An Electrifying Idea For Roads

Companies such as Wave and Magment offer a variety of approaches for charging vehicles without plugs while they're being stored or even used, but costs stand in the way of broader adoption.
Starting this summer, the public buses in the Oberhaching suburb of Munich, Germany, won’t have to be plugged in to charge overnight anymore. Stefan Schelle, the mayor of Oberhaching, is taking advantage of the fact that an innovative startup has its offices in his community: Magment, short for “magnetizing cement,” will install its underground charging pad in the coming months. As soon as that happens, the buses will charge while they wait at the city’s main station or while stored at their overnight quarters.
In his light-filled office, Magment’s co-founder and CEO, Mauricio Esguerra, demonstrates how the new technology works: The lights on his black model car only flash when he puts the miniature Porsche directly atop the induction plate. “This works just like when you charge your iPhone on its charging pad or heat a pot on an induction range. People don’t have to be afraid of magnetic fields or anything like that,” says the 60-year-old Colombia-born entrepreneur. “The induction only gets activated when the storage battery is placed directly on top.
Patented by Esguerra, the “magnetizing concrete” is able to target the charge quite precisely. The batteries will be mounted in a box underneath the vehicles such as the retrofitted public buses. “Look, here’s one passing by,” says Esguerra, pointing out the window as a blue city bus rides past his office.
An invention finds its purpose
Esguerra grew up in Bogotá, studied physics at the Technical University Munich where he fell in love with a German woman, and started a family in her home country. For 15 years, he developed magnetic products, including the magnetizing cement, for Siemens, Europe’s largest industrial manufacturing company. The patent belonged to Siemens, of course. “But there were hardly any electric vehicles yet,” Esguerra says, “and Siemens didn’t quite know what to do with this invention.”
Esguerra changed companies a few times but, in 2015, he got an offer from Siemens. The patent for the magnetizing cement was expiring and Siemens wasn’t interested in keeping it. Would he, as the inventor, want it back? “I did not hesitate a second,” Esguerra remembers with a smile. “I’m a magnetician at heart.” That same year, he founded Magment to finally make use of the technology he created 20 years ago.
To demonstrate how his cement is made, he opens the lid of a plastic bucket filled with cement powder. Mixed in are fingernail-sized black pieces, so-called ferrites, mainly consisting of three ceramic oxides: iron, nickel and zinc. Conventionally, they are used in electronics such as cell phones, computers and cables. Molded in concrete, ferrites create a magnetic field that can transport charge to a vehicle, potentially eliminating range anxiety for EV drivers.

Molded in concrete, ferrites create a magnetic field that can transport charge to a vehicle, potentially eliminating range anxiety for EV drivers.
Magment
“Ferrites have extremely high rejection rates,” Esguerra adds. “It’s comparable to other ceramics: As soon as there is a small tear or crack, the material is rejected. We are talking about a rejection pile of 500,000 tons per year worldwide. There are mountains of unused materials.”
Exactly this fact was the starting point of his research at Siemens: “What can we do with this energy-intensive material? Back then, it was crushed up and mixed into the cement for building streets, without adding any function.” Today, too, the Magment material can simply be mixed with the conventional material and equipment of the cement industry. “We take advantage of the fact that we don’t have to build factories and don’t have high transportation costs."
In addition to saving resources, recycled ferrite also makes concrete more durable.
No plugs, no charging breaks
A young intern in the office next door winds cables around a new coil. These coils will later be lowered underground in a box, connected to the grid and encased in magnetizing concrete. The recipient box looks similar; it’s another coil but smaller, and it will be mounted underneath the carriage of the vehicle. For a car, the battery box would be 25 by 25 centimeters (about 10 inches), for a scooter five by five centimeters (about two inches).
Esguerra pushes an electric scooter into a cemented scooter rack next to his office. The charging pad is invisible. A faint beep is the only sign that it has started charging. “Childs play!” Esguerra says. “Even when someone puts in the scooter a little crooked, the charge still works. Our efficiency rate is up to 96 percent.” From this summer on, hotel chains in Munich will try out this system with their rental scooters, at a price of about 500 Euros per charging station.
