How old fishing nets turn into chairs, car mats and Prada bags
A company called Aquafil is turning the fibers from fishing nets and old carpets into new threads for chairs, car mats, bikinis and Prada bags.
Discarded nylon fishing nets in the oceans are among the most harmful forms of plastic pollution. Every year, about 640,000 tons of fishing gear are left in our oceans and other water bodies to turn into death traps for marine life. London-based non-profit World Animal Protection estimates that entanglement in this “ghost gear” kills at least 136,000 seals, sea lions and large whales every year. Experts are challenged to estimate how many birds, turtles, fish and other species meet the same fate because the numbers are so high.
Since 2009, Giulio Bonazzi, the son of a small textile producer in northern Italy, has been working on a solution: an efficient recycling process for nylon. As CEO and chairman of a company called Aquafil, Bonazzi is turning the fibers from fishing nets – and old carpets – into new threads for car mats, Adidas bikinis, environmentally friendly carpets and Prada bags.
For Bonazzi, shifting to recycled nylon was a question of survival for the family business. His parents founded a textile company in 1959 in a garage in Verona, Italy. Fifteen years later, they started Aquafil to produce nylon for making raincoats, an enterprise that led to factories on three continents. But before the turn of the century, cheap products from Asia flooded the market and destroyed Europe’s textile production. When Bonazzi had finished his business studies and prepared to take over the family company, he wondered how he could produce nylon, which is usually produced from petrochemicals, in a way that was both successful and ecologically sustainable.
The question led him on an intellectual journey as he read influential books by activists such as world-renowned marine biologist Sylvia Earle and got to know Michael Braungart, who helped develop the Cradle-to-Cradle ethos of a circular economy. But the challenges of applying these ideologies to his family business were steep. Although fishing nets have become a mainstay of environmental fashion ads—and giants like Dupont and BASF have made breakthroughs in recycling nylon—no one had been able to scale up these efforts.
For ten years, Bonazzi tinkered with ideas for a proprietary recycling process. “It’s incredibly difficult because these products are not made to be recycled,” Bonazzi says. One complication is the variety of materials used in older carpets. “They are made to be beautiful, to last, to be useful. We vastly underestimated the difficulty when we started.”
Soon it became clear to Bonazzi that he needed to change the entire production process. He found a way to disintegrate old fibers with heat and pull new strings from the discarded fishing nets and carpets. In 2022, his company Aquafil produced more than 45,000 tons of Econyl, which is 100% recycled nylon, from discarded waste.
More than half of Aquafil’s recyclate is from used goods. According to the company, the recycling saves 90 percent of the CO2 emissions compared to the production of conventional nylon. That amounts to saving 57,100 tons of CO2 equivalents for every 10,000 tons of Econyl produced.
Bonazzi collects fishing nets from all over the world, including Norway and Chile—which have the world’s largest salmon productions—in addition to the Mediterranean, Turkey, India, Japan, Thailand, the Philippines, Pakistan, and New Zealand. He counts the government leadership of Seychelles as his most recent client; the island has prohibited ships from throwing away their fishing nets, creating the demand for a reliable recycler. With nearly 3,000 employees, Aquafil operates almost 40 collection and production sites in a dozen countries, including four collection sites for old carpets in the U.S., located in California and Arizona.
First, the dirty nets are gathered, washed and dried. Bonazzi explains that nets often have been treated with antifouling agents such as copper oxide. “We recycle the coating separately,” he says via Zoom from his home near Verona. “Copper oxide is a useful substance, why throw it away?”
Still, only a small percentage of Aquafil’s products are made from nets fished out of the ocean, so your new bikini may not have saved a strangled baby dolphin. “Generally, nylon recycling is a good idea,” says Christian Schiller, the CEO of Cirplus, the largest global marketplace for recyclates and plastic waste. “But contrary to what consumers think, people rarely go out to the ocean to collect ghost nets. Most are old, discarded nets collected on land. There’s nothing wrong with this, but I find it a tad misleading to label the final products as made from ‘ocean plastic,’ prompting consumers to think they’re helping to clean the oceans by buying these products.”
Aquafil gets most of its nets from aqua farms. Surprisingly, one of Aquafil’s biggest problems is finding enough waste. “I know, it’s hard to believe because waste is everywhere,” Bonazzi says. “But we need to find it in reliable quantity and quality.” He has invested millions in establishing reliable logistics to source the fishing nets. Then the nets get shredded into granules that can be turned into car mats for the new Hyundai Ioniq 5 or a Gucci swimsuit.
