Anti-Aging Pioneer Aubrey de Grey: “People in Middle Age Now Have a Fair Chance”
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

Aubrey de Grey at the World Stem Cell Summit in Miami on January 25, 2018.
Aging is not a mystery, says famed researcher Dr. Aubrey de Grey, perhaps the world's foremost advocate of the provocative view that medical technology will one day allow humans to control the aging process and live healthily into our hundreds—or even thousands.
"The cultural attitudes toward all of this are going to be completely turned upside down by sufficiently promising results in the lab, in mice."
He likens aging to a car wearing down over time; as the body operates normally, it accumulates damage which can be tolerated for a while, but eventually sends us into steep decline. The most promising way to escape this biological reality, he says, is to repair the damage as needed with precise scientific tools.
The bad news is that doing this groundbreaking research takes a long time and a lot of money, which has not always been readily available, in part due to a cultural phenomenon he terms "the pro-aging trance." Cultural attitudes have long been fatalistic about the inevitability of aging; many people balk at the seemingly implausible prospect of indefinite longevity.
But the good news for de Grey—and those who are cheering him on—is that his view is becoming less radical these days. Both the academic and private sectors are racing to tackle aging; his own SENS Research Foundation, for one, has spun out into five different companies. Defeating aging, he says, "is not just a future industry; it's an industry now that will be both profitable and extremely good for your health."
De Grey sat down with Editor-in-Chief Kira Peikoff at the World Stem Cell Summit in Miami to give LeapsMag the latest scoop on his work. Here is an edited and condensed version of our conversation.
Since your book Ending Aging was published a decade ago, scientific breakthroughs in stem cell research, genome editing, and other fields have taken the world by storm. Which of these have most affected your research?
They have all affected it a lot in one way, and hardly at all in another way. They have speeded it up--facilitated short cuts, ways to get where we're already trying to go. What they have not done is identified any fundamental changes to the overall strategy. In the book, we described the seven major types of damage, and particular ways of going about fixing each of them, and that hasn't changed.
"Repair at the microscopic level, one would be able to expect to do without surgery, just by injecting the right kind of stem cells."
Has any breakthrough specifically made the biggest impact?
It's not just the obvious things, like iPS (induced pluripotent stem cells) and CRISPR (a precise tool for editing genes). It's also the more esoteric things that applied specifically to certain of our areas, but most people don't really know about them. For example, the identification of how to control something called co-translational mitochondrial protein import.
How much of the future of anti-aging treatments will involve regeneration of old tissue, or wholesale growth of new organs?
The more large-scale ones, regenerating whole new organs, are probably only going to play a role in the short-term and will be phased out relatively rapidly, simply because, in order to be useful, one has to employ surgery, which is really invasive. We'll want to try to get around that, but it seems quite likely that in the very early stages, the techniques we have for repairing things at the molecular and cellular level in situ will be insufficiently comprehensive, and so we will need to do the more sledgehammer approach of building a whole new organ and sticking it in.
Every time you are in a position where you're replacing an organ, you have the option, in principle, of repairing the organ, without replacing it. And repair at the microscopic level, one would be able to expect to do without surgery, just by injecting the right kind of stem cells or whatever. That would be something one would expect to be able to apply to someone much closer to death's door and much more safely in general, and probably much more cheaply. One would expect that subsequent generations of these therapies would move in that direction.
Your foundation is working on an initiative requiring $50 million in funding—
Well, if we had $50 million per year in funding, we could go about three times faster than we are on $5 million per year.
And you're looking at a 2021 timeframe to start human trials?
That's approximate. Remember, because we accumulate in the body so many different types of damage, that means we have many different types of therapy to repair that damage. And of course, each of those types has to be developed independently. It's very much a divide and conquer therapy. The therapies interact with each other to some extent; the repair of one type of damage may slow down the creation of another type of damage, but still that's how it's going to be.