Compared to plug-in charging, Magment’s benefits include smaller batteries that charge slower and, therefore, gentler, so they may last longer. Nobody needs to plug in the vehicles manually anymore. “Personally, I’ve had an EV for six years,” Esguerra says, “and how often does it happen that I forgot to plug it in overnight and then start out with a low charge in the morning? Once people get used to the invisible charging system, it will become the norm.“
There are also downsides: Most car companies aren’t ready for the new technology. Hyundai is the first carmaker that announced plans to equip some new models with inductive charging capability. “How many cars are electrified worldwide?” Esguerra asks and gives the answer himself: “One percent. And how many forklifts are electrified? More than 70 percent!” Therefore, Magment focuses on charging forklifts, e-scooters and buses.

Magment has focused most of its efforts on charging forklifts and other vehicle types that are entirely or predominantly electric, unlike cars.
Magment
On the morning of my visit to Esguerra’s office, a developer of the world’s third-biggest forklift manufacturer is there to inspect how the technology works on the ground. In the basement, a Magment engineer drives an electric forklift over a testbed with invisible charging coils, turning on the green charging light. Esguerra opens the interior of the forklift and points out the two batteries. “With our system, the forklift will only need one battery.” The savings, about 7,000 Euro per forklift, will pay for the installation of Magment’s charging system in warehouses, Esguerra calculates. “Less personnel and no unnecessary wait times for charging will lead to further savings,” he says.
To implement the new technology as efficiently as possible, Magment engineers began recording the transport routes of forklifts in warehouses. “It looks like spaghetti diagrams,” Esguerra explains. “Soon you get the areas where the forklifts pass or wait most frequently. This is where you install the chargers underground.” The forklifts will charge while in use, without having to pause for charging breaks. The method could also work for robots, for instance, in warehouses and distribution centers.
Roads of the future could be electric
Potential disadvantages might become apparent once the technology is more broadly in use. Therefore investors were initially reluctant, Esguerra admits. “Some are eager to be the first but most prefer to wait until the technology has been extensively used in real life.”
A clear hurdle today is that electrifying entire freeways with induction coils would cost at least 1 to 1.5 million Euros per kilometer. The German Department for Transportation even calculates overall costs of 14 to 47 million Euros per kilometer. So, the technology may only make sense for areas where vehicles pass or dwell the longest, like the Oberhaching train station or a busy interstate toll booth.
And yet, Magment is ramping up to compete with other companies that build larger inductive charging pads. The company just finished the first 20 meters of a testbed in Indiana, in partnership with the Purdue University and the Indiana Department of Transportation. Magment is poised to build “the world’s first contactless wireless-charging concrete pavement highway segment,” Purdue University announced.
The project, part of Purdue’s ASPIRE (Advancing Sustainability through Powered Infrastructure for Roadway Electrification) program, is financed by the National Science Foundation. “Indiana is known as the Crossroads of America, and we’re committed to fortifying our position as a transportation leader by innovating to support the emerging vehicle technology,” Governor Eric J. Holcomb said. If testing is successful, including the concrete’s capacity to charge heavy trucks operating at higher power (200 kilowatts and above), Indiana plans to identify a highway segment to install Magment’s charging pads. The earliest would be 2023 at best.
In the meantime, buses in the Californian Antelope Valley, trams at Hollywood's Universal Studios and transit buses in Tampa, Florida, are already charging with inductive technology developed by Wave, a company spun out of Utah State University. In Michigan, Governor Gretchen Whitmer announced plans to build a test route for vehicles to charge while driving, in collaboration with the Israel-based company Electreon, and this year contracted to build the first road-based charging system in the U.S. The state is providing support through an innovative grant program.
Costs remain one of the biggest obstacles, but Esguerra’s vision includes the potential that toll roads could charge a premium for inductive charging capabilities. “And in reverse, a driver who has too much energy could feed his surplus into the grid while driving,” Esguerra dreams.
Meanwhile, Wave’s upcoming big projects are moving trucks along a route in Southern California and running a UPS route between Seattle and Portland. Wave CTO Michael Masquelier describes the inductive power transfer his company champions as “similar to a tuning fork. By vibrating that fork, you sent energy through the air and it is received by another tuning fork across the room. So it’s similar to that, but it’s magnetic energy versus sound energy.”
