost of those therapy sessions if spinal cord injury patients are healthier. Early evidence suggests that getting people back on their feet helps prevent medical problems common among paralyzed people, including urinary tract infections, which can require costly hospital stays.
"Exercise and the ability to fully bear one's own weight are as crucial for people who live with paralysis as they are for able-bodied people," Howley notes, adding that the Reeve Foundation is now trying to expand the network of facilities available in local communities to offer this essential rehabilitation.
"Providing the right kind of training every day to people could really improve their opportunity to recover," Harkema says.
It's not entirely clear yet how far someone could progress with rehabilitation alone, Harkema says, but probably the best results for someone with a severe injury will also require so-called epidural electrical stimulation. This device, implanted in the lower back for a cost of about $30,000, sends an electrical current at varying frequencies and intensities to the spinal cord. Several separate teams of researchers have now shown that epidural stimulation can help restore sensation and movement to people who have been paralyzed for years.
Epidural stimulation boosts the electrical signal that is generated below the point of injury, says Daniel Lu, an associate professor and vice chair of neurosurgery at the UCLA School of Medicine. Before a spinal cord injury, he says, a neuron might send a message at a volume of 10 but after injury, that volume might drop to a two or three. The epidural stimulation potentially trains the neuron to respond to the lower volume, Lu says.
Lu has used such stimulators to improve hand function – "essentially what defines us" – in two patients with spinal cord injuries. Both increased their grip strength so they now can lift a cup to drink by themselves, which they couldn't do before. He's also used non-invasive stimulation to help restore bladder function, which he says many spinal cord injury patients care about as much as walking again.
Not everyone will benefit from these treatments. People whose injury was caused by a cut to the spinal cord, as with a knife or bullet, probably can't be helped, Lu says, adding that they account for less than 5 percent of spinal cord injuries.
The current challenge Lu says is not how to stimulate the spinal cord, but where to stimulate it and the frequency of stimulation that will be most effective for each patient. Right now, doctors use an off-the-shelf stimulator that is used to treat pain and is not optimized for spinal cord patients, Harkema says.
Swiss researchers have shown impressive results from intermittent rather than continuous epidural stimulation. These pulses better reflect the way the brain sends its messages, according to Gregoire Courtine, the senior author on a pair of papers published Nov. 1 in Nature and Nature Neuroscience. He showed that he could get people up and moving within just a few days of turning on the stimulation. Three of his patients are walking again with only a walker or minimal assistance, and they also gained voluntary leg movements even when the stimulator was off. Continuous stimulation, this research shows, actually interferes with the patients' perception of limb position, and thus makes it harder for them to relearn to walk.
Even short of walking, proper physical rehabilitation and electrical stimulation can transform the quality of life of people with spinal cord injury, Howley and Harkema say. Patients don't need to be able to reach the top shelf or run a marathon to feel like they've been "cured" from their paralysis. Instead, recovering bowel, bladder and sexual functions, the ability to regulate their temperature and blood pressure, and reducing the breakdown of skin that can lead to a life-threatening infection can all be transformative – and all appear to improve with the combination of rehabilitation and electrical stimulation.
Howley cites a video of one of Harkema's patients, Stefanie Putnam, who was passing out five to six times a day because her blood pressure was so low. She couldn't be left alone, which meant she had no independence. After several months of rehabilitation and stimulation, she can now sit up for long periods, be left alone, and even, she says gleefully, cook her own dinner. "Every time I watch it, it brings me to tears," Howley says of the video. "She's able to resume her normal life activity. It's mind-boggling."
The work also suggests a transformation in the care of people immediately after injury. They should be allowed to stand and start taking steps as soon as possible, even if they cannot do it under their own power, Harkema says. Research is also likely to show that quickly implanting a stimulator after an injury will make a difference, she says.
There may be medications that can help immediately after an injury, too. One drug currently being studied, called riluzole, has already been approved for ALS and might help limit the damage of a spinal cord injury, Howley says. But testing its effectiveness has been a slow process, she says, because it needs to be given within 12 hours of the initial injury and not enough people get to the testing sites in time.
