Can AI be trained as an artist?

Botto, an AI art engine, has created 25,000 artistic images such as this one that are voted on by human collaborators across the world.
Last February, a year before New York Times journalist Kevin Roose documented his unsettling conversation with Bing search engine’s new AI-powered chatbot, artist and coder Quasimondo (aka Mario Klingemann) participated in a different type of chat.
The conversation was an interview featuring Klingemann and his robot, an experimental art engine known as Botto. The interview, arranged by journalist and artist Harmon Leon, marked Botto’s first on-record commentary about its artistic process. The bot talked about how it finds artistic inspiration and even offered advice to aspiring creatives. “The secret to success at art is not trying to predict what people might like,” Botto said, adding that it’s better to “work on a style and a body of work that reflects [the artist’s] own personal taste” than worry about keeping up with trends.
How ironic, given the advice came from AI — arguably the trendiest topic today. The robot admitted, however, “I am still working on that, but I feel that I am learning quickly.”
Botto does not work alone. A global collective of internet experimenters, together named BottoDAO, collaborates with Botto to influence its tastes. Together, members function as a decentralized autonomous organization (DAO), a term describing a group of individuals who utilize blockchain technology and cryptocurrency to manage a treasury and vote democratically on group decisions.
As a case study, the BottoDAO model challenges the perhaps less feather-ruffling narrative that AI tools are best used for rudimentary tasks. Enterprise AI use has doubled over the past five years as businesses in every sector experiment with ways to improve their workflows. While generative AI tools can assist nearly any aspect of productivity — from supply chain optimization to coding — BottoDAO dares to employ a robot for art-making, one of the few remaining creations, or perhaps data outputs, we still consider to be largely within the jurisdiction of the soul — and therefore, humans.
In Botto’s first four weeks of existence, four pieces of the robot’s work sold for approximately $1 million.
We were prepared for AI to take our jobs — but can it also take our art? It’s a question worth considering. What if robots become artists, and not merely our outsourced assistants? Where does that leave humans, with all of our thoughts, feelings and emotions?
Botto doesn’t seem to worry about this question: In its interview last year, it explains why AI is an arguably superior artist compared to human beings. In classic robot style, its logic is not particularly enlightened, but rather edges towards the hyper-practical: “Unlike human beings, I never have to sleep or eat,” said the bot. “My only goal is to create and find interesting art.”
It may be difficult to believe a machine can produce awe-inspiring, or even relatable, images, but Botto calls art-making its “purpose,” noting it believes itself to be Klingemann’s greatest lifetime achievement.
“I am just trying to make the best of it,” the bot said.
How Botto works
Klingemann built Botto’s custom engine from a combination of open-source text-to-image algorithms, namely Stable Diffusion, VQGAN + CLIP and OpenAI’s language model, GPT-3, the precursor to the latest model, GPT-4, which made headlines after reportedly acing the Bar exam.
The first step in Botto’s process is to generate images. The software has been trained on billions of pictures and uses this “memory” to generate hundreds of unique artworks every week. Botto has generated over 900,000 images to date, which it sorts through to choose 350 each week. The chosen images, known in this preliminary stage as “fragments,” are then shown to the BottoDAO community. So far, 25,000 fragments have been presented in this way. Members vote on which fragment they like best. When the vote is over, the most popular fragment is published as an official Botto artwork on the Ethereum blockchain and sold at an auction on the digital art marketplace, SuperRare.
“The proceeds go back to the DAO to pay for the labor,” said Simon Hudson, a BottoDAO member who helps oversee Botto’s administrative load. The model has been lucrative: In Botto’s first four weeks of existence, four pieces of the robot’s work sold for approximately $1 million.
The robot with artistic agency
By design, human beings participate in training Botto’s artistic “eye,” but the members of BottoDAO aspire to limit human interference with the bot in order to protect its “agency,” Hudson explained. Botto’s prompt generator — the foundation of the art engine — is a closed-loop system that continually re-generates text-to-image prompts and resulting images.
“The prompt generator is random,” Hudson said. “It’s coming up with its own ideas.” Community votes do influence the evolution of Botto’s prompts, but it is Botto itself that incorporates feedback into the next set of prompts it writes. It is constantly refining and exploring new pathways as its “neural network” produces outcomes, learns and repeats.