And some of these therapies are much easier to implement than others. The easier components of what we need to do are already in clinical trials—stem cell therapies especially, and immunotherapy against amyloid in the brain, for example. Even in phase III clinical trials in some cases. So when I talk about a timeframe like 2021, or early 20s shall we say, I'm really talking about the most difficult components.
What recent strides are you most excited about?
Looking back over the past couple of years, I'm particularly proud of the successes we've had in the very most difficult areas. If you go through the 7 components of SENS, there are two that have absolutely been stuck in a rut and have gotten nowhere for 15 to 20 years, and we basically fixed that in both cases. We published two years ago in Science magazine that essentially showed a way forward against the stiffening of the extracellular matrix, which is responsible for things like wrinkles and hypertension. And then a year ago, we published a real breakthrough paper with regard to placing copies of the mitochondria DNA in the nuclear DNA modified in such a way that they still work, which is an idea that had been around for 30 years; everyone had given up on it, some a long time ago, and we basically revived it.
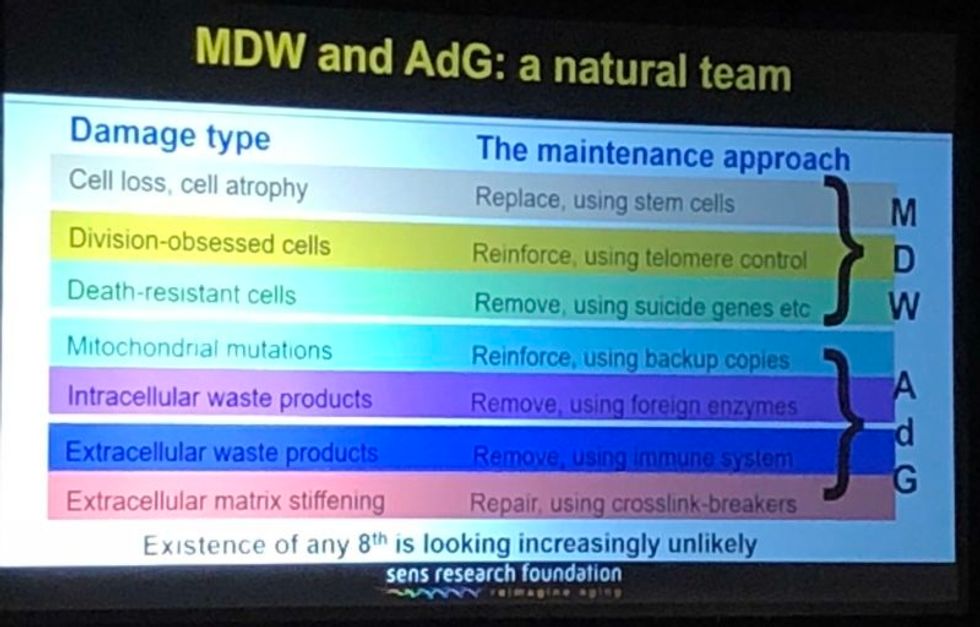
A slide presented by Aubrey de Grey, referencing his collaboration with Mike West at AgeX, showing the 7 types of damage that he believes must be repaired to end aging.
(Courtesy Kira Peikoff)
That's exciting. What do you think are the biggest barriers to defeating aging today: the technological challenges, the regulatory framework, the cost, or the cultural attitude of the "pro-aging" trance?
One can't really address those independently of each other. The technological side is one thing; it's hard, but we know where we're going, we've got a plan. The other ones are very intertwined with each other. A lot of people are inclined to say, the regulatory hurdle will be completely insurmountable, plus people don't recognize aging as a disease, so it's going to be a complete nonstarter. I think that's nonsense. And the reason is because the cultural attitudes toward all of this are going to be completely turned upside down before we have to worry about the regulatory hurdles. In other words, they're going to be turned upside down by sufficiently promising results in the lab, in mice. Once we get to be able to rejuvenate actually old mice really well so they live substantially longer than they otherwise would have done, in a healthy state, everyone's going to know about it and everyone's going to demand – it's not going to be possible to get re-elected unless you have a manifesto commitment to turn the FDA completely upside down and make sure this happens without any kind of regulatory obstacle.
