Scientists redesign bacteria to tackle the antibiotic resistance crisis
Probiotic bacteria can be engineered to fight antibiotic-resistant superbugs by releasing chemicals that kill them.
In 1945, almost two decades after Alexander Fleming discovered penicillin, he warned that as antibiotics use grows, they may lose their efficiency. He was prescient—the first case of penicillin resistance was reported two years later. Back then, not many people paid attention to Fleming’s warning. After all, the “golden era” of the antibiotics age had just began. By the 1950s, three new antibiotics derived from soil bacteria — streptomycin, chloramphenicol, and tetracycline — could cure infectious diseases like tuberculosis, cholera, meningitis and typhoid fever, among others.
Today, these antibiotics and many of their successors developed through the 1980s are gradually losing their effectiveness. The extensive overuse and misuse of antibiotics led to the rise of drug resistance. The livestock sector buys around 80 percent of all antibiotics sold in the U.S. every year. Farmers feed cows and chickens low doses of antibiotics to prevent infections and fatten up the animals, which eventually causes resistant bacterial strains to evolve. If manure from cattle is used on fields, the soil and vegetables can get contaminated with antibiotic-resistant bacteria. Another major factor is doctors overprescribing antibiotics to humans, particularly in low-income countries. Between 2000 to 2018, the global rates of human antibiotic consumption shot up by 46 percent.
In recent years, researchers have been exploring a promising avenue: the use of synthetic biology to engineer new bacteria that may work better than antibiotics. The need continues to grow, as a Lancet study linked antibiotic resistance to over 1.27 million deaths worldwide in 2019, surpassing HIV/AIDS and malaria. The western sub-Saharan Africa region had the highest death rate (27.3 people per 100,000).
Researchers warn that if nothing changes, by 2050, antibiotic resistance could kill 10 million people annually.
To make it worse, our remedy pipelines are drying up. Out of the 18 biggest pharmaceutical companies, 15 abandoned antibiotic development by 2013. According to the AMR Action Fund, venture capital has remained indifferent towards biotech start-ups developing new antibiotics. In 2019, at least two antibiotic start-ups filed for bankruptcy. As of December 2020, there were 43 new antibiotics in clinical development. But because they are based on previously known molecules, scientists say they are inadequate for treating multidrug-resistant bacteria. Researchers warn that if nothing changes, by 2050, antibiotic resistance could kill 10 million people annually.
The rise of synthetic biology
To circumvent this dire future, scientists have been working on alternative solutions using synthetic biology tools, meaning genetically modifying good bacteria to fight the bad ones.
From the time life evolved on earth around 3.8 billion years ago, bacteria have engaged in biological warfare. They constantly strategize new methods to combat each other by synthesizing toxic proteins that kill competition.
For example, Escherichia coli produces bacteriocins or toxins to kill other strains of E.coli that attempt to colonize the same habitat. Microbes like E.coli (which are not all pathogenic) are also naturally present in the human microbiome. The human microbiome harbors up to 100 trillion symbiotic microbial cells. The majority of them are beneficial organisms residing in the gut at different compositions.
The chemicals that these “good bacteria” produce do not pose any health risks to us, but can be toxic to other bacteria, particularly to human pathogens. For the last three decades, scientists have been manipulating bacteria’s biological warfare tactics to our collective advantage.
In the late 1990s, researchers drew inspiration from electrical and computing engineering principles that involve constructing digital circuits to control devices. In certain ways, every cell in living organisms works like a tiny computer. The cell receives messages in the form of biochemical molecules that cling on to its surface. Those messages get processed within the cells through a series of complex molecular interactions.
Synthetic biologists can harness these living cells’ information processing skills and use them to construct genetic circuits that perform specific instructions—for example, secrete a toxin that kills pathogenic bacteria. “Any synthetic genetic circuit is merely a piece of information that hangs around in the bacteria’s cytoplasm,” explains José Rubén Morones-Ramírez, a professor at the Autonomous University of Nuevo León, Mexico. Then the ribosome, which synthesizes proteins in the cell, processes that new information, making the compounds scientists want bacteria to make. “The genetic circuit remains separated from the living cell’s DNA,” Morones-Ramírez explains. When the engineered bacteria replicates, the genetic circuit doesn’t become part of its genome.