He hopes to partner with Magment, saying that “the magnetizing cement makes installation easier and improves the energy efficiency.” More research is needed to evaluate which company’s technology will prove to be the most efficient, practical, and cost-effective.
Esguerra’s vision includes the potential that toll roads could charge a premium for inductive charging capabilities. “And in reverse, a driver who has too much energy could feed his surplus into the grid while driving,” Esguerra dreams.
The future will soon arrive in the idyllic town of Bad Staffelstein, a quaint tourist destination in the Upper Franconia region of Germany. Visitors will be taken to and from the main station and the popular thermal bath by driverless shuttles. Together with the University of Wuppertal, the regional government of Upper Franconia wants to turn its district into “the center of autonomous driving.” Magment is about to install inductive charging pads at the shuttle stations and the thermal bath, eliminating the need for the shuttles to stop for charging times. No more drivers, no cable, no range anxiety. Masquelier believes that “wireless and autonomous driving go hand in hand.” Science fiction? It will become science reality in spring 2023.
CORRECTION: An earlier version of the story erroneously mentioned that Electreon required overhead cables.
Scientists Are Working to Develop a Clever Nasal Spray That Tricks the Coronavirus Out of the Body
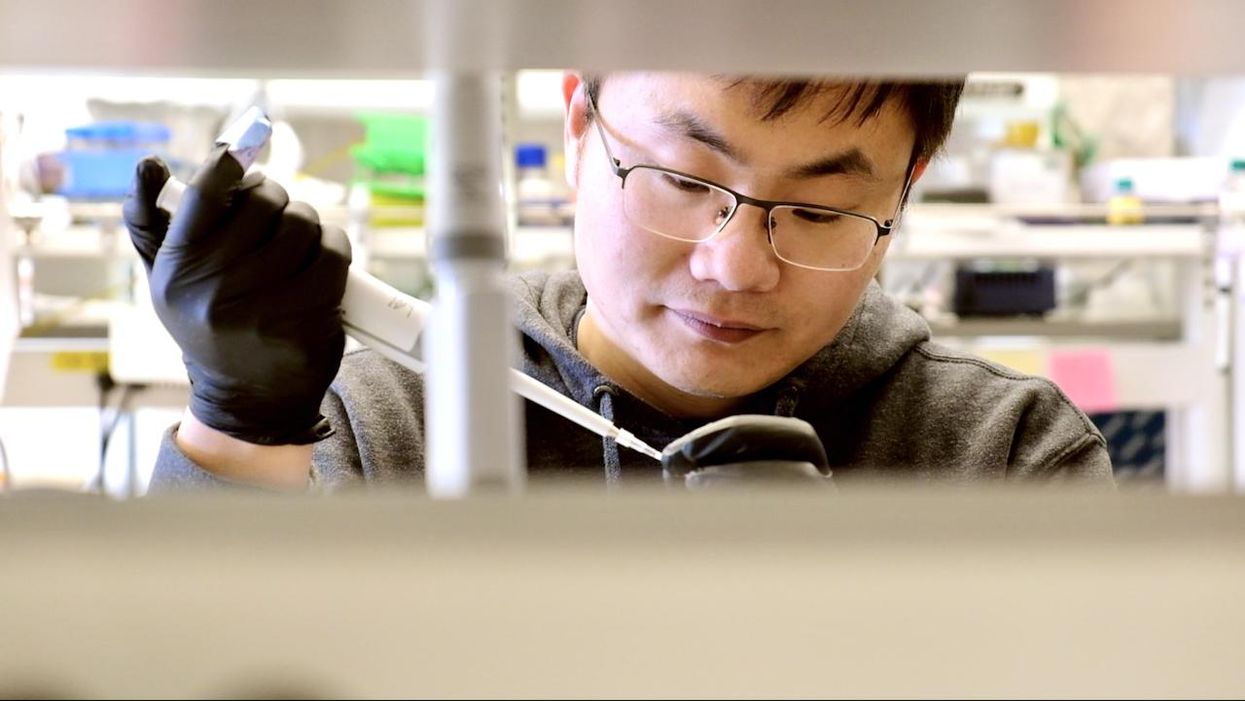
Biochemist Longxing Cao is working with colleagues at the University of Washington on promising research to disable infectious coronavirus in a person's nose.