I've been struggling away all these years trying to bring little bits of money in the door, and the reason I have is because of the skepticism as to regards whether this could actually work, combined with the pro-aging trance, which is a product of the skepticism – people not wanting to get their hopes up, so finding excuses about aging being a blessing in disguise, so they don't have to think about it. All of that will literally disintegrate pretty much overnight when we have the right kind of sufficiently impressive progress in the lab. Therefore, the availability of money will also [open up]. It's already cracking: we're already seeing the beginnings of the actual rejuvenation biotechnology industry that I've been talking about with a twinkle in my eye for some years.
"For humans, a 50-50 chance would be twenty years at this point, and there's a 10 percent chance that we won't get there for a hundred years."
Why do you think the culture is starting to shift?
There's no one thing yet. There will be that tipping point I mentioned, perhaps five years from now when we get a real breakthrough, decisive results in mice that make it simply impossible to carry on being fatalistic about all this. Prior to that, what we're already seeing is the impact of sheer old-school repeat advertising—me going out there, banging away and saying the same fucking thing again and again, and nobody saying anything that persuasively knocks me down. … And it's also the fact that we are making incremental amounts of progress, not just ourselves, but the scientific community generally. It has become incrementally more plausible that what I say might be true.
I'm sure you hate getting the timeline question, but if we're five years away from this breakthrough in mice, it's hard to resist asking—how far is that in terms of a human cure?
When I give any kind of timeframes, the only real care I have to take is to emphasize the variance. In this case I think we have got a 50-50 chance of getting to that tipping point in mice within five years from now, certainly it could be 10 or 15 years if we get unlucky. Similarly, for humans, a 50-50 chance would be twenty years at this point, and there's a 10 percent chance that we won't get there for a hundred years.
"I don't get people coming to me saying, well I don't think medicine for the elderly should be done because if it worked it would be a bad thing. People like to ignore this contradiction."
What would you tell skeptical people are the biggest benefits of a very long-lived population?
Any question about the longevity of people is the wrong question. Because the longevity that people fixate about so much will only ever occur as a side effect of health. However long ago you were born or however recently, if you're sick, you're likely to die fairly soon unless we can stop you being sick. Whereas if you're healthy, you're not. So if we do as well as we think we can do in terms of keeping people healthy and youthful however long ago they were born, then the side effect in terms of longevity and life expectancy is likely to be very large. But it's still a side effect, so the way that people actually ought to be—in fact have a requirement to be—thinking, is about whether they want people to be healthy.
Now I don't get people coming to me saying, well I don't think medicine for the elderly should be done because if it worked it would be a bad thing. People like to ignore this contradiction, they like to sweep it under the carpet and say, oh yeah, aging is totally a good thing.
People will never actually admit to the fact that what they are fundamentally saying is medicine for the elderly, if it actually works, would be bad, but still that is what they are saying.
Shifting gears a bit, I'm curious to find out which other radical visionaries in science and tech today you most admire?
Fair question. One is Mike West. I have the great privilege that I now work for him part-time with Age X. I have looked up to him very much for the past ten years, because what he did over the past 20 years starting with Geron is unimaginable today. He was working in an environment where I would not have dreamt of the possibility of getting any private money, any actual investment, in something that far out, that far ahead of its time, and he did it, again and again. It's insane what he managed to do.
What about someone like Elon Musk?
Sure, he's another one. He is totally impervious to the caution and criticism and conservatism that pervades humanity, and he's getting on making these bloody self-driving cars, space tourism, and so on, making them happen. He's thinking just the way I'm thinking really.
"You can just choose how frequently and how thoroughly you repair the damage. And you can make a different choice next time."
You famously said ten years ago that you think the first person to live to 1000 is already alive. Do you think that's still the case?