The process works similarly with carpets. In the U.S. alone, 3.5 billion pounds of carpet are discarded in landfills every year, and less than 3 percent are currently recycled. Aquafil has built a recycling plant in Phoenix to help divert 12,500 tons of carpets from the landfill every year. The carpets are shredded and deconstructed into three components: fillers such as calcium carbonate will be reused in the cement industry, synthetic fibers like polypropylene can be used for engineering plastics, and nylon. Only the pelletized nylon gets shipped back to Europe for the production of Econyl. “We ship only what’s necessary,” Bonazzi says. Nearly 50 percent of his nylon in Italy and Slovenia is produced from recyclate, and he hopes to increase the percentage to two-thirds in the next two years.
His clients include Interface, the leading world pioneer for sustainable flooring, and many other carpet producers plus more than 2500 fashion labels, including Gucci, Prada, Patagonia, Louis Vuitton, Adidas and Stella McCartney. “Stella McCartney just introduced a parka that’s made 100 percent from Econyl,” Bonazzi says. “We’re also in a lot of sportswear because Nylon is a good fabric for swimwear and for yoga clothes.” Next, he’s looking into sunglasses and chairs made with Econyl - for instance, the flexible ergonomic noho chair, designed by New Zealand company Formway.
“When I look at a landfill, I see a gold mine," Bonazzi says.
“Bonazzi decided many years ago to invest in the production of recycled nylon though industry giants halted similar plans after losing large investments,” says Anika Herrmann, vice president of the German Greentech-competitor Camm Solutions, which creates bio-based polymers from cane sugar and other ag waste. “We need role models like Bonazzi who create sustainable solutions with courage and a pioneering spirit. Like Aquafil, we count on strategic partnerships to enable fast upscaling along the entire production chain.”
Bonazzi’s recycled nylon is still five to 10 percent more expensive than conventionally produced material. However, brands are increasingly bending to the pressure of eco-conscious consumers who demand sustainable fashion. What helped Bonazzi was the recent rise of oil prices and the pressure on industries to reduce their carbon footprint. Now Bonazzi says, “When I look at a landfill, I see a gold mine.”
Ideally, the manufacturers take the products back when the client is done with it, and because the nylon can theoretically be reused nearly infinitely, the chair or bikini could be made into another chair or bikini. “But honestly,” Bonazzi half-jokes, “if someone returns a McCartney parka to me, I’ll just resell it because it’s so expensive.”
The next step: Bonazzi wants to reshape the entire nylon industry by pivoting from post-consumer nylon to plant-based nylon. In 2017, he began producing “nylon-6,” together with Genomatica in San Diego. The process uses sugar instead of petroleum. “The idea is to make the very same molecule from sugar, not from oil,” he says. The demonstration plant in Ljubljana, Slovenia, has already produced several hundred tons of nylon, and Genomatica is collaborating with Lululemon to produce plant-based yoga wear.
Bonazzi acknowledges that his company needs a few more years before the technology is ready to meet his ultimate goal, producing only recyclable products with no petrochemicals, low emissions and zero waste on an industrial scale. “Recycling is not enough,” he says. “You also need to produce the primary material in a sustainable way, with a low carbon footprint.”
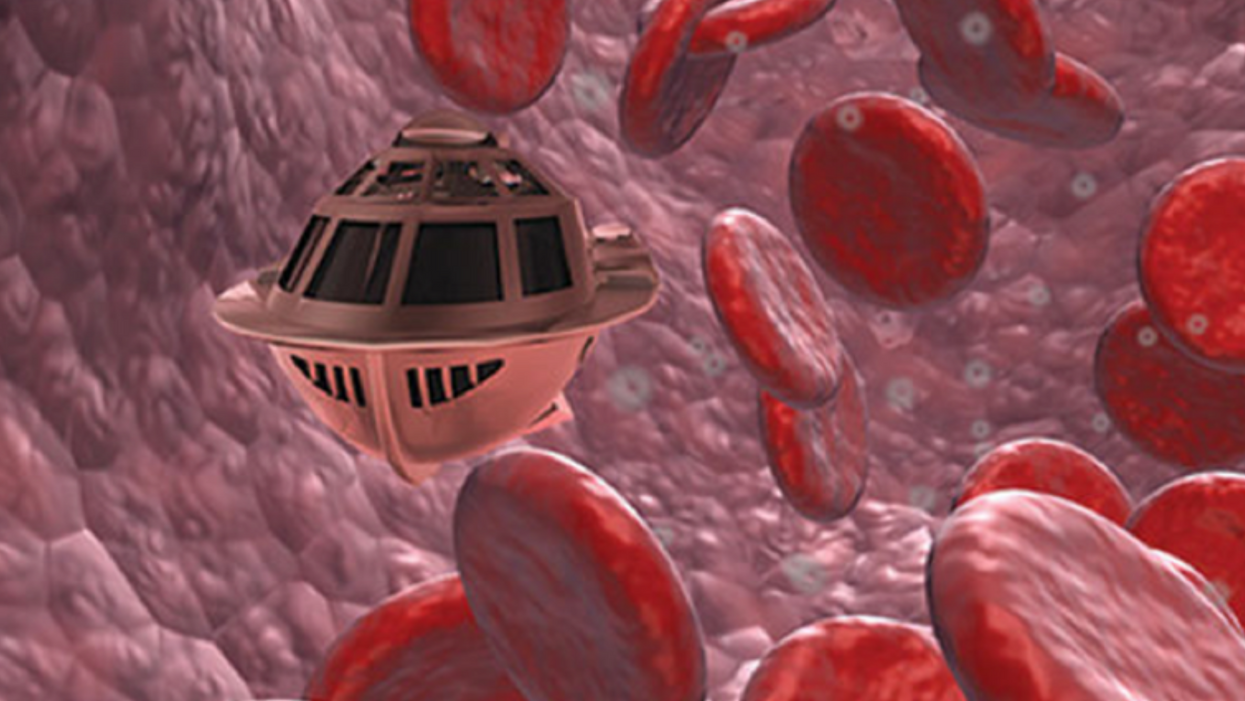
A movie still from the 1966 film "Fantastic Voyage"
In the 1966 movie "Fantastic Voyage," actress Raquel Welch and her submarine were shrunk to the size of a cell in order to eliminate a blood clot in a scientist's brain. Now, 55 years later, the scenario is becoming closer to reality.