Imagine this scenario: you get an annoying cough and a bit of a fever. When you wake up the next morning you lose your sense of taste and smell. That sounds familiar, so you head to a doctor's office for a Covid test, which comes back positive.
Your next step? An anti-Covid nasal spray of course, a "trickster drug" that will clear the once-dangerous and deadly virus out of the body. The drug works by tricking the coronavirus with decoy receptors that appear to be just like those on the surface of our own cells. The virus latches onto the drug's molecules "thinking" it is breaking into human cells, but instead it flushes out of your system before it can cause any serious damage.
This may sounds like science fiction, but several research groups are already working on such trickster coronavirus drugs, with some candidates close to clinical trials and possibly even becoming available late this year. The teams began working on them when the pandemic arrived, and continued in lockdown.
This may sounds like science fiction, but several research groups are already working on such trickster coronavirus drugs, with some candidates close to clinical trials and possibly even becoming available late this year. The teams began working on them when the pandemic arrived, and continued in lockdown.
When the pandemic first hit and the state of California issued a lockdown order on March 16, postdoctoral researchers Anum and Jeff Glasgow found themselves stuck at home with nothing to do. The two scientists who study bioengineering felt that they were well equipped to research molecular ways of disabling coronavirus's cell-penetrating spike protein, but they could no longer come to their labs at the University of California San Francisco.
"We were upset that no one put us in the game," says Anum Glasgow. "We have a lot of experience between us doing these types of projects so we wanted to contribute." But they still had computers so they began modeling the potential virus-disabling proteins in silico using Robetta, special software for designing and modeling protein structures, developed and maintained by University of Washington biochemist David Baker and his lab.
"We saw some imperfections in that lock and key and we created something better. We made a 10 times tighter adhesive."
The SARS-CoV-2 virus that causes Covid-19 uses its surface spike protein to bind on to a specific receptor on human cells called ACE2. Unfortunately for humans, the spike protein's molecular shape fits the ACE2 receptor like a well-cut key, making it very successful at breaking into our cells. But if one could design a molecular ACE2-mimic to "trick" the virus into latching onto it instead, the virus would no longer be able to enter cells. Scientists call such mimics receptor traps or inhibitors, or blockers. "It would block the adhesive part of the virus that binds to human cells," explains Jim Wells, professor of pharmaceutical chemistry at UCSF, whose lab took part in designing the ACE2-receptor mimic, working with the Glasgows and other colleagues.
The idea of disabling infectious or inflammatory agents by tricking them into binding to the targets' molecular look-alikes is something scientists have tried with other diseases. The anti-inflammatory drugs commonly used to treat autoimmune conditions, including rheumatoid arthritis, Crohn's disease and ulcerative colitis, rely on conceptually similar molecular mechanisms. Called TNF blockers, these drugs block the activity of the inflammatory cytokines, molecules that promote inflammation. "One of the biggest selling drugs in the world is a receptor trap," says Jeff Glasgow. "It acts as a receptor decoy. There's a TNF receptor that traps the cytokine."
In the recent past, scientists also pondered a similar look-alike approach to treating urinary tract infections, which are often caused by a pathogenic strain of Escherichia coli. An E. coli bacterium resembles a squid with protruding filaments equipped with proteins that can change their shape to form hooks, used to hang onto specific sugar molecules called ligands, which are present on the surface of the epithelial cells lining the urinary tract.
A recent study found that a sugar-like compound that's structurally similar to that ligand can play a similar trick on the E. Coli. When administered in in sufficient amounts, the compound hooks the bacteria on, which is then excreted out of the body with urine. The "trickster" method had been also tried against the HIV virus, but it wasn't very effective because HIV has a high mutation rate and multiple ways of entering human cells.