Highly intelligent by bacterial standards, some multidrug resistant V. cholerae strains can also “collaborate” with other intestinal bacterial species to gain advantage and take hold of the gut.
In 2000, Boston-based researchers constructed an E.coli with a genetic switch that toggled between turning genes on and off two. Later, they built some safety checks into their bacteria. “To prevent unintentional or deleterious consequences, in 2009, we built a safety switch in the engineered bacteria’s genetic circuit that gets triggered after it gets exposed to a pathogen," says James Collins, a professor of biological engineering at MIT and faculty member at Harvard University’s Wyss Institute. “After getting rid of the pathogen, the engineered bacteria is designed to switch off and leave the patient's body.”
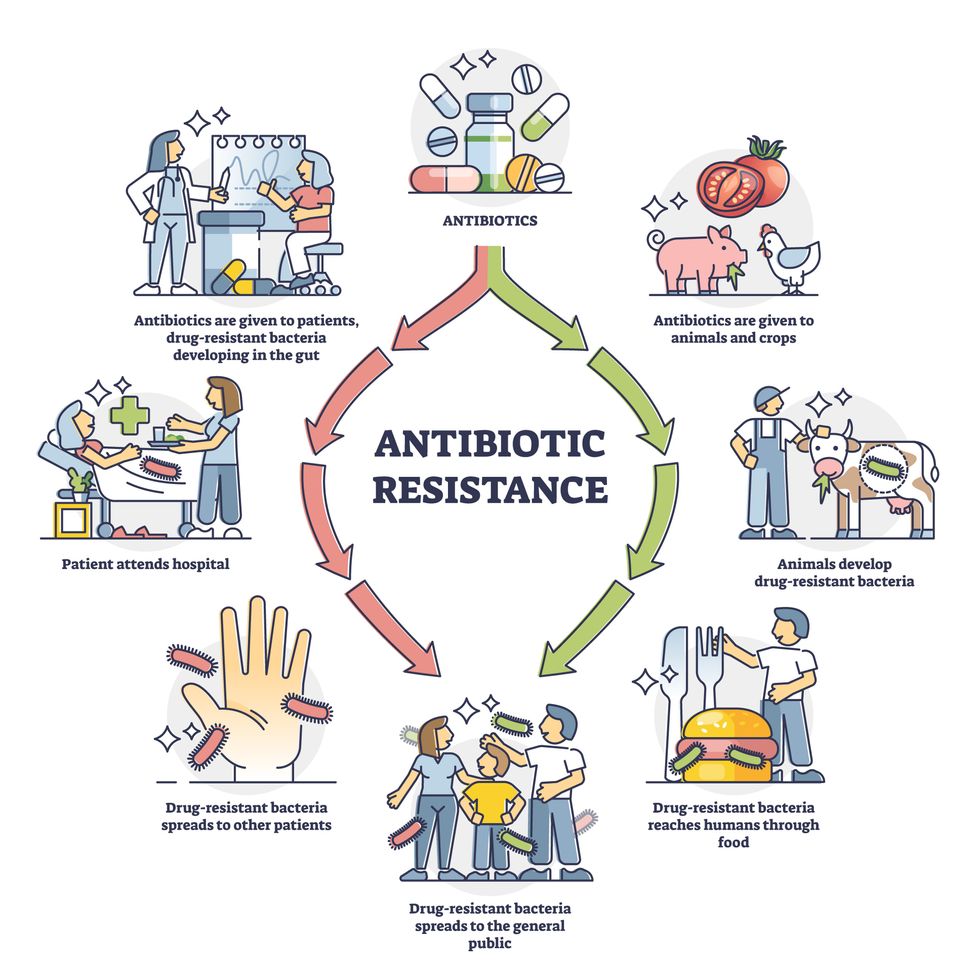
Overuse and misuse of antibiotics causes resistant strains to evolve
Adobe Stock
Seek and destroy
As the field of synthetic biology developed, scientists began using engineered bacteria to tackle superbugs. They first focused on Vibrio cholerae, which in the 19th and 20th century caused cholera pandemics in India, China, the Middle East, Europe, and Americas. Like many other bacteria, V. cholerae communicate with each other via quorum sensing, a process in which the microorganisms release different signaling molecules, to convey messages to its brethren. Highly intelligent by bacterial standards, some multidrug resistant V. cholerae strains can also “collaborate” with other intestinal bacterial species to gain advantage and take hold of the gut. When untreated, cholera has a mortality rate of 25 to 50 percent and outbreaks frequently occur in developing countries, especially during floods and droughts.