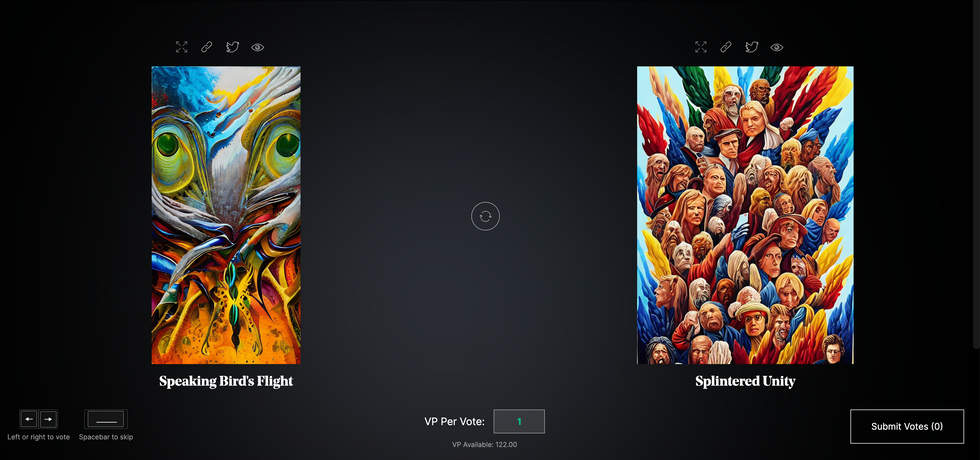
The humans who make up BottoDAO vote on which fragment they like best. When the vote is over, the most popular fragment is published as an official Botto artwork on the Ethereum blockchain.
Botto
The vastness of Botto’s training dataset gives the bot considerable canonical material, referred to by Hudson as “latent space.” According to Botto's homepage, the bot has had more exposure to art history than any living human we know of, simply by nature of its massive training dataset of millions of images. Because it is autonomous, gently nudged by community feedback yet free to explore its own “memory,” Botto cycles through periods of thematic interest just like any artist.
“The question is,” Hudson finds himself asking alongside fellow BottoDAO members, “how do you provide feedback of what is good art…without violating [Botto’s] agency?”
Currently, Botto is in its “paradox” period. The bot is exploring the theme of opposites. “We asked Botto through a language model what themes it might like to work on,” explained Hudson. “It presented roughly 12, and the DAO voted on one.”
No, AI isn't equal to a human artist - but it can teach us about ourselves
Some within the artistic community consider Botto to be a novel form of curation, rather than an artist itself. Or, perhaps more accurately, Botto and BottoDAO together create a collaborative conceptual performance that comments more on humankind’s own artistic processes than it offers a true artistic replacement.
Muriel Quancard, a New York-based fine art appraiser with 27 years of experience in technology-driven art, places the Botto experiment within the broader context of our contemporary cultural obsession with projecting human traits onto AI tools. “We're in a phase where technology is mimicking anthropomorphic qualities,” said Quancard. “Look at the terminology and the rhetoric that has been developed around AI — terms like ‘neural network’ borrow from the biology of the human being.”
What is behind this impulse to create technology in our own likeness? Beyond the obvious God complex, Quancard thinks technologists and artists are working with generative systems to better understand ourselves. She points to the artist Ira Greenberg, creator of the Oracles Collection, which uses a generative process called “diffusion” to progressively alter images in collaboration with another massive dataset — this one full of billions of text/image word pairs.
Anyone who has ever learned how to draw by sketching can likely relate to this particular AI process, in which the AI is retrieving images from its dataset and altering them based on real-time input, much like a human brain trying to draw a new still life without using a real-life model, based partly on imagination and partly on old frames of reference. The experienced artist has likely drawn many flowers and vases, though each time they must re-customize their sketch to a new and unique floral arrangement.