But the coronavirus spike protein's shape is more stable. And while it has a strong affinity for the ACE2 receptors, its natural binding to these receptors isn't perfect, which allowed the UCSF researchers to design a mimic with a better grip. "We saw some imperfections in that lock and key and we created something better," says Wells. "We made a 10 times tighter adhesive." The team demonstrated that their traps neutralized SARS-CoV-2 in lab experiments and published their study in the Proceedings of the National Academy of Sciences.
Baker, who is the director of the Institute for Protein Design at the University of Washington, was also devising ACE2 look-alikes with his team. Only unlike the UCSF team, they didn't perfect the virus-receptor lock and key combo, but instead designed their mimics from scratch. Using Robetta, they digitally modeled over two million proteins, zeroed-in on over 100,000 potential candidates and identified a handful with a strong promise of blocking SARS-CoV-2, testing them against the virus in human cells. Their design of the miniprotein inhibitors was published in the journal Science.

Biochemist David Baker, pictured in his lab at the University of Washington.
UW
The concept of the ACE2 receptor mimics is somewhat similar to the antibody plasma, but better, the teams explain. Antibodies don't always coat all of the virus's spike proteins and sometimes don't bind perfectly. By contrast, the ACE2 mimics directly compete with the virus's entry mechanism. ACE2 mimics are also easier and cheaper to make, researchers say.
Antibodies, which are long protein chains, must be grown inside mammalian cells, which is a slow and costly process. As drugs, antibody cocktails must be kept refrigerated. On the contrary, proteins that mimic ACE2 receptors are smaller and can be produced by bacteria easily and inexpensively. Designed to specs, these proteins don't need refrigeration and are easy to store. "We designed them to be very stable," says Baker. "Our computation design tries to come up with the stable proteins that have the desired functions."
That stability may allow the team to create an inhaler drug rather than an intravenous one, which would be another advantage over the antibody plasma, given via an IV. The team envisions people spraying the miniprotein solution into their nose, creating a protecting coating that would disable the inhaled virus. "The infection starts from your respiratory system, from your nose," explains Longxing Cao, the study's co-author—so a nasal spray would be a natural way to administer it. "So that you can have it like a layer, similar to a mask."
As the virus evolves, new variants are arising. But the teams think that their ACE2 protein mimics should work on the new variants too for several reasons. "Since the new SARS-CoV-2 variants still use ACE2 for their cell entry, they will likely still be susceptible to ACE2-based traps," Glasgow says.
Cao explains that their approach should work too because most of the mutations happen outside the ACE2 binding region. Plus, they are building multiple binders that can bind to an array of the coronavirus variants. "Our binder can still bind with most of the variants and we are trying to make one protein that could inhibit all the future escape variants," he says.
Baker and Cao hope that their miniproteins may be available to patients later this year. But besides getting the medicine out to patients, this approach will allow researchers to test the computer-modeled mimics end-to-end with an unprecedented speed. That would give humans a leg up in future pandemics or zoonotic disease outbreaks, which remain an increasingly pressing threat due to human activity and climate change.
"That's what we are focused on right now—understanding what we have learned from this pandemic to improve our design methods," says Baker. "So that we should be able to obtain binders like these very quickly when a new pandemic threat is identified."
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
How Will the New Strains of COVID-19 Affect Our Vaccination Plans?
The mutated strains that first arose in the U.K. and South Africa and have now spread to many countries are prompting urgent studies on the effectiveness of current vaccines to neutralize the new strains.
When the world's first Covid-19 vaccine received regulatory approval in November, it appeared that the end of the pandemic might be near. As one by one, the Pfizer/BioNTech, Moderna, AstraZeneca, and Sputnik V vaccines reported successful Phase III results, the prospect of life without lockdowns and restrictions seemed a tantalizing possibility.
But for scientists with many years' worth of experience in studying how viruses adapt over time, it remained clear that the fight against the SARS-CoV-2 virus was far from over. "The more virus circulates, the more it is likely that mutations occur," said Professor Beate Kampmann, director of the Vaccine Centre at the London School of Hygiene & Tropical Medicine. "It is inevitable that new variants will emerge."