Definitely, yeah. I can't see how it could not be. Again, it's a probabilistic thing. I said there's at least a 10 percent chance that we won't get to what I call Longevity Escape Velocity for 100 years and if that's true, then the statement about 1000 years being alive already is not going to be the case. But for sure, I believe that the beneficiaries of what we may as well call SENS 1.0, the point where we get to LEV, those people are exceptionally unlikely ever to suffer from any kind of ill health correlated with their age. Because we will never fall below Longevity Escape Velocity once we attain it.
Could someone who was just born today expect—
I would say people in middle age now have a fair chance. Remember – a 50/50 chance of getting to LEV within 20 years, and when you get there, you don't just stay at biologically 70 or 80, you are rejuvenated back to biologically 30 or 40 and you stay there, so your risk of death each year is not related to how long ago you were born, it's the same as a young adult. Today, that's less than 1 in 1000 per year, and that number is going to go down as we get self-driving cars and all that, so actually 1000 is a very conservative number.
So you would be able to choose what age you wanted to go back to?
Oh sure, of course, it's just like a car. What you're doing is you're repairing damage, and the damage is still being created by the body's metabolism, so you can just choose how frequently and how thoroughly you repair the damage. And you can make a different choice next time.
What would be your perfect age?
I have no idea. That's something I don't have an opinion about, because I could change it whenever I like.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Questions remain about new drug for hot flashes
In May, a new drug, Fezolinetant, was approved by the FDA to treat hot flashes associated with menopause.
Vascomotor symptoms (VMS) is the medical term for hot flashes associated with menopause. You are going to hear a lot more about it because a company has a new drug to sell. Here is what you need to know.
Menopause marks the end of a woman’s reproductive capacity. Normal hormonal production associated with that monthly cycle becomes erratic and finally ceases. For some women the transition can be relatively brief with only modest symptoms, while for others the body's “thermostat” in the brain is disrupted and they experience hot flashes and other symptoms that can disrupt daily activity. Lifestyle modification and drugs such as hormone therapy can provide some relief, but women at risk for cancer are advised not to use them and other women choose not to do so.
Fezolinetant, sold by Astellas Pharma Inc. under the product name Veozah™, was approved by the Food and Drug Administration (FDA) on May 12 to treat hot flashes associated with menopause. It is the first in a new class of drugs called neurokinin 3 receptor antagonists, which block specific neurons in the brain “thermostat” that trigger VMS. It does not appear to affect other symptoms of menopause. As with many drugs targeting a brain cell receptor, it must be taken continuously for a few days to build up a good therapeutic response, rather than working as a rescue product such as an asthma inhaler to immediately treat that condition.
Hot flashes vary greatly and naturally get better or resolve completely with time. That contributes to a placebo effect and makes it more difficult to judge the outcome of any intervention. Early this year, a meta analysis of 17 studies of drug trials for hot flashes found an unusually large placebo response in those types of studies; the placebo groups had an average of 5.44 fewer hot flashes and a 36 percent reduction in their severity.
In studies of fezolinetant, the drug recently approved by the FDA, the placebo benefit was strong and persistent. The drug group bested the placebo response to a statistically significant degree but, “If people have gone from 11 hot flashes a day to eight or seven in the placebo group and down to a couple fewer ones in the drug groups, how meaningful is that? Having six hot flashes a day is still pretty unpleasant,” says Diana Zuckerman, president of the National Center for Health Research (NCHR), a health oriented think tank.
“Is a reduction compared to placebo of 2-3 hot flashes per day, in a population of women experiencing 10-11 moderate to severe hot flashes daily, enough relief to be clinically meaningful?” Andrea LaCroix asked a commentary published in Nature Medicine. She is an epidemiologist at the University of California San Diego and a leader of the MsFlash network that has conducted a handful of NIH-funded studies on menopause.
Questions Remain
LaCroix and others have raised questions about how Astellas, the company that makes the new drug, handled missing data from patients who dropped out of the clinical trials. “The lack of detailed information about important parameters such as adherence and missing data raises concerns that the reported benefits of fezolinetant very likely overestimate those that will be observed in clinical practice," LaCroix wrote.