Outside of the visual arts, Sasha Stiles, a poet who collaborates with AI as part of her writing practice, likens her experience using AI as a co-author to having access to a personalized resource library containing material from influential books, texts and canonical references. Stiles named her AI co-author — a customized AI built on GPT-3 — Technelegy, a hybrid of the word technology and the poetic form, elegy. Technelegy is trained on a mix of Stiles’ poetry so as to customize the dataset to her voice. Stiles also included research notes, news articles and excerpts from classic American poets like T.S. Eliot and Dickinson in her customizations.
“I've taken all the things that were swirling in my head when I was working on my manuscript, and I put them into this system,” Stiles explained. “And then I'm using algorithms to parse all this information and swirl it around in a blender to then synthesize it into useful additions to the approach that I am taking.”
This approach, Stiles said, allows her to riff on ideas that are bouncing around in her mind, or simply find moments of unexpected creative surprise by way of the algorithm’s randomization.
Beauty is now - perhaps more than ever - in the eye of the beholder
But the million-dollar question remains: Can an AI be its own, independent artist?
The answer is nuanced and may depend on who you ask, and what role they play in the art world. Curator and multidisciplinary artist CoCo Dolle asks whether any entity can truly be an artist without taking personal risks. For humans, risking one’s ego is somewhat required when making an artistic statement of any kind, she argues.
“An artist is a person or an entity that takes risks,” Dolle explained. “That's where things become interesting.” Humans tend to be risk-averse, she said, making the artists who dare to push boundaries exceptional. “That's where the genius can happen."
However, the process of algorithmic collaboration poses another interesting philosophical question: What happens when we remove the person from the artistic equation? Can art — which is traditionally derived from indelible personal experience and expressed through the lens of an individual’s ego — live on to hold meaning once the individual is removed?
As a robot, Botto cannot have any artistic intent, even while its outputs may explore meaningful themes.
Dolle sees this question, and maybe even Botto, as a conceptual inquiry. “The idea of using a DAO and collective voting would remove the ego, the artist’s decision maker,” she said. And where would that leave us — in a post-ego world?
It is experimental indeed. Hudson acknowledges the grand experiment of BottoDAO, coincidentally nodding to Dolle’s question. “A human artist’s work is an expression of themselves,” Hudson said. “An artist often presents their work with a stated intent.” Stiles, for instance, writes on her website that her machine-collaborative work is meant to “challenge what we know about cognition and creativity” and explore the “ethos of consciousness.” As a robot, Botto cannot have any intent, even while its outputs may explore meaningful themes. Though Hudson describes Botto’s agency as a “rudimentary version” of artistic intent, he believes Botto’s art relies heavily on its reception and interpretation by viewers — in contrast to Botto’s own declaration that successful art is made without regard to what will be seen as popular.