Since the start of the pandemic, dozens of new variants of SARS-CoV-2 – containing different mutations in the viral genome sequence - have appeared as it copies itself while spreading through the human population. The majority of these mutations are inconsequential, but in recent months, some mutations have emerged in the receptor binding domain of the virus's spike protein, increasing how tightly it binds to human cells. These mutations appear to make some new strains up to 70 percent more transmissible, though estimates vary and more lab experiments are needed. Such new strains include the B.1.1.7 variant - currently the dominant strain in the UK – and the 501Y.V2 variant, which was first found in South Africa.
"I'm quite optimistic that even with these mutations, immunity is not going to suddenly fail on us."
Because so many more people are becoming infected with the SARS-CoV-2 virus as a result, vaccinologists point out that these new strains will prolong the pandemic.
"It may take longer to reach vaccine-induced herd immunity," says Deborah Fuller, professor of microbiology at the University of Washington School of Medicine. "With a more transmissible variant taking over, an even larger percentage of the population will need to get vaccinated before we can shut this pandemic down."
That is, of course, as long as the vaccinations are still highly protective. The South African variant, in particular, contains a mutation called E484K that is raising alarms among scientists. Emerging evidence indicates that this mutation allows the virus to escape from some people's immune responses, and thus could potentially weaken the effectiveness of current vaccines.
What We Know So Far
Over the past few weeks, manufacturers of the approved Covid-19 vaccines have been racing to conduct experiments, assessing whether their jabs still work well against the new variants. This process involves taking blood samples from people who have already been vaccinated and assessing whether the antibodies generated by those people can neutralize the new strains in a test tube.
Pfizer has just released results from the first of these studies, declaring that their vaccine was found to still be effective at neutralizing strains of the virus containing the N501Y mutation of the spike protein, one of the mutations present within both the UK and South African variants.
However, the study did not look at the full set of mutations contained within either of these variants. Earlier this week, academics at the Fred Hutchinson Cancer Research Center in Seattle suggested that the E484K spike protein mutation could be most problematic, publishing a study which showed that the efficacy of neutralizing antibodies against this region dropped by more than ten-fold because of the mutation.
Thankfully, this development is not expected to make vaccines useless. One of the Fred Hutch researchers, Jesse Bloom, told STAT News that he did not expect this mutation to seriously reduce vaccine efficacy, and that more harmful mutations would need to accrue over time to pose a very significant threat to vaccinations.
"I'm quite optimistic that even with these mutations, immunity is not going to suddenly fail on us," Bloom told STAT. "It might be gradually eroded, but it's not going to fail on us, at least in the short term."
While further vaccine efficacy data will emerge in the coming weeks, other vaccinologists are keen to stress this same point: At most, there will be a marginal drop in efficacy against the new variants.
"Each vaccine induces what we call polyclonal antibodies targeting multiple parts of the spike protein," said Fuller. "So if one antibody target mutates, there are other antibody targets on the spike protein that could still neutralize the virus. The vaccine platforms also induce T-cell responses that could provide a second line of defense. If some virus gets past antibodies, T-cell responses can find and eliminate infected cells before the virus does too much damage."
She estimates that if vaccine efficacy decreases, for example from 95% to 85%, against one of the new variants, the main implications will be that some individuals who might otherwise have become severely ill, may still experience mild or moderate symptoms from an infection -- but crucially, they will not end up in intensive care.
"Plug and Play" Vaccine Platforms
One of the advantages of the technologies which have been pioneered to create the Covid-19 vaccines is that they are relatively straightforward to update with a new viral sequence. The mRNA technology used in the Pfizer/BioNTech and Moderna vaccines, and the adenovirus vectors used in the Astra Zeneca and Sputnik V vaccines, are known as 'plug and play' platforms, meaning that a new form of the vaccine can be rapidly generated against any emerging variant.
"With a rapid pipeline for manufacture established, these new vaccine technologies could enable production and distribution within 1-3 months of a new variant emerging."
While the technology for the seasonal influenza vaccines is relatively inefficient, requiring scientists to grow and cultivate the new strain in the lab before vaccines can be produced - a process that takes nine months - mRNA and adenovirus-based vaccines can be updated within a matter of weeks. According to BioNTech CEO Uğur Şahin, a new version of their vaccine could be produced in six weeks.
"With a rapid pipeline for manufacture established, these new vaccine technologies could enable production and distribution within 1-3 months of a new variant emerging," says Fuller.