Sometimes, however, V. cholerae makes mistakes. In 2008, researchers at Cornell University observed that when quorum sensing V. cholerae accidentally released high concentrations of a signaling molecule called CAI-1, it had a counterproductive effect—the pathogen couldn’t colonize the gut.
So the group, led by John March, professor of biological and environmental engineering, developed a novel strategy to combat V. cholerae. They genetically engineered E.coli to eavesdrop on V. cholerae communication networks and equipped it with the ability to release the CAI-1 molecules. That interfered with V. cholerae progress. Two years later, the Cornell team showed that V. cholerae-infected mice treated with engineered E.coli had a 92 percent survival rate.
These findings inspired researchers to sic the good bacteria present in foods like yogurt and kimchi onto the drug-resistant ones.
Three years later in 2011, Singapore-based scientists engineered E.coli to detect and destroy Pseudomonas aeruginosa, an often drug-resistant pathogen that causes pneumonia, urinary tract infections, and sepsis. Once the genetically engineered E.coli found its target through its quorum sensing molecules, it then released a peptide, that could eradicate 99 percent of P. aeruginosa cells in a test-tube experiment. The team outlined their work in a Molecular Systems Biology study.
“At the time, we knew that we were entering new, uncharted territory,” says lead author Matthew Chang, an associate professor and synthetic biologist at the National University of Singapore and lead author of the study. “To date, we are still in the process of trying to understand how long these microbes stay in our bodies and how they might continue to evolve.”
More teams followed the same path. In a 2013 study, MIT researchers also genetically engineered E.coli to detect P. aeruginosa via the pathogen’s quorum-sensing molecules. It then destroyed the pathogen by secreting a lab-made toxin.
Probiotics that fight
A year later in 2014, a Nature study found that the abundance of Ruminococcus obeum, a probiotic bacteria naturally occurring in the human microbiome, interrupts and reduces V.cholerae’s colonization— by detecting the pathogen’s quorum sensing molecules. The natural accumulation of R. obeum in Bangladeshi adults helped them recover from cholera despite living in an area with frequent outbreaks.
The findings from 2008 to 2014 inspired Collins and his team to delve into how good bacteria present in foods like yogurt and kimchi can attack drug-resistant bacteria. In 2018, Collins and his team developed the engineered probiotic strategy. They tweaked a bacteria commonly found in yogurt called Lactococcus lactis to treat cholera.
Engineered bacteria can be trained to target pathogens when they are at their most vulnerable metabolic stage in the human gut. --José Rubén Morones-Ramírez.
More scientists followed with more experiments. So far, researchers have engineered various probiotic organisms to fight pathogenic bacteria like Staphylococcus aureus (leading cause of skin, tissue, bone, joint and blood infections) and Clostridium perfringens (which causes watery diarrhea) in test-tube and animal experiments. In 2020, Russian scientists engineered a probiotic called Pichia pastoris to produce an enzyme called lysostaphin that eradicated S. aureus in vitro. Another 2020 study from China used an engineered probiotic bacteria Lactobacilli casei as a vaccine to prevent C. perfringens infection in rabbits.
In a study last year, Ramírez’s group at the Autonomous University of Nuevo León, engineered E. coli to detect quorum-sensing molecules from Methicillin-resistant Staphylococcus aureus or MRSA, a notorious superbug. The E. coli then releases a bacteriocin that kills MRSA. “An antibiotic is just a molecule that is not intelligent,” says Ramírez. “On the other hand, engineered bacteria can be trained to target pathogens when they are at their most vulnerable metabolic stage in the human gut.”