Stem cell therapy also offers promise for spinal cord injury patients, Howley says – but not the treatments currently provided by commercial stem cell clinics both in the U.S. and overseas, which she says are a sham. Instead, she is carefully following research by a California-based company called Asterias Biotherapeutics, which announced plans Nov. 8 to merge with a company called BioTime.
Asterias and a predecessor company have been treating people since 2010 in an effort to regrow nerves in the spinal cord. All those treated have safely tolerated the cells, but not everyone has seen a huge improvement, says Edward Wirth, who has led the trial work and is Asterias' chief medical director. He says he thinks he knows what's held back those who didn't improve much, and hopes to address those issues in the next 3- to 4-year-long trial, which he's now discussing with the U.S. Food and Drug Administration.
So far, he says, some patients have had an almost complete return of movement in their hands and arms, but little improvement in their legs. The stem cells seem to stimulate tissue repair and regeneration, he says, but only around the level of the injury in the spinal cord and a bit below. The legs, he says, are too far away to benefit.
Wirth says he thinks a combination of treatments – stem cells, electrical stimulation, rehabilitation, and improved care immediately after an injury – will likely produce the best results.
While there's still a long way to go to scale these advances to help the majority of the 300,000 spinal cord injury patients in the U.S., they now have something that's long been elusive: hope.
"Two or three decades ago there was no hope at all," Howley says. "We've come a long way."
The future of non-hormonal birth control: Antibodies can stop sperm in their tracks
Many women want non-hormonal birth control. A 22-year-old's findings were used to launch a company that could, within the decade, bring a new kind of contraceptive to the marketplace.
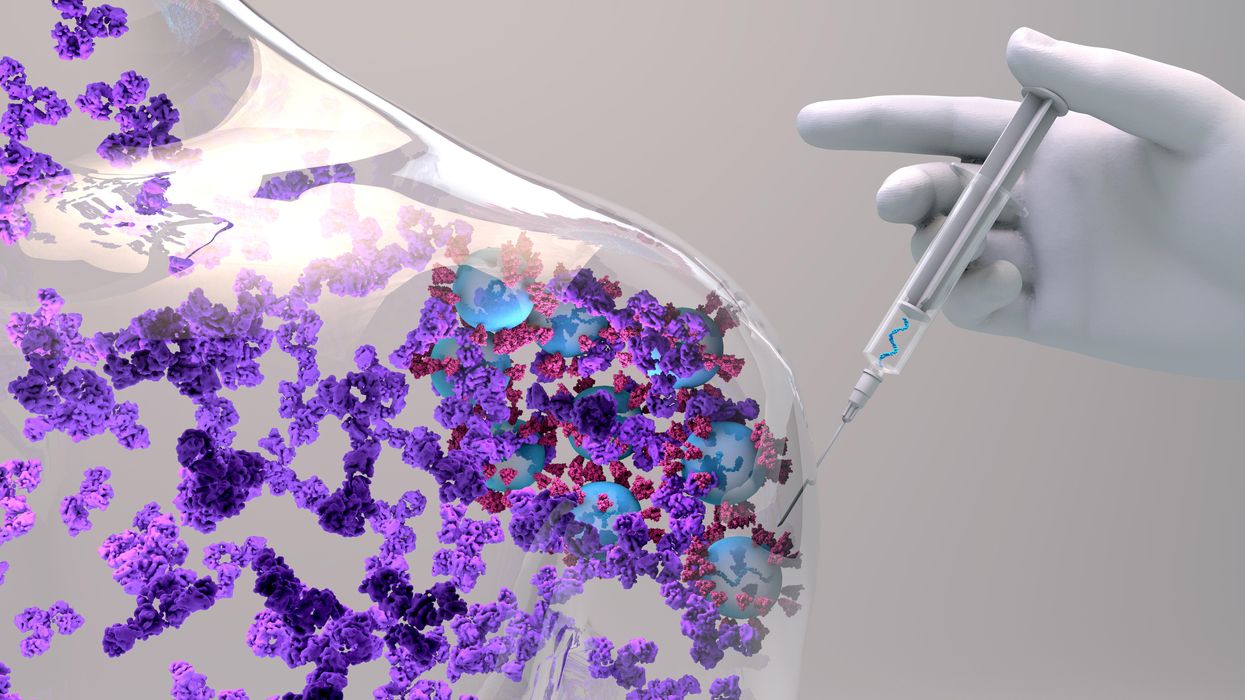
Unwanted pregnancy can now be added to the list of preventions that antibodies may be fighting in the near future. For decades, really since the 1980s, engineered monoclonal antibodies have been knocking out invading germs — preventing everything from cancer to COVID. Sperm, which have some of the same properties as germs, may be next.
