Antibody Testing Alone is Not the Key to Re-Opening Society
Immunity tests have too many unknowns right now to make them very useful in determining protective antibody status.
[Editor's Note: We asked experts from different specialties to weigh in on a timely Big Question: "How should immunity testing play a role in re-opening society?" Below, a virologist offers her perspective.]
With the advent of serology testing and increased emphasis on "re-opening" America, public health officials have begun considering whether or not people who have recovered from COVID-19 can safely re-enter the workplace.
"Immunity certificates cannot certify what is not known."
Conventional wisdom holds that people who have developed antibodies in response to infection with SARS-CoV-2, the coronavirus that causes COVID-19, are likely to be immune to reinfection.
For most acute viral infections, this is generally true. However, SARS-CoV-2 is a new pathogen, and there are currently many unanswered questions about immunity. Can recovered patients be reinfected or transmit the virus? Does symptom severity determine how protective responses will be after recovery? How long will protection last? Understanding these basic features is essential to phased re-opening of the government and economy for people who have recovered from COVID-19.
One mechanism that has been considered is issuing "immunity certificates" to individuals with antibodies against SARS-CoV-2. These certificates would verify that individuals have already recovered from COVID-19, and thus have antibodies in their blood that will protect them against reinfection, enabling them to safely return to work and participate in society. Although this sounds reasonable in theory, there are many practical reasons why this is not a wise policy decision to ease off restrictive stay-home orders and distancing practices.
Too Many Scientific Unknowns
Serology tests measure antibodies in the serum—the liquid component of blood, which is where the antibodies are located. In this case, serology tests measure antibodies that specifically bind to SARS-CoV-2 virus particles. Usually when a person is infected with a virus, they develop antibodies that can "recognize" that virus, so the presence of SARS-CoV-2 antibodies indicates that a person has been previously exposed to the virus. Broad serology testing is critical to knowing how many people have been infected with SARS-CoV-2, since testing capacity for the virus itself has been so low.
Tests for the virus measure amounts of SARS-CoV-2 RNA—the virus's genetic material—directly, and thus will not detect the virus once a person has recovered. Thus, the majority of people who were not severely ill and did not require hospitalization, or did not have direct contact with a confirmed case, will not test positive for the virus weeks after they have recovered and can only determine if they had COVID-19 by testing for antibodies.
In most cases, for most pathogens, antibodies are also neutralizing, meaning they bind to the virus and render it incapable of infecting cells, and this protects against future infections. Immunity certificates are based on the assumption that people with antibodies specific for SARS-CoV-2 will be protected against reinfection. The problem is that we've only known that SARS-CoV-2 existed for a little over four months. Although studies so far indicate that most (but not all) patients with confirmed COVID-19 cases develop antibodies, we don't know the extent to which antibodies are protective against reinfection, or how long that protection will last. Immunity certificates cannot certify what is not known.
The limited data so far is encouraging with regard to protective immunity. Most of the patient sera tested for antibodies show reasonable titers of IgG, the type of antibodies most likely to be neutralizing. Furthermore, studies have shown that these IgG antibodies are capable of neutralizing surrogate viruses as well as infectious SARS-CoV-2 in laboratory tests. In addition, rhesus monkeys that were experimentally infected with SARS-CoV-2 and allowed to recover were protected from reinfection after a subsequent experimental challenge. These data tentatively suggest that most people are likely to develop neutralizing IgG, and protective immunity, after being infected by SARS-CoV-2.
However, not all COVID-19 patients do produce high levels of antibodies specific for SARS-CoV-2. A small number of patients in one study had no detectable neutralizing IgG. There have also been reports of patients in South Korea testing PCR positive after a prior negative test, indicating reinfection or reactivation. These cases may be explained by the sensitivity of the PCR test, and no data have been produced to indicate that these cases are genuine reinfection or recurrence of viral infection.
Complicating matters further, not all serology tests measure antibody titers. Some rapid serology tests are designed to be binary—the test can either detect antibodies or not, but does not give information about the amount of antibodies circulating. Based on our current knowledge, we cannot be certain that merely having any level of detectable antibodies alone guarantees protection from reinfection, or from a subclinical reinfection that might not cause a second case of COVID-19, but could still result in transmission to others. These unknowns remain problematic even with tests that accurately detect the presence of antibodies—which is not a given today, as many of the newly available tests are reportedly unreliable.