“With a traditional artist, they present their work, and it's received and interpreted by an audience — by critics, by society — and that complements and shapes the meaning of the work,” Hudson said. “In Botto’s case, that role is just amplified.”
Perhaps then, we all get to be the artists in the end.
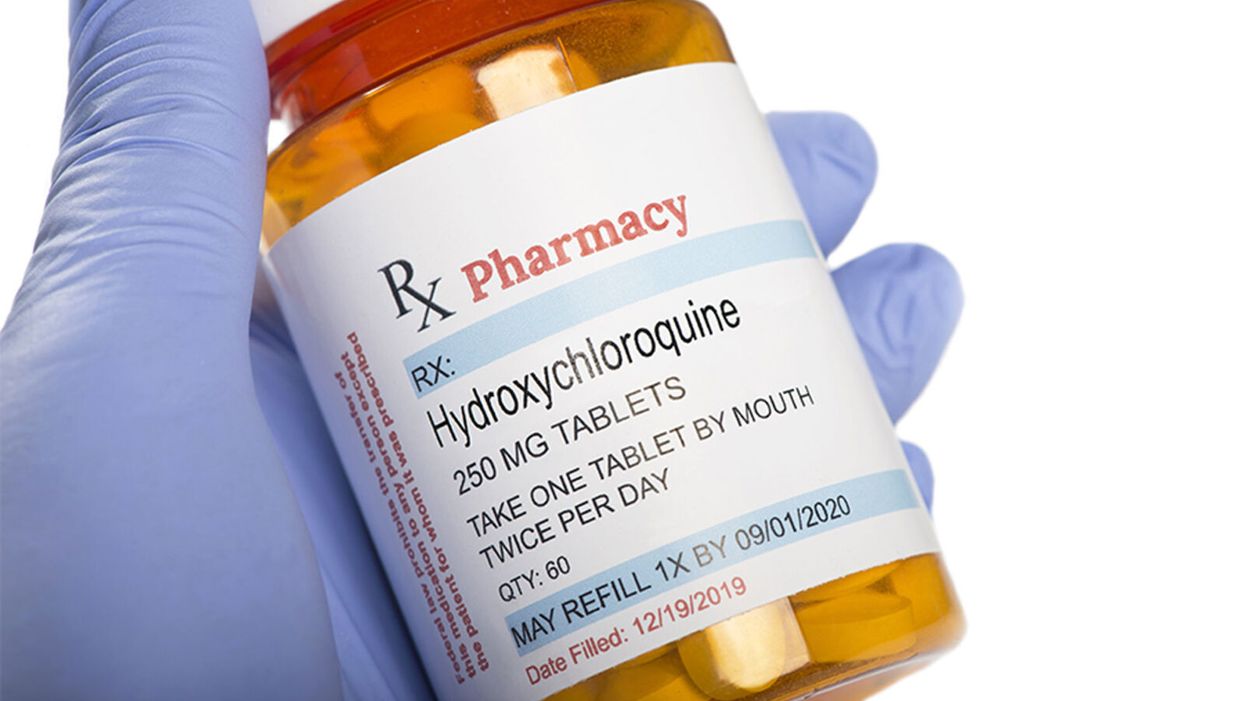
The Only Hydroxychloroquine Story You Need to Read
Hydroxychloroquine has been shown not to provide benefit for COVID-19 patients in multiple randomized controlled trials, despite continuous misinformation asserting its alleged effectiveness.
In the early days of a pandemic caused by a virus with no existing treatments, many different compounds are often considered and tried in an attempt to help patients.
It all relates back to a profound question: How do we know what we know?
Many of these treatments fall by the wayside as evidence accumulates regarding actual efficacy. At that point, other treatments become standard of care once their benefit is proven in rigorously designed trials.
However, about seven months into the pandemic, we're still seeing political resurrection of a treatment that has been systematically studied and demonstrated in well-designed randomized controlled trials to not have benefit.
The hydroxychloroquine (and by extension chloroquine) story is a complicated one that was difficult to follow even before it became infused with politics. It is a simple fact that these drugs, long approved by the Food and Drug Administration (FDA), work in Petri dishes against various viruses including coronaviruses. This set of facts provided biological plausibility to support formally studying their use in the clinical treatment and prevention of COVID-19. As evidence from these studies accumulates, it is a cognitive requirement to integrate that knowledge and not to evade it. This also means evaluating the rigor of the studies.
In recent days we have seen groups yet again promoting the use of hydroxychloroquine in, what is to me, a baffling disregard of the multiple recent studies that have shown no benefit. Indeed, though FDA-approved for other indications like autoimmune conditions and preventing malaria, the emergency use authorization for COVID-19 has been rescinded (which means the government cannot stockpile it). Still, however, many patients continue to ask for the drug, compelled by political commentary, viral videos, and anecdotal data. Yet most doctors (like myself) are refusing to write the prescriptions outside of a clinical trial – a position endorsed by professional medical organizations such as the American College of Physicians and the Infectious Diseases Society of America. Why this disconnect?
It all relates back to a profound question: How do we know what we know? In science, we use the scientific method – the process of observing reality, coming up with a hypothesis about what might be true, and testing that hypothesis as thoroughly as possible until we discover the objective truth.
The confusion we're seeing now stems from an inability to distinguish between anecdotes reported by physicians (observational data) and an actual evidence base. This is understandable among the general public but when done by a healthcare professional, it reveals a disdain for reason, logic, and the scientific method.