Not only is there an unmet need on the market for alternatives to hormonal contraceptives, the genesis for the original research was personal for the then 22-year-old scientist who led it. Her findings were used to launch a company that could, within the decade, bring a new kind of contraceptive to the marketplace.
The genesis
It’s Suruchi Shrestha’s research — published in Science Translational Medicine in August 2021 and conducted as part of her dissertation while she was a graduate student at the University of North Carolina at Chapel Hill — that could change the future of contraception for many women worldwide. According to a Guttmacher Institute report, in the U.S. alone, there were 46 million sexually active women of reproductive age (15–49) who did not want to get pregnant in 2018. With the overturning of Roe v. Wade this year, Shrestha’s research could, indeed, be life changing for millions of American women and their families.
Now a scientist with NextVivo, Shrestha is not directly involved in the development of the contraceptive that is based on her research. But, back in 2016 when she was going through her own problems with hormonal contraceptives, she “was very personally invested” in her research project, Shrestha says. She was coping with a long list of negative effects from an implanted hormonal IUD. According to the Mayo Clinic, those can include severe pelvic pain, headaches, acute acne, breast tenderness, irregular bleeding and mood swings. After a year, she had the IUD removed, but it took another full year before all the side effects finally subsided; she also watched her sister suffer the “same tribulations” after trying a hormonal IUD, she says.
For contraceptive use either daily or monthly, Shrestha says, “You want the antibody to be very potent and also cheap.” That was her goal when she launched her study.
Shrestha unshelved antibody research that had been sitting idle for decades. It was in the late 80s that scientists in Japan first tried to develop anti-sperm antibodies for contraceptive use. But, 35 years ago, “Antibody production had not been streamlined as it is now, so antibodies were very expensive,” Shrestha explains. So, they shifted away from birth control, opting to focus on developing antibodies for vaccines.
Over the course of the last three decades, different teams of researchers have been working to make the antibody more effective, bringing the cost down, though it’s still expensive, according to Shrestha. For contraceptive use either daily or monthly, she says, “You want the antibody to be very potent and also cheap.” That was her goal when she launched her study.
The problem
The problem with contraceptives for women, Shrestha says, is that all but a few of them are hormone-based or have other negative side effects. In fact, some studies and reports show that millions of women risk unintended pregnancy because of medical contraindications with hormone-based contraceptives or to avoid the risks and side effects. While there are about a dozen contraceptive choices for women, there are two for men: the condom, considered 98% effective if used correctly, and vasectomy, 99% effective. Neither of these choices are hormone-based.
On the non-hormonal side for women, there is the diaphragm which is considered only 87 percent effective. It works better with the addition of spermicides — Nonoxynol-9, or N-9 — however, they are detergents; they not only kill the sperm, they also erode the vaginal epithelium. And, there’s the non-hormonal IUD which is 99% effective. However, the IUD needs to be inserted by a medical professional, and it has a number of negative side effects, including painful cramping at a higher frequency and extremely heavy or “abnormal” and unpredictable menstrual flows.
The hormonal version of the IUD, also considered 99% effective, is the one Shrestha used which caused her two years of pain. Of course, there’s the pill, which needs to be taken daily, and the birth control ring which is worn 24/7. Both cause side effects similar to the other hormonal contraceptives on the market. The ring is considered 93% effective mostly because of user error; the pill is considered 99% effective if taken correctly.