Collins and Timothy Lu, an associate professor of biological engineering at MIT, found that engineered E. coli can help treat other conditions—such as phenylketonuria, a rare metabolic disorder, that causes the build-up of an amino acid phenylalanine. Their start-up Synlogic aims to commercialize the technology, and has completed a phase 2 clinical trial.
Circumventing the challenges
The bacteria-engineering technique is not without pitfalls. One major challenge is that beneficial gut bacteria produce their own quorum-sensing molecules that can be similar to those that pathogens secrete. If an engineered bacteria’s biosensor is not specific enough, it will be ineffective.
Another concern is whether engineered bacteria might mutate after entering the gut. “As with any technology, there are risks where bad actors could have the capability to engineer a microbe to act quite nastily,” says Collins of MIT. But Collins and Ramírez both insist that the chances of the engineered bacteria mutating on its own are virtually non-existent. “It is extremely unlikely for the engineered bacteria to mutate,” Ramírez says. “Coaxing a living cell to do anything on command is immensely challenging. Usually, the greater risk is that the engineered bacteria entirely lose its functionality.”
However, the biggest challenge is bringing the curative bacteria to consumers. Pharmaceutical companies aren’t interested in antibiotics or their alternatives because it’s less profitable than developing new medicines for non-infectious diseases. Unlike the more chronic conditions like diabetes or cancer that require long-term medications, infectious diseases are usually treated much quicker. Running clinical trials are expensive and antibiotic-alternatives aren’t lucrative enough.
“Unfortunately, new medications for antibiotic resistant infections have been pushed to the bottom of the field,” says Lu of MIT. “It's not because the technology does not work. This is more of a market issue. Because clinical trials cost hundreds of millions of dollars, the only solution is that governments will need to fund them.” Lu stresses that societies must lobby to change how the modern healthcare industry works. “The whole world needs better treatments for antibiotic resistance.”
In today's podcast episode, law professor Gaia Bernstein talks about the challenges of keeping control over our thoughts and actions, even when some powerful forces are pushing in the other direction.
Each afternoon, kids walk through my neighborhood, on their way back home from school, and almost all of them are walking alone, staring down at their phones. It's a troubling site. This daily parade of the zombie children just can’t bode well for the future.
That’s one reason I felt like Gaia Bernstein’s new book was talking directly to me. A law professor at Seton Hall, Gaia makes a strong argument that people are so addicted to tech at this point, we need some big, system level changes to social media platforms and other addictive technologies, instead of just blaming the individual and expecting them to fix these issues.
Gaia’s book is called Unwired: Gaining Control Over Addictive Technologies. It’s fascinating and I had a chance to talk with her about it for today’s podcast. At its heart, our conversation is really about how and whether we can maintain control over our thoughts and actions, even when some powerful forces are pushing in the other direction.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
We discuss the idea that, in certain situations, maybe it's not reasonable to expect that we’ll be able to enjoy personal freedom and autonomy. We also talk about how to be a good parent when it sometimes seems like our kids prefer to be raised by their iPads; so-called educational video games that actually don’t have anything to do with education; the root causes of tech addictions for people of all ages; and what kinds of changes we should be supporting.
Gaia is Seton’s Hall’s Technology, Privacy and Policy Professor of Law, as well as Co-Director of the Institute for Privacy Protection, and Co-Director of the Gibbons Institute of Law Science and Technology. She’s the founding director of the Institute for Privacy Protection. She created and spearheaded the Institute’s nationally recognized Outreach Program, which educated parents and students about technology overuse and privacy.
Professor Bernstein's scholarship has been published in leading law reviews including the law reviews of Vanderbilt, Boston College, Boston University, and U.C. Davis. Her work has been selected to the Stanford-Yale Junior Faculty Forum and received extensive media coverage. Gaia joined Seton Hall's faculty in 2004. Before that, she was a fellow at the Engelberg Center of Innovation Law & Policy and at the Information Law Institute of the New York University School of Law. She holds a J.S.D. from the New York University School of Law, an LL.M. from Harvard Law School, and a J.D. from Boston University.