A Logistical and Ethical Quagmire
While most people are eager to cast off the isolation of physical distancing and resume their normal lives, mere desire to return to normality is not an indicator of whether those antibodies actually work, and no certificate can confer immune protection. Furthermore, immunity certificates could lead to some complicated logistical and ethical issues. If antibodies do not guarantee protective immunity, certifying that they do could give antibody-positive people a false sense of security, causing them to relax infection control practices such as distancing and hand hygiene.
"We should not, however, place our faith in assumptions and make return to normality contingent on an arbitrary and uninformative piece of paper."
Certificates could be forged, putting susceptible people at higher exposure risk. It's not clear who would issue them, what they would entitle the bearer to do or not do, or how certification would be verified or enforced. There are many ways in which such certificates could be used as a pretext to discriminate against people based on health status, in addition to disability, race, and socioeconomic status. Tracking people based on immune status raises further concerns about privacy and civil rights.
Rather than issuing documents confirming immune status, we should instead "re-open" society cautiously, with widespread virus and serology testing to accurately identify and isolate infected cases rapidly, with immediate contact tracing to safely quarantine and monitor those at exposure risk. Broad serosurveillance must be coupled with functional assays for neutralization activity to begin assessing how protective antibodies might actually be against SARS-CoV-2 infection. To understand how long immunity lasts, we should study antibodies, as well as the functional capabilities of other components of the larger immune system, such as T cells, in recovered COVID-19 patients over time.
We should not, however, place our faith in assumptions and make return to normality contingent on an arbitrary and uninformative piece of paper. Re-opening society, the government, and the economy depends not only on accurately determining how many people have antibodies to SARS-CoV-2, but on a deeper understanding of how those antibodies work to provide protection.
Tapping into the Power of the Placebo Effect
When Wayne Jonas was in medical school 40 years ago, doctors would write out a prescription for placebos, spelling it out backwards in capital letters, O-B-E-C-A-L-P. The pharmacist would fill the prescription with a sugar pill, recalls Jonas, now director of integrative health programs at the Samueli Foundation. It fulfilled the patient's desire for the doctor to do something when perhaps no drug could help, and the sugar pills did no harm.
Today, that deception is seen as unethical. But time and time again, studies have shown that placebos can have real benefits. Now, researchers are trying to untangle the mysteries of placebo effect in an effort to better treat patients.
The use of placebos took off in the post-WWII period, when randomized controlled clinical trials became the gold standard for medical research. One group in a study would be treated with a placebo, a supposedly inert pill or procedure that would not affect normal healing and recovery, while another group in the study would receive an "active" component, most commonly a pill under investigation. Presumably, the group receiving the active treatment would have a better response and the difference from the placebo group would represent the efficacy of the drug being tested. That was the basis for drug approval by the U.S. Food and Drug Administration.
"Placebo responses were marginalized," says Ted Kaptchuk, director of the Program in Placebo Studies & Therapeutic Encounters at Harvard Medical School. "Doctors were taught they have to overcome it when they were thinking about using an effective drug."
But that began to change around the turn of the 21st century. The National Institutes of Health held a series of meetings to set a research agenda and fund studies to answer some basic questions, led by Jonas who was in charge of the office of alternative medicine at the time. "People spontaneously get better all the time," says Kaptchuk. The crucial question was, is the placebo effect real? Is it more than just spontaneous healing?
Brain mechanisms
A turning point came in 2001 in a paper in Science that showed physical evidence of the placebo effect. It used positron emission tomography (PET) scans to measure release patterns of dopamine — a chemical messenger involved in how we feel pleasure — in the brains of patients with Parkinson's disease. Surprisingly, the placebo activated the same patterns that were activated by Parkinson's drugs, such as levodopa. It proved the placebo effect was real; now the search was on to better understand and control it.
A key part of the effect can be the beliefs, expectations, context, and "rituals" of the encounter between doctor and patient. Belief by the doctor and patient that the treatment would work, and the formalized practices of administering the treatment can all contribute to a positive outcome.
Conditioning can be another important component in generating a response, as Pavlov demonstrated more than a century ago in his experiments with dogs. They were trained with a bell prior to feeding such that they would begin to salivate in anticipation at the sound of a bell even with no food present.
Translating that to humans, studies with pain medications and sleeping aids showed that patients who had a positive response with a certain dose of those medications could have the same response if the doses was reduced and a dummy pill substituted, even to the point where there was no longer any active ingredient.
Researchers think placebo treatments can work particularly well in helping people deal with pain and psychological disorders.