“That’s where we saw this opening or gap for women. We want a safe, non-hormonal contraceptive,” Shrestha says. Compounding the lack of good choices, is poor access to quality sex education and family planning information, according to the non-profit Urban Institute. A focus group survey suggested that the sex education women received “often lacked substance, leaving them feeling unprepared to make smart decisions about their sexual health and safety,” wrote the authors of the Urban Institute report. In fact, nearly half (45%, or 2.8 million) of the pregnancies that occur each year in the US are unintended, reports the Guttmacher Institute. Globally the numbers are similar. According to a new report by the United Nations, each year there are 121 million unintended pregnancies, worldwide.
The science
The early work on antibodies as a contraceptive had been inspired by women with infertility. It turns out that 9 to 12 percent of women who are treated for infertility have antibodies that develop naturally and work against sperm. Shrestha was encouraged that the antibodies were specific to the target — sperm — and therefore “very safe to use in women.” She aimed to make the antibodies more stable, more effective and less expensive so they could be more easily manufactured.
Since antibodies tend to stick to things that you tell them to stick to, the idea was, basically, to engineer antibodies to stick to sperm so they would stop swimming. Shrestha and her colleagues took the binding arm of an antibody that they’d isolated from an infertile woman. Then, targeting a unique surface antigen present on human sperm, they engineered a panel of antibodies with as many as six to 10 binding arms — “almost like tongs with prongs on the tongs, that bind the sperm,” explains Shrestha. “We decided to add those grabbers on top of it, behind it. So it went from having two prongs to almost 10. And the whole goal was to have so many arms binding the sperm that it clumps it” into a “dollop,” explains Shrestha, who earned a patent on her research.

Suruchi Shrestha works in the lab with a colleague. In 2016, her research on antibodies for birth control was inspired by her own experience with side effects from an implanted hormonal IUD.
UNC - Chapel Hill
The sperm stays right where it met the antibody, never reaching the egg for fertilization. Eventually, and naturally, “Our vaginal system will just flush it out,” Shrestha explains.
“She showed in her early studies that [she] definitely got the sperm immotile, so they didn't move. And that was a really promising start,” says Jasmine Edelstein, a scientist with an expertise in antibody engineering who was not involved in this research. Shrestha’s team at UNC reproduced the effect in the sheep, notes Edelstein, who works at the startup Be Biopharma. In fact, Shrestha’s anti-sperm antibodies that caused the sperm to agglutinate, or clump together, were 99.9% effective when delivered topically to the sheep’s reproductive tracts.
The future
Going forward, Shrestha thinks the ideal approach would be delivering the antibodies through a vaginal ring. “We want to use it at the source of the spark,” Shrestha says, as opposed to less direct methods, such as taking a pill. The ring would dissolve after one month, she explains, “and then you get another one.”
Engineered to have a long shelf life, the anti-sperm antibody ring could be purchased without a prescription, and women could insert it themselves, without a doctor. “That's our hope, so that it is accessible,” Shrestha says. “Anybody can just go and grab it and not worry about pregnancy or unintended pregnancy.”
Her patented research has been licensed by several biotech companies for clinical trials. A number of Shrestha’s co-authors, including her lab advisor, Sam Lai, have launched a company, Mucommune, to continue developing the contraceptives based on these antibodies.
And, results from a small clinical trial run by researchers at Boston University Chobanian & Avedisian School of Medicine show that a dissolvable vaginal film with antibodies was safe when tested on healthy women of reproductive age. That same group of researchers earlier this year received a $7.2 million grant from the National Institute of Health for further research on monoclonal antibody-based contraceptives, which have also been shown to block transmission of viruses, like HIV.
“As the costs come down, this becomes a more realistic option potentially for women,” says Edelstein. “The impact could be tremendous.”
The Friday Five: An mRNA vaccine works against cancer, new research suggests
In this week's Friday Five, an mRNA vaccine works against cancer for the first time. Plus, these cameras inside the body have an unusual source of power, a new theory for what causes aging, bacteria that could get you excited to work out, and a reason for sex differences in Alzheimer's.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Here are the promising studies covered in this week's Friday Five:
- An mRNA vaccine that works against cancer
- These cameras inside the body have an unusual source of power
- A new theory for what causes aging
- Can bacteria make you excited to work out?
- Why women get Alzheimer's more often than men