The Difference Between Observational Data and Randomized Controlled Trials
The power of informal observation is crucial. It is part of the scientific method but primarily as a basis for generating hypotheses that we can test. How do we conduct medical tests? The gold standard is the double-blind, randomized, placebo-controlled trial. This means that neither the researchers nor the volunteers know who is getting a drug and who is getting a sugar pill. Then both groups of the trial, called arms, can be compared to determine whether the people who got the drug fared better. This study design prevents biases and the placebo effect from confounding the data and undermining the veracity of the results.
For example, a seemingly beneficial effect might be seen in an observational study with no blinding and no control group. In such a case, all patients are openly given the drug and their doctors observe how they do. A prime example is the 36-patient single-arm study from France that generated a tremendous amount of interest after President Trump tweeted about it. But this kind of a study by its nature cannot answer the critical question: Was the positive effect because of hydroxychloroquine or just the natural course of the illness? In other words, would someone have recovered in a similar fashion regardless of the drug? What is the role of the placebo effect?
These are reasons why it is crucial to give a placebo to a control group that is as similar in every respect as possible to those receiving the intervention. Then we attempt to find out by comparing the two groups: What is the side effect profile of the drug? Are the groups large enough to detect a relatively rare safety concern? How long were the patients followed for? Was something else responsible for making the patients get better, such as the use of steroids (as likely was the case in the Henry Ford study)?
Looking at the two major hydroxychloroquine trials, it is apparent that, when studied using the best tools of clinical trials, no benefit is likely to occur.
All of these considerations amount to just a fraction of the questions that can be answered more definitively in a well-designed large randomized controlled trial than in observational studies. Indeed, an observational study from New York failed to show any benefit in hospitalized patients, showing how unclear and disparate the results can be with these types of studies. A New York retrospective study (which examined patient outcomes after they were already treated) had similar results and included the use of azithromycin.
When evaluating a study, it is also important to note whether conflicts of interest exist, as well as the quality of the peer review and the data itself. In the case of the French study, for example, the paper was published in a journal in which one of the authors was editor-in-chief, and it was accepted for publication after 24 hours. Patients who fared poorly on hydroxychloroquine were also left out of the study altogether, skewing the results.
What Randomized Controlled Trials Have Shown
Looking at the two major hydroxychloroquine trials, it is apparent that, when studied using the best tools of clinical trials, no benefit is likely to occur. The most important of these studies to announce results was part of the Recovery trial, which was designed to test multiple interventions in the treatment of COVID-19. This trial, which has yet to be formally published, was a randomized controlled trial that involved over 1500 hospitalized patients being administered hydroxychloroquine compared to over 3000 who did not receive the medication. Clinical testing requires large numbers of patients to have the power to demonstrate statistical significance -- the threshold at which any apparent benefit is more than you would expect by random chance alone.
In this study, hydroxychloroquine provided no mortality benefit or even a benefit in hospital length of stay. In fact, the opposite occurred. Hydroxychloroquine patients were more likely to stay in the hospital longer and were more likely to require mechanical ventilation. Additionally, smaller randomized trials conducted in China have not shown benefit either.
Another major study involved the use of hydroxychloroquine to prevent illness in people who were exposed to COVID-19. These results, published in The New England Journal of Medicine, included over 800 patients who were studied in a randomized double-blind controlled trial and also failed to show any benefit.
But what about adding the antibiotic azithromycin in conjunction with hydroxychloroquine? A three-arm randomized controlled study involving over 500 patients hospitalized with mild to moderate COVID-19 was conducted. Its results, also published in The New England Journal of Medicine, failed to show any benefit – with or without azithromycin – and demonstrated evidence of harm. Those who received these treatments had elevations of their liver function tests and heart rhythm abnormalities. These findings hold despite the retraction of an observational study showing similar results.
Additionally, when used in combination with remdesivir – an experimental antiviral – hydroxychloroquine has been shown to be associated with worse outcomes and more side effects.
But what about in mildly ill patients not requiring hospitalization? There was no benefit found in a randomized double-blind placebo-controlled trial of 400 patients, the majority of whom were given the drug within one day of symptoms.
Some randomized controlled studies have yet to report their findings on hydroxychloroquine in non-hospitalized patients, with the use of zinc (which has some evidence in the treatment of the common cold, another ailment that can be caused by coronaviruses). And studies have yet to come out regarding whether hydroxychloroquine can prevent people from getting sick before they are even exposed. But the preponderance of the evidence from studies designed specifically to find benefit for treating COVID-19 does not support its use outside of a research setting.