Gaia’s work on this topic is groundbreaking I hope you’ll listen to the conversation and then consider pre-ordering her new book. It comes out on March 28.

Time to visit your TikTok doc? The good and bad of doctors on social media
Rakhi Patel is among an increasing number of health care professionals, including doctors and nurses, who maintain an active persona on Instagram, TikTok and other social media sites.
Rakhi Patel has carved a hobby out of reviewing pizza — her favorite food — on Instagram. In a nod to her preferred topping, she calls herself thepepperoniqueen. Photos and videos show her savoring slices from scores of pizzerias. In some of them, she’s wearing scrubs — her attire as an inpatient neurology physician associate at Tufts Medical Center in Boston.
“Depending on how you dress your pizza, it can be more nutritious,” said Patel, who suggests a thin crust, sugarless tomato sauce and vegetables galore as healthier alternatives. “There are no boundaries for a health care professional to enjoy pizza.”
Beyond that, “pizza fuels my mental health and makes me happy, especially when loaded with pepperoni,” she said. “If I’m going to be a pizza connoisseur, then I also need to take care of my physical health by ensuring that I get at least three days of exercise per week and eat nutritiously when I’m not eating pizza.”
She’s among an increasing number of health care professionals, including doctors and nurses, who maintain an active persona on social media, according to bioethics researchers. They share their hobbies and interests with people inside and outside the world of medicine, helping patients and the public become acquainted with the humans behind the scrubs or white coats. Other health care experts limit their posts to medical topics, while some opt for a combination of personal and professional commentaries. Depending on the posts, ethical issues may come into play.
“Health care professionals are quite prevalent on social media,” said Mercer Gary, a postdoctoral researcher at The Hastings Center, an independent bioethics research institute in Garrison, New York. “They’ve been posting on #medTwitter for many years, mainly to communicate with one another, but, of course, anyone can see the threads. Most recently, doctors and nurses have become a presence on TikTok.”
On social media, many health care providers perceive themselves to be “humanizing” their profession by coming across as more approachable — “reminding patients that providers are people and workers, as well as repositories of medical expertise,” Gary said. As a result, she noted that patients who are often intimidated by clinicians may feel comfortable enough to overcome barriers to scheduling health care appointments. The use of TikTok in particular may help doctors and nurses connect with younger followers.
When health care providers post on social media, they must bear in mind that they have legal and ethical duties to their patients, profession and society, said Elizabeth Levy, founder and director of Physicians for Justice.
While enduring three years of pandemic conditions, many health care professionals have struggled with burnout, exhaustion and moral distress. “Much health care provider content on social media seeks to expose the difficulties of the work,” Gary added. “TikTok and Instagram reels have shown health care providers crying after losing a patient or exhausted after a night shift in the emergency department.”
A study conducted in Beijing, China and published last year found that TikTok is the world’s most rapidly growing video application, amassing 1.6 billion users in 2021. “More and more patients are searching for information on genitourinary cancers via TikTok,” the study’s authors wrote in Frontiers in Oncology, referring to cancers of the urinary tracts and male reproductive organs. Among the 61 sample videos examined by the researchers, health care practitioners contributed the content in 29, or 47 percent, of them. Yet, 22 posts, 36 percent, were misinformative, mostly due to outdated information.
More than half of the videos offered good content on disease symptoms and examinations. The authors concluded that “most videos on genitourinary cancers on TikTok are of poor to medium quality and reliability. However, videos posted by media agencies enjoyed great public attention and interaction. Medical practitioners could improve the video quality by cooperating with media agencies and avoiding unexplained terminologies.”
When health care providers post on social media, they must bear in mind that they have legal and ethical duties to their patients, profession and society, said Elizabeth Levy, founder and director of Physicians for Justice in Irvine, Calif., a nonprofit network of volunteer physicians partnering with public interest lawyers to address the social determinants of health.