California-based startup Bionaut Labs has developed a nanobot about the size of a grain of rice that's designed to transport medication to the exact location in the body where it's needed. If you think about it, the conventional way to deliver medicine makes little sense: A painkiller affects the entire body instead of just the arm that's hurting, and chemotherapy is flushed through all the veins instead of precisely targeting the tumor.
"Chemotherapy is delivered systemically," Bionaut-founder and CEO Michael Shpigelmacher says. "Often only a small percentage arrives at the location where it is actually needed."
But what if it was possible to send a tiny robot through the body to attack a tumor or deliver a drug at exactly the right location?
Several startups and academic institutes worldwide are working to develop such a solution but Bionaut Labs seems the furthest along in advancing its invention. "You can think of the Bionaut as a tiny screw that moves through the veins as if steered by an invisible screwdriver until it arrives at the tumor," Shpigelmacher explains. Via Zoom, he shares the screen of an X-ray machine in his Culver City lab to demonstrate how the half-transparent, yellowish device winds its way along the spine in the body. The nanobot contains a tiny but powerful magnet. The "invisible screwdriver" is an external magnetic field that rotates that magnet inside the device and gets it to move and change directions.
The current model has a diameter of less than a millimeter. Shpigelmacher's engineers could build the miniature vehicle even smaller but the current size has the advantage of being big enough to see with bare eyes. It can also deliver more medicine than a tinier version. In the Zoom demonstration, the micorobot is injected into the spine, not unlike an epidural, and pulled along the spine through an outside magnet until the Bionaut reaches the brainstem. Depending which organ it needs to reach, it could be inserted elsewhere, for instance through a catheter.
"The hope is that we can develop a vehicle to transport medication deep into the body," says Max Planck scientist Tian Qiu.
Imagine moving a screw through a steak with a magnet — that's essentially how the device works. But of course, the Bionaut is considerably different from an ordinary screw: "At the right location, we give a magnetic signal, and it unloads its medicine package," Shpigelmacher says.
To start, Bionaut Labs wants to use its device to treat Parkinson's disease and brain stem gliomas, a type of cancer that largely affects children and teenagers. About 300 to 400 young people a year are diagnosed with this type of tumor. Radiation and brain surgery risk damaging sensitive brain tissue, and chemotherapy often doesn't work. Most children with these tumors live less than 18 months. A nanobot delivering targeted chemotherapy could be a gamechanger. "These patients really don't have any other hope," Shpigelmacher says.
Of course, the main challenge of the developing such a device is guaranteeing that it's safe. Because tissue is so sensitive, any mistake could risk disastrous results. In recent years, Bionaut has tested its technology in dozens of healthy sheep and pigs with no major adverse effects. Sheep make a good stand-in for humans because their brains and spines are similar to ours.

The Bionaut device is about the size of a grain of rice.
Bionaut Labs
"As the Bionaut moves through brain tissue, it creates a transient track that heals within a few weeks," Shpigelmacher says. The company is hoping to be the first to test a nanobot in humans. In December 2022, it announced that a recent round of funding drew $43.2 million, for a total of 63.2 million, enabling more research and, if all goes smoothly, human clinical trials by early next year.
Once the technique has been perfected, further applications could include addressing other kinds of brain disorders that are considered incurable now, such as Alzheimer's or Huntington's disease. "Microrobots could serve as a bridgehead, opening the gateway to the brain and facilitating precise access of deep brain structure – either to deliver medication, take cell samples or stimulate specific brain regions," Shpigelmacher says.