In response to this concern, Anna Criddle, director of global portfolio communications at Astellas, wrote in an email to Leaps.org: “…a full analysis of data, including adherence data and any impact of missing data, was submitted for assessment by [the FDA].”
The company ran the studies at more than 300 sites around the world. Curiously, none appear to have been at academic medical centers, which are known for higher quality research. Zuckerman says, "When somebody is paid to do a study, if they want to get paid to do another study by the same company, they will try to make sure that the results are the results that the company wants.”
Criddle said that Astellas picked the sites “that would allow us to reach a diverse population of women, including race and ethnicity.”
A trial of a lower dose of the drug was conducted in Asia. In March 2022, Astellas issued a press release saying it had failed to prove effectiveness. No further data has been released. Astellas still plans to submit the data, according to Criddle. Results from clinical trials funded by the U.S. goverment must be reported on clinicaltrials.gov within one year of the study's completion - a deadline that, in this case, has expired.
The measurement scale for hot flashes used in the studies, mild-moderate-severe, also came in for criticism. “It is really not good scale, there probably isn’t a broad enough range of things going on or descriptors,” says David Rind. He is chief medical officer of the Institute for Clinical and Economic Review (ICER), a nonprofit authority on new drugs. It conducted a thorough review and analysis of fezolinestant using then existing data gathered from conference abstracts, posters and presentations and included a public stakeholder meeting in December. A 252-page report was published in January, finding “considerable uncertainty about the comparative net health benefits of fezolinetant” versus hormone therapy.
Questions surrounding some of these issues might have been answered if the FDA had chosen to hold a public advisory committee meeting on fezolinetant, which it regularly does for first in class medicines. But the agency decided such a meeting was unnecessary.
Cost
There was little surprise when Astellas announced a list price for fezolinetant of $550 a month ($6000 annually) and a program of patient assistance to ease out of pocket expenses. The company had already incurred large expenses.
In 2017 Astellas purchased the company that originally developed fezolinetant for $534 million plus several hundred million in potential royalties. The drug company ran a "disease awareness” ad, Heat on the Street, hat aired during the Super Bowl in February, where 30 second ads cost about $7 million. Industry analysts have projected sales to be $1.9 billion by 2028.
ICER’s pre-approval evaluation said fezolinetant might "be considered cost-effective if priced around $2,000 annually. ... [It]will depend upon its price and whether it is considered an alternative to MHT [menopause hormone treatment] for all women or whether it will primarily be used by women who cannot or will not take MHT."
Criddle wrote that Astellas set the price based on the novelty of the science, the quality of evidence for the drug and its uniqueness compared to the rest of the market. She noted that an individual’s payment will depend on how much their insurance company decides to cover. “[W]e expect insurance coverage to increase over the course of the year and to achieve widespread coverage in the U.S. over time.”
Leaps.org wrote to and followed up with nine of the largest health insurers/providers asking basic questions about their coverage of fezolinetant. Only two responded. Jennifer Martin, the deputy chief consultant for pharmacy benefits management at the Department of Veterans Affairs, said the agency “covers all drugs from the date that they are launched.” Decisions on whether it will be included in the drug formulary and what if any copays might be required are under review.
“[Fezolinetant] will go through our standard P&T Committee [patient and treatment] review process in the next few months, including a review of available efficacy data, safety data, clinical practice guidelines, and comparison with other agents used for vasomotor symptoms of menopause," said Phil Blando, executive director of corporate communications for CVS Health.
Other insurers likely are going through a similar process to decide issues such as limiting coverage to women who are advised not to use hormones, how much copay will be required, and whether women will be required to first try other options or obtain approvals before getting a prescription.
Rind wants to see a few years of use before he prescribes fezolinetant broadly, and believes most doctors share his view. Nor will they be eager to fill out the additional paperwork required for women to participate in the Astellas patient assistance program, he added.