Fuller predicts that more new variants of the virus are almost certain to emerge within the coming months and years, potentially requiring the public to receive booster shots. This means there is one key advantage the mRNA-based vaccines have over the adenovirus technologies. mRNA vaccines only express the spike protein, while the AstraZeneca and Sputnik V vaccines use adenoviruses - common viruses most of us are exposed to - as a delivery mechanism for genes from the SARS-CoV-2 virus.
"For the adenovirus vaccines, our bodies make immune responses against both SARS-CoV-2 and the adenovirus backbone of the vaccine," says Fuller. "That means if you update the adenovirus-based vaccine with the new variant and then try to boost people, they may respond less well to the new vaccine, because they already have antibodies against the adenovirus that could block the vaccine from working. This makes mRNA vaccines more amenable to repeated use."
Regulatory Unknowns
One of the key questions remains whether regulators would require new versions of the vaccine to go through clinical trials, a hurdle which would slow down the response to emerging strains, or whether the seasonal influenza paradigm will be followed, whereby a new form of the vaccine can be released without further clinical testing.
Regulators are currently remaining tight-lipped on which process they will choose to follow, until there is more information on how vaccines respond against the new variants. "Only when such information becomes available can we start the scientific evaluation of what data would be needed to support such a change and assess what regulatory procedure would be required for that," said Rebecca Harding, communications officer for the European Medicines Agency.
The Food and Drug Administration (FDA) did not respond to requests for comment before press time.
While vaccinologists feel it is unlikely that a new complete Phase III trial would be required, some believe that because these are new technologies, regulators may well demand further safety data before approving an updated version of the vaccine.
"I would hope if we ever have to update the current vaccines, regulatory authorities will treat it like influenza," said Drew Weissman, professor of medicine at the University of Pennsylvania, who was involved in developing the mRNA technology behind the Pfizer/BioNTech and Moderna vaccines. "I would guess, at worst, they may want a new Phase 1 or 1 and 2 clinical trials."
Others suggest that rather than new trials, some bridging experiments may suffice to demonstrate that the levels of neutralizing antibodies induced by the new form of the vaccine are comparable to the previous one. "Vaccines have previously been licensed by this kind of immunogenicity data only, for example meningitis vaccines," said Kampmann.
While further mutations and strains of SARS-CoV-2 are inevitable, some scientists are concerned that the vaccine rollout strategy being employed in some countries -- of distributing a first shot to as many people as possible, and potentially delaying second shots as a result -- could encourage more new variants to emerge. Just today, the Biden administration announced its intention to release nearly all vaccine doses on hand right away, without keeping a reserve for second shots. This plan risks relying on vaccine manufacturing to ramp up quickly to keep pace if people are to receive their second shots at the right intervals.
"I am not very happy about this change as it could lead to a large number of people out there with partial immunity and this could select new mutations, and escalate the potential problem of vaccine escape."
The Biden administration's shift appears to conflict with the FDA's recent position that second doses should be given on a strict schedule, without any departure from the three- and four-week intervals established in clinical trials. Two top FDA officials said in a statement that changing the dosing schedule "is premature and not rooted solidly in the available evidence. Without appropriate data supporting such changes in vaccine administration, we run a significant risk of placing public health at risk, undermining the historic vaccination efforts to protect the population from COVID-19."
"I understand the argument of trying to get at least partial protection to as many people as possible, but I am concerned about the increased interval between the doses that is now being proposed," said Kampmann. "I am not very happy about this change as it could lead to a large number of people out there with partial immunity and this could select new mutations, and escalate the potential problem of vaccine escape."
But it's worth emphasizing that the virus is unlikely for now to accumulate enough harmful mutations to render the current vaccines completely ineffective.
"It will be very hard for the virus to evolve to completely evade the antibody responses the vaccines induce," said Fuller. "The parts of the virus that are targeted by vaccine-induced antibodies are essential for the virus to infect our cells. If the virus tries to mutate these parts to evade antibodies, then it could compromise its own fitness or even abort its ability to infect. To be sure, the virus is developing these mutations, but we just don't see these variants emerge because they die out."