Those types of studies troubled Kaptchuk because they often relied on deception; patients weren't told they were receiving a placebo, or at best there was a possibility that they might be randomized to receive a placebo. He believed the placebo effect could work even if patients were told upfront that they were going to receive a placebo. More than a dozen so call "open-label placebo" studies across numerous medical conditions, by Kaptchuk and others, have shown that you don't have to lie to patients for a placebo to work.
Jonas likes to tell the story of a patient who used methotrexate, a potent immunosuppressant, to control her rheumatoid arthritis. She was planning a long trip and didn't want to be bothered with the injections and monitoring required in using the drug, So she began to drink a powerful herbal extract of anise, a licorice flavor that she hated, prior to each injection. She reduced the amount of methotrexate over a period of months and finally stopped, but continued to drink the anise. That process had conditioned her body "to alter her immune function and her autoimmunity" as if she were taking the drug, much like Pavlov's dogs had been trained. She has not taken methotrexate for more than a year.
An intriguing paper published in May 2021 found that mild, non-invasive electric stimulation to the brain could not only boost the placebo effect on pain but also reduce the "nocebo" effect — when patients report a negative effect to a sham treatment. While the work is very preliminary, it may open the door to directly manipulating these responses.
Researchers think placebo treatments can work particularly well in helping people deal with pain and psychological disorders, areas where drugs often are of little help. Still, placebos aren't a cure and only a portion of patients experience a placebo effect.
Nocebo
If medicine were a soap opera, the nocebo would be the evil twin of the placebo. It's what happens when patients have adverse side effects because of the expectation that they will. It's commonly seem when patients claims to experience pain or gastric distress that can occur with a drug even when they've received a placebo. The side effects were either imagined or caused by something else.
"Up to 97% of reported pharmaceutical side effects are not caused by the drug itself but rather by nocebo effects and symptom misattribution," according to one 2019 paper.
One way to reduce a nocebo response is to simply not tell patients that specific side effects might occur. An example is a liver biopsy, in which a large-gauge needle is used to extract a tissue sample for examination. Those told ahead of time that they might experience some pain were more likely to report pain and greater pain than those who weren't offered this information.
Interestingly, a nocebo response plays out in the hippocampus, a part of the brain that is never activated in a placebo response. "I think what we are dealing with with nocebo is anxiety," says Kaptchuk, but he acknowledges that others disagree.
Distraction may be another way to minimize the nocebo effect. Pediatricians are using virtual reality (VR) to engage children and distract them during routine procedures such as blood draws and changing wound dressings, and burn patients of all ages have found relief with specially created VRs.
Treatment response
Jonas argues that what we commonly call the placebo effect is misnamed and leading us astray. "The fact is people heal and that inherent healing capacity is both powerful and influenced by mental, social, and contextual factors that are embedded in every medical encounter since the idea of treatment began," he wrote in a 2019 article in the journal Frontiers in Psychiatry. "Our understanding of healing and ability to enhance it will be accelerated if we stop using the term 'placebo response' and call it what it is—the meaning response, and its special application in medicine called the healing response."
He cites evidence that "only 15% to 20% of the healing of an individual or a population comes from health care. The rest—nearly 80%—comes from other factors rarely addressed in the health care system: behavioral and lifestyle choices that people make in their daily life."
To better align treatments and maximize their effectiveness, Jonas has created HOPE (Healing Oriented Practices & Environments) Note, "a patient-guided process designed to identify the patient's values and goals in their life and for healing." Essentially, it seeks to make clear to both doctor and patient what the patient's goals are in seeking treatment. In an extreme example of terminal cancer, some patients may choose to extend life despite the often brutal treatments, while others might prefer to optimize quality of life in the remaining time that they have. It builds on practices already taught in medical schools. Jonas believes doctors and patients can use tools like these to maximize the treatment response and achieve better outcomes.
Much of the medical profession has been resistant to these approaches. Part of that is simply tradition and limited data on their effectiveness, but another very real factor is the billing process for how they are reimbursed. Jonas says a new medical billing code added this year gives doctors another way to be compensated for the extra time and effort that a more holistic approach to medicine may initially require. Other moves away from fee-for-service payments to bundling and payment for outcomes, and the integrated care provided by the Veterans Affairs, Kaiser Permanente and other groups offer longer term hope for the future of approaches that might enhance the healing response.
This article was first published by Leaps.org on July 7, 2021.