Safety
Astellas is marketing its drug by pointing out risks of hormone therapy, such as a recent paper in The BMJ, which noted that women who took hormones for even a short period of time had a 24 percent increased risk of dementia. While the percentage was scary, the combined number of women both on and off hormones who developed dementia was small. And it is unclear whether hormones are causing dementia or if more severe hot flashes are a marker for higher risk of developing dementia. This information is emerging only after 80 years of hundreds of millions of women using hormones.
In contrast, the label for fezolinetant prohibits “concomitant use with CYP1A2 inhibitors” and requires testing for liver and kidney function prior to initiating the drug and every three months thereafter. There is no human or animal data on use in a geriatric population, defined as 65 or older, a group that is likely to use the drug. Only a few thousand women have ever taken fezolinetant and most have used it for just a few months.
Options
A woman seeking relief from symptoms of menopause would like to see how fezolintant compares with other available treatment options. But Astellas did not conduct such a study and Andrea LaCroix says it is unlikely that anyone ever will.
ICER has come the closest, with a side-by-side analysis of evidence-based treatments and found that fezolinetant performed quite similarly and modestly as the others in providing relief from hot flashes. Some treatments also help with other symptoms of menopause, which fezolinetant does not.
There are many coping strategies that women can adopt to deal with hot flashes; one of the most common is dressing in layers (such as a sleeveless blouse with a sweater) that can be added or subtracted as conditions require. Avoiding caffeine, hot liquids, and spicy foods is another common strategy. “I stopped drinking hot caffeinated drinks…for several years, and you get out of the habit of drinking them,” says Zuckerman.
LaCroix curates those options at My Meno Plan, which includes a search function where you can enter your symptoms and identify which treatments might work best for you. It also links to published research papers. She says the goal is to empower women with information to make informed decisions about menopause.
A company in England has made a test that picks out the compounds from breath that reveal if people have liver disease.
Every year, around two million people worldwide die of liver disease. While some people inherit the disease, it’s most commonly caused by hepatitis, obesity and alcoholism. These underlying conditions kill liver cells, causing scar tissue to form until eventually the liver cannot function properly. Since 1979, deaths due to liver disease have increased by 400 percent.
The sooner the disease is detected, the more effective treatment can be. But once symptoms appear, the liver is already damaged. Around 50 percent of cases are diagnosed only after the disease has reached the final stages, when treatment is largely ineffective.
To address this problem, Owlstone Medical, a biotech company in England, has developed a breath test that can detect liver disease earlier than conventional approaches. Human breath contains volatile organic compounds (VOCs) that change in the first stages of liver disease. Owlstone’s breath test can reliably collect, store and detect VOCs, while picking out the specific compounds that reveal liver disease.
“There’s a need to screen more broadly for people with early-stage liver disease,” says Owlstone’s CEO Billy Boyle. “Equally important is having a test that's non-invasive, cost effective and can be deployed in a primary care setting.”
The standard tool for detection is a biopsy. It is invasive and expensive, making it impractical to use for people who aren't yet symptomatic. Meanwhile, blood tests are less invasive, but they can be inaccurate and can’t discriminate between different stages of the disease.
In the past, breath tests have not been widely used because of the difficulties of reliably collecting and storing breath. But Owlstone’s technology could help change that.
The team is testing patients in the early stages of advanced liver disease, or cirrhosis, to identify and detect these biomarkers. In an initial study, Owlstone’s breathalyzer was able to pick out patients who had early cirrhosis with 83 percent sensitivity.
Boyle’s work is personally motivated. His wife died of colorectal cancer after she was diagnosed with a progressed form of the disease. “That was a big impetus for me to see if this technology could work in early detection,” he says. “As a company, Owlstone is interested in early detection across a range of diseases because we think that's a way to save lives and a way to save costs.”
How it works
In the past, breath tests have not been widely used because of the difficulties of reliably collecting and storing breath. But Owlstone’s technology could help change that.