“Providers are also responsible for understanding the mechanics of their posts,” such as who can see these messages and how long they stay up, Levy said. As a starting point for figuring what’s acceptable, providers could look at social media guidelines put out by their professional associations. Even beyond that, though, they must exercise prudent judgment. “As social media continues to evolve, providers will also need to stay updated with the changing risks and benefits of participation.”
Patients often research their providers online, so finding them on social media can help inform about values and approaches to care, said M. Sara Rosenthal, a professor and founding director of the program for bioethics and chair of the hospital ethics committee at the University of Kentucky College of Medicine.
Health care providers’ posts on social media also could promote patient education. They can advance informed consent and help patients navigate the risks and benefits of various treatments or preventive options. However, providers could violate ethical principles if they espouse “harmful, risky or questionable therapies or medical advice that is contrary to clinical practice guidelines or accepted standards of care,” Rosenthal said.
Inappropriate self-disclosure also can affect a provider’s reputation, said Kelly Michelson, a professor of pediatrics and director of the Center for Bioethics and Medical Humanities at Northwestern University’s Feinberg School of Medicine. A clinician’s obligations to professionalism extend beyond those moments when they are directly taking care of their patients, she said. “Many experts recommend against clinicians ‘friending’ patients or the families on social media because it blurs the patient-clinician boundary.”
Meanwhile, clinicians need to adhere closely to confidentiality. In sharing a patient’s case online for educational purposes, safeguarding identity becomes paramount. Removing names and changing minor details is insufficient, Michelson said.
“The patient-clinician relationship is sacred, and it can only be effective if patients have 100 percent confidence that all that happens with their clinician is kept in the strictest of confidence,” she said, adding that health care providers also should avoid obtaining information about their patients from social media because it can lead to bias and risk jeopardizing objectivity.
Academic clinicians can use social media as a recruitment tool to expand the pool of research participants for their studies, Michelson said. Because the majority of clinical research is conducted at academic medical centers, large segments of the population are excluded. “This affects the quality of the data and knowledge we gain from research,” she said.
Don S. Dizon, a professor of medicine and surgery at the Warren Alpert Medical School of Brown University in Providence, Rhode Island, uses LinkedIn and Doximity, as well as Twitter, Instagram, TikTok, Facebook, and most recently, YouTube and Post. He’s on Twitter nearly every day, where he interacts with the oncology community and his medical colleagues.
Also, he said, “I really like Instagram. It’s where you will see a hybrid of who I am professionally and personally. I’ve become comfortable sharing both up to a limit, but where else can I combine my appreciation of clothes with my professional life?” On that site, he’s seen sporting shirts with polka dots or stripes and an occasional bow-tie. He also posts photos of his cats.

Don S. Dizon, a professor of medicine and surgery at Brown, started using TikTok several years ago, telling medical stories in short-form videos.
Don S. Dizon
Dizon started using TikTok several years ago, telling medical stories in short-form videos. He may talk about an inspirational patient, his views on end-of-life care and death, or memories of people who have passed. But he is careful not to divulge any details that would identify anyone.
Recently, some people have become his patients after viewing his content on social media or on the Internet in general, which he clearly states isn’t a forum for medical advice. “In both situations, they are so much more relaxed when we meet, because it’s as if they have a sense of who I am as a person,” Dizon said. “I think that has helped so much in talking through a cancer diagnosis and a treatment plan, and yes, even discussions about prognosis.”
He also posts about equity and diversity. “I have found myself more likely to repost or react to issues that are inherently political, including racism, homophobia, transphobia and lack-of-access issues, because medicine is not isolated from society, and I truly believe that medicine is a social justice issue,” said Dizon, who is vice chair of diversity, equity, inclusion and professional integrity at the SWOG Cancer Research Network.
Through it all, Dizon likes “to break through the notion of doctor as infallible and all-knowing, the doctor as deity,” he said. “Humanizing what I do, especially in oncology, is something that challenges me on social media, and I appreciate the opportunities to do it on TikTok.”