Robot-assisted hybrid surgery with artificial intelligence is already used in state-of-the-art surgery centers, and many medical experts believe that nanorobotics will be the instrument of the future. In 2016, three scientists were awarded the Nobel Prize in Chemistry for their development of "the world's smallest machines," nano "elevators" and minuscule motors. Since then, the scientific experiments have progressed to the point where applicable devices are moving closer to actually being implemented.
Bionaut's technology was initially developed by a research team lead by Peer Fischer, head of the independent Micro Nano and Molecular Systems Lab at the Max Planck Institute for Intelligent Systems in Stuttgart, Germany. Fischer is considered a pioneer in the research of nano systems, which he began at Harvard University more than a decade ago. He and his team are advising Bionaut Labs and have licensed their technology to the company.
"The hope is that we can develop a vehicle to transport medication deep into the body," says Max Planck scientist Tian Qiu, who leads the cooperation with Bionaut Labs. He agrees with Shpigelmacher that the Bionaut's size is perfect for transporting medication loads and is researching potential applications for even smaller nanorobots, especially in the eye, where the tissue is extremely sensitive. "Nanorobots can sneak through very fine tissue without causing damage."
In "Fantastic Voyage," Raquel Welch's adventures inside the body of a dissident scientist let her swim through his veins into his brain, but her shrunken miniature submarine is attacked by antibodies; she has to flee through the nerves into the scientist's eye where she escapes into freedom on a tear drop. In reality, the exit in the lab is much more mundane. The Bionaut simply leaves the body through the same port where it entered. But apart from the dramatization, the "Fantastic Voyage" was almost prophetic, or, as Shpigelmacher says, "Science fiction becomes science reality."
This article was first published by Leaps.org on April 12, 2021.
These doctors have a heart for recycling
In the U.S. and Europe, it is illegal to reuse pacemakers and other implants. Therefore, cardiologists export them to the global South where they save the lives of people of all ages.
This is part 3 of a three part series on a new generation of doctors leading the charge to make the health care industry more sustainable - for the benefit of their patients and the planet. Read part 1 here and part 2 here.
One could say that over 400 people owe their life to the fact that Carsten Israel fell in love. Twenty years ago, as a young doctor in Frankfurt, Germany, he began to court an au pair from Kenya, Elisabeth, his now-wife of 13 years with whom he has three children. When the couple started visiting her parents in Kenya, Israel wanted to check out the local hospitals, “just out of professional curiosity,“ says the cardiologist, who is currently the head doctor at the Clinic for Interior Medicine in Bielefeld. “I was completely shocked.“
Often he observed there were no doctors in the E.R.s, and hte nurses could render only basic first aid. “When somebody fell into a coma, they fell into a coma,“ Israel remembers. “There weren’t even any defibrillators to restart a patient’s heart,” while defibrillators are standard equipment in most clinics in the U.S. and Europe as lifesaving devices. When Israel finally visited the largest and most modern hospital in Nairobi, he found it better equipped but he learned that its services were only available to patients who could afford them. The cardiologist there had a drawer full of petitions from patients with heart ailments who couldn’t afford lifesaving surgery. Even two decades ago, a pacemaker cost $5,000 in Kenya, which made it unaffordable for most Kenyans who earn an average of $600 per month.
Since 2003, Israel and a team of two doctors and two nurses visit Kenya and Zambia once or twice a year to implant German pacemakers for free. Notably, the pacemakers and defibrillators Israel exports to Africa would end up in the landfill in Germany. Clinics have to pay for specialized services to dispose of this medical equipment. “In Germany, I could go to jail if I used a defibrillator that is one day past its expiration date,“ Israel says, “but in Kenya, people don’t have the money for the cheapest model. What nonsense to throw this precious medical equipment away while people in poorer countries die because they desperately need it.“
Israel works at the breakpoint between the laws in a wealthy country like Germany and the reality in the global South. The U.S. and most European countries have strict laws that ban the reuse of medical implants and enforce strict expiration dates for medical equipment. “But if a pacemaker is a few days past its expiration date, it still works perfectly fine,“ Israel says. “And it also happens that we implant a pacemaker and five months later it turns out that the patient needs a different kind. Then we replace it and we’d have to trash the first one in Germany, though it could easily run another 12 years.“
“If we get this right, we have lots of devices we can implant, hips and knees, etcetera. Where this will lead is limitless," says Eva Kline Rogers, the program coordinator for My Heart, Your Heart.
Israel has been collecting donations of pacemakers and defibrillators from manufacturers but also from other doctors and from funeral homes for his nonprofit Pacemakers for East Africa since 2003. Most funeral homes in the U.S. and Europe are legally obliged to remove pacemakers from the dead before cremation. “Most pacemakers survive their owners,“ says Israel. He