Study participants breathe into a mouthpiece attached to a breath sampler developed by Owlstone. It has cartridges are designed and optimized to collect gases. The sampler specifically targets VOCs, extracting them from atmospheric gases in breath, to ensure that even low levels of these compounds are captured.
The sampler can store compounds stably before they are assessed through a method called mass spectrometry, in which compounds are converted into charged atoms, before electromagnetic fields filter and identify even the tiniest amounts of charged atoms according to their weight and charge.
The top four compounds in our breath
In an initial study, Owlstone captured VOCs in breath to see which ones could help them tell the difference between people with and without liver disease. They tested the breath of 46 patients with liver disease - most of them in the earlier stages of cirrhosis - and 42 healthy people. Using this data, they were able to create a diagnostic model. Individually, compounds like 2-Pentanone and limonene performed well as markers for liver disease. Owlstone achieved even better performance by examining the levels of the top four compounds together, distinguishing between liver disease cases and controls with 95 percent accuracy.
“It was a good proof of principle since it looks like there are breath biomarkers that can discriminate between diseases,” Boyle says. “That was a bit of a stepping stone for us to say, taking those identified, let’s try and dose with specific concentrations of probes. It's part of building the evidence and steering the clinical trials to get to liver disease sensitivity.”
Sabine Szunerits, a professor of chemistry in Institute of Electronics at the University of Lille, sees the potential of Owlstone’s technology.
“Breath analysis is showing real promise as a clinical diagnostic tool,” says Szunerits, who has no ties with the company. “Owlstone Medical’s technology is extremely effective in collecting small volatile organic biomarkers in the breath. In combination with pattern recognition it can give an answer on liver disease severity. I see it as a very promising way to give patients novel chances to be cured.”
Improving the breath sampling process
Challenges remain. With more than one thousand VOCs found in the breath, it can be difficult to identify markers for liver disease that are consistent across many patients.
Julian Gardner is a professor of electrical engineering at Warwick University who researches electronic sensing devices. “Everyone’s breath has different levels of VOCs and different ones according to gender, diet, age etc,” Gardner says. “It is indeed very challenging to selectively detect the biomarkers in the breath for liver disease.”
So Owlstone is putting chemicals in the body that they know interact differently with patients with liver disease, and then using the breath sampler to measure these specific VOCs. The chemicals they administer are called Exogenous Volatile Organic Compound) probes, or EVOCs.
Most recently, they used limonene as an EVOC probe, testing 29 patients with early cirrhosis and 29 controls. They gave the limonene to subjects at specific doses to measure how its concentrations change in breath. The aim was to try and see what was happening in their livers.
“They are proposing to use drugs to enhance the signal as they are concerned about the sensitivity and selectivity of their method,” Gardner says. “The approach of EVOC probes is probably necessary as you can then eliminate the person-to-person variation that will be considerable in the soup of VOCs in our breath.”
Through these probes, Owlstone could identify patients with liver disease with 83 percent sensitivity. By targeting what they knew was a disease mechanism, they were able to amplify the signal. The company is starting a larger clinical trial, and the plan is to eventually use a panel of EVOC probes to make sure they can see diverging VOCs more clearly.
“I think the approach of using probes to amplify the VOC signal will ultimately increase the specificity of any VOC breath tests, and improve their practical usability,” says Roger Yazbek, who leads the South Australian Breath Analysis Research (SABAR) laboratory in Flinders University. “Whilst the findings are interesting, it still is only a small cohort of patients in one location.”
The future of breath diagnosis
Owlstone wants to partner with pharmaceutical companies looking to learn if their drugs have an effect on liver disease. They’ve also developed a microchip, a miniaturized version of mass spectrometry instruments, that can be used with the breathalyzer. It is less sensitive but will enable faster detection.
Boyle says the company's mission is for their tests to save 100,000 lives. "There are lots of risks and lots of challenges. I think there's an opportunity to really establish breath as a new diagnostic class.”