New tech helps people of all ages stay social
Sonja Bauman, 39, and Mariela Florez, 83, taking one of their regular walks in Plantation, Fla. The pair met through an online platform called Papa that provides "family on demand." (Photo by Sonja Bauman)
In March, Sonja Bauman, 39, used an online platform called Papa, which offers “family on demand,” to meet Mariela Florez, an 83-year-old retiree. Despite living with her adult children, Florez was bored and lonely when they left for work, and her recoveries from a stroke and broken hip were going slowly. That's when Bauman began visiting twice per week. They take walks, strengthening Florez’s hip, and play games like Connect Four for mental stimulation. “It’s very important for me so I don’t feel lonely all day long,” said Florez. Her memories, blurred by the stroke, are gradually returning.
Papa is one of a growing number of tech approaches that are bringing together people of all ages. In addition to platforms like Papa that connect people in real life, other startups use virtual reality and video, with some of them focusing especially on deepening social connections between the generations — relationships that support the health of older and younger people alike. “I enjoy seeing Mariela as much as she enjoys seeing me,” Bauman said.
Connecting in real life
Telehealth expert Andrew Parker founded Papa in 2017 to improve the health outcomes of older adults and families. Seniors can meet people — some their grandkids’ age — for healthy activities, while working parents find retirees to watch their children. These “Papa Pals” are provided as a benefit through Medicare, Medicaid and some employer health plans.
In 2020, Papa connected Bauman, the 39-year-old Floridian, with another woman in her mid-70s who lives alone and has very limited mobility. Bauman began driving her to doctor’s appointments and helping her with chores around the house. “When I’m not there, she doesn’t leave her apartment,” said Bauman. The two have gone to the gym together, and they walk slowly through the neighborhood, chatting so it feels less like exercise.
Parker was driven to start Papa by the problem of social isolation among seniors, exacerbated by the pandemic, but he believes users of all ages can benefit. “Many of our Pals feel more comfortable opening up with older members than their same-aged friends,” he said.
Other platforms aim for similar, in-person connections. Generation Tech unites teens with seniors for technology training. And Mon Ami, which provides case management software for aging and disability service providers, has an app that connects isolated older people with college-age volunteers.
Making new connections through video
Several new sites match you with strangers for real-time video chatting on various topics, such as finding common ground on political issues. Other video platforms focus on intergenerational connections.
S. Jay Olshansky, a gerontology professor at the University of Illinois-Chicago, recalls the first time he saw Hyunseung Lee, an 11-year-old from Seoul, through his computer screen. The kid was shy, but Olshansky, 67, encouraged him to ask questions. “Turns out, he was thirsting for this kind of interaction.”
They’d connected through Eldera, a platform that pairs mentors age 60 and up with mentees, using an algorithm, for video conversations. “The time and wisdom of older adults is the most important natural resource we can give future generations,” said Dana Griffin, Eldera's CEO. “Connecting through a screen is the opposite of social media.”
In weekly meetings, Olshansky noticed Lee’s unique interest in math. “There’s something special in you,” Olshansky told him. “How do we bring it to the surface?” He suggested Lee write a book on his favorite subject, and the preteen ran with it, cranking out 70 pages in two weeks. Lee has published his love letter to theorems on Amazon.
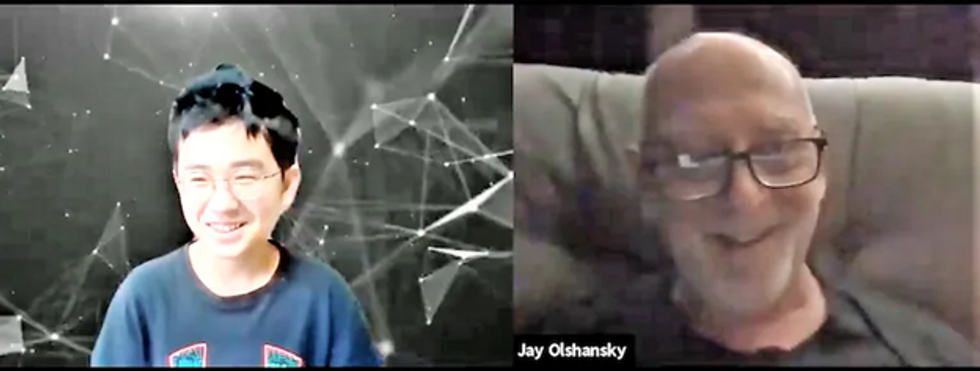
Hyunseung Lee, age 11, of Korea, and U.S. college professor Jay Olshanksy, 67, discuss math, strategy and Hyunsung's budding career as a book author during their video chats through a platform called Eldera. (Photo by Dana Palmer/Eldera)
Lee’s parents told Olshansky that their son has become more assertive — a recurring theme, Griffin said. “Confidence is the number one thing parents tell us about.” Since Eldera’s inception last year, the number of mentors has grown exponentially. Even so, Griffin said the waitlist for mentors typically numbers 200 kids.