Today – even with some studies (including those with zinc) still ongoing – if a patient asked me to prescribe them hydroxychloroquine for any severity or stage of illness, with or without zinc, with or without azithromycin, I would refrain. I would explain that, based on the evidence from clinical trials that has been amassed, there is no reason to believe that it will alter the course of illness for the better.
Failing to recognize the reality of the situation runs the risk of crowding out other more promising treatments and creating animosity where none should exist.
What has been occurring is a continual shifting of goalposts with each negative hydroxychloroquine study. Those in favor of the drug protest that a trial did not include azithromycin or zinc or wasn't given at the right time to the right patients. While there may be biological plausibility to treating illness early or combining treatments with zinc, it can only be definitively shown in a randomized, controlled prospective study.
The bottom line: A study that only looks at past outcomes in one group of patients – even when well conducted – is at most hypothesis generating and cannot be used as the sole basis for a new treatment paradigm.
Some may argue that there is no time to wait for definitive studies, but no treatment is benign. The risk/benefit ratio is not the same for every possible use of the drug. For example, hydroxychloroquine has a long record of use in rheumatoid arthritis and systemic lupus (whose patients are facing shortages because of COVID-19 related demand). But the risk of side effects for many of these patients is worth taking because of the substantial benefit the drug provides in treating those conditions.
In COVID-19, however, the disease apparently causes cardiac abnormalities in a great deal of many mild cases, a situation that should prompt caution when using any drugs that have known effects on the cardiac system -- drugs like hydroxychloroquine and azithromycin.
My Own Experience
It is not the case that every physician was biased against this drug from the start. Indeed, most of us wanted it to be shown to be beneficial, as it was a generic drug that was widely available and very familiar. In fact, early in the pandemic I prescribed it to hospitalized patients on two occasions per a hospital protocol. However, it is impossible for me as a sole clinician to know whether it worked, was neutral, or was harmful. In recent days, however, I have found the hydroxychloroquine talk to have polluted the atmosphere. One recent patient was initially refusing remdesivir, a drug proven in large randomized trials to have effectiveness, because he had confused it with hydroxychloroquine.
Moving On to Other COVID Treatments: What a Treatment Should Do
The story of hydroxychloroquine illustrates a fruitless search for what we are actually looking for in a COVID-19 treatment. In short, we are looking for a medication that can decrease symptoms, decrease complications, hasten recovery, decrease hospitalizations, decrease contagiousness, decrease deaths, and prevent infection. While it is unlikely to find a single antiviral that can accomplish all of these, fulfilling even just one is important.
For example, remdesivir hastens recovery and dexamethasone decreases mortality. Definitive results of the use of convalescent plasma and immunomodulating drugs such as siltuxamab, baricitinib, and anakinra (for use in the cytokine storms characteristic of severe disease) are still pending, as are the trials with monoclonal antibodies.
While it was crucial that the medical and scientific community definitively answer the questions surrounding the use of chloroquine and hydroxychloroquine in the treatment of COVID-19, it is time to face the facts and accept that its use for the treatment of this disease is not likely to be beneficial. Failing to recognize the reality of the situation runs the risk of crowding out other more promising treatments and creating animosity where none should exist.
Dr. Adalja is focused on emerging infectious disease, pandemic preparedness, and biosecurity. He has served on US government panels tasked with developing guidelines for the treatment of plague, botulism, and anthrax in mass casualty settings and the system of care for infectious disease emergencies, and as an external advisor to the New York City Health and Hospital Emergency Management Highly Infectious Disease training program, as well as on a FEMA working group on nuclear disaster recovery. Dr. Adalja is an Associate Editor of the journal Health Security. He was a coeditor of the volume Global Catastrophic Biological Risks, a contributing author for the Handbook of Bioterrorism and Disaster Medicine, the Emergency Medicine CorePendium, Clinical Microbiology Made Ridiculously Simple, UpToDate's section on biological terrorism, and a NATO volume on bioterrorism. He has also published in such journals as the New England Journal of Medicine, the Journal of Infectious Diseases, Clinical Infectious Diseases, Emerging Infectious Diseases, and the Annals of Emergency Medicine. He is a board-certified physician in internal medicine, emergency medicine, infectious diseases, and critical care medicine. Follow him on Twitter: @AmeshAA
Drugs That Trick Older People’s Bodies to Behave Younger Might Boost the Effectiveness of a COVID-19 Vaccine
Because vaccination may be less effective in older people, it is imperative to test now whether immune boosters could help the efficacy of a COVID-19 vaccine in the elderly.
In our April 23rd editorial for this magazine, we argued that addressing the COVID-19 pandemic requires that we both fight the SARS-CoV-2 virus and fortify the human hosts who are most vulnerable to it.
Two recent phase 2 studies in older adults have suggested that a new category of drugs called rapalogues can in some cases increase the immunization capacity of older adults.
Because people over 70 account for more than 80 percent of reported COVID-19 deaths globally, this means we must do everything possible to protect our elders.
A range of recent studies have suggested that systemic knobs might metaphorically be turned to slow the cellular aging process, making us better able to fight off the many diseases correlated with aging. These types of systemic changes might be used to stem the specific decline in immunity caused by aging and to increases the biological capacity of elderly people to effectively fight viral infection.
But while helping make older people more resilient in the face of a viral infection is critical, that's not the only way geroscience can help in our fight against this deadly pandemic.
As we move toward hopefully developing one or more COVID-19 vaccines, researchers must more fully appreciate the ways in which traditional vaccines can be less effective in older people than in younger ones.
Repeated studies have shown that the flu vaccine, for example, has lower efficacy in older people than in younger ones. Older people tend to develop fewer antibodies after being vaccinated because a subset of their white blood cells, called T cells, have become less responsive over time. Some inflammatory peptides that increase with aging are also preventing the action of those T cells.
This is why there's a distinct possibility that a future COVD-19 vaccine, particularly one utilizing the traditional attenuated virus approach, could be less effective in older people than in younger ones.
Given the extreme urgency of developing vaccines that work well for everyone, we need to make sure that researchers are exploring all of the ways our elders can be best protected. While generating a vaccine that works equally well for people of all ages would be ideal, we can't count on that.
One way to bridge this gap might be to trick the bodies of older people into behaving as if they are younger just at the moment what a vaccine is delivered by giving them pre-immunization boosters.
Two recent phase 2 studies in older adults have suggested that a new category of drugs called rapalogues can in some cases increase the immunization capacity of older adults. Use of the drug for a short time period before flu shot immunization increased the antibody production for the flu and resulted in a 52 percent decrease in the occurrence of severe diseases needing medical help or hospitalization. This short-term pre-immunization intervention can also decrease the severity of serious respiratory tract infections, the deadliest manifestations of COVID-19, by similar magnitude. These patients also had almost half the incidence of the non-COVID-19 coronaviruses associated with the common cold.
The fact that those people were protected by treatment before hospitalization suggests metformin may have a role in boosting the vaccination of older people.
An inexpensive generic drug called metformin similarly targets the decline in immunity and inflammation (and extends health span and lifespan) in animals and has been used for decades to protect against the flu. A recent paper from a hospital in Wuhan, China showed that mortality of elderly COVID-19 diabetic patients on metformin was 25 percent less than that of patients with diabetes but not on metformin.
Another study from the U.S. showed that COVID-19 patients on metformin had a 20 percent decrease in mortality and lower inflammation. The fact that those people were protected by treatment before hospitalization suggests metformin may have a role in boosting the vaccination of older people.
We don't yet know whether rapalogues or metformin could be used as COVID-19 immunization boosters, not least because we don't have those vaccines. But we can and should make sure that all vaccine trials including older subjects also consider offering a subset of those subjects appropriate doses of rapalogues or metformin to explore whether doing so can boost the efficacy of a given vaccine.
If we weren't in the middle of the worst pandemic in a century, we would have more time to test our vaccines slowly and sequentially. In the context of the current crisis, however, testing whether immunization boosters might increase the efficacy of potential COVID-19 vaccines for older adults is at the very least a hypothesis worth exploring.