Another site, Big and Mini, hosts video interactions between seniors and young adults; about 10,000 active users have joined since 2019, said co-founder Aditi Merchant.
Users often bring the benefits of their video interactions to their real-world relationships. Olshansky views Lee as an older version of his grandkids. “Eldera teaches me how to interact with them.” Lee, high on confidence, began instructing his classmates in math. Griffin noted that a group of Eldera mentors in Memphis, who met initially on Eldera, now take walks together in-person to trade ideas for helping each other’s Eldera kids solve problems in their schools and communities.
“We’ve evolved into a community for older adults who want to give back to the world,” said Griffin. Other new tools for connection take the form of virtual reality apps.
Connecting in virtual reality
During pandemic isolation, record numbers of people bought devices for virtual and augmented reality. Such gadgets can convince you that you’re hanging out with friends, even if they’re in another hemisphere. Lifelike simulations from miles away could be especially useful for meaningful interactions between people of different generations, since they’re often geographically segregated.
VR’s benefits require further study, but users report less social isolation and depression, according to MIT research. The immersive, 3-D experience is more compelling than FaceTime or Zoom. “It’s like the difference between a phone call and video call,” said Rick Robinson, Vice President of AARP’s Innovation Labs.
“When VR is designed right, the medium disappears,” said Jeremy Bailenson of Stanford.
Dana Pierce, a 56-year-old government employee in Indiana, got Meta's VR headset in May, 2021, thinking she’d enjoy it more than a new laptop. After many virtual group tours of exotic destinations, she has no regrets. Her adventures occur on Alcove, an app made by Robinson’s Innovation Labs. He co-created it with VR-company Rendever and sought input from people over age 50 to tailor it to their interests. “I’m an introvert,” said Pierce. “I’ve been more socially active since getting my headset than I am in real life.”
Tagging along with her to places like Paris are avatars representing real people around the world. She’s gotten to know VR users in their 70s, 80s and 90s, as well as younger people and some her own age. One is a new friend she plays chess with in relaxing nature settings. Another is her oldest son. He lives 90 minutes away but, earlier this year, Pierce welcomed him and his girlfriend to her virtual house on Alcove. They chatted in the living room decorated with family photos uploaded by Pierce. Then they took out a boat to go VR fishing — because why not — until 2 a.m.
“When VR is designed right, the medium disappears,” said Jeremy Bailenson, a communications professor who directs Stanford’s Virtual Human Interaction Lab. He’s teaching a class of 175 students entirely in VR. After months of covid isolation, the first time the class met, “there was a big catharsis. It really feels like you’re in a big crowd.” Like-minded people meet in VR for events such as comedy shows and creative writing meetups, while the Swedish pop group ABBA has performed this year as digital versions of themselves (“ABBA-tars”) during a virtual concert tour.
Karen Fingerman, a psychologist and director of the Texas Aging and Longevity Center at the University of Texas-Austin, supports the idea of VR for social connection, though she added that some people need it more than others. Hospitals and assisted-living facilities are using products such as Penumbra’s REAL I-Series and MyndVR to bring VR excursions to isolated patients and seniors. “If you’re in a bed or facility, this gives you something to talk about,” said Gita Barry, Penumbra’s executive vice president.
Pierce uses it on most days. She may see another adult son, who lives with her, less often as a result. But VR helps her manage real-world stressors, more than escaping them. After a long workday, she visits her back porch on Alcove, which overlooks a pond. “It’s my little retreat,” she said. “VR improves my mood. It’s added a lot to my life.”
Some seniors are using more than one technology. Olshansky and Lee discuss strategy while playing Internet chess. And Olshansky recently began using VR. He sees his sister, who lives far away, in a virtual beach house. “It’d be a great way to interact with Hyunseung,” he said. “I should get him a headset.”
A version of this article first appeared in The Washington Post on December 3, 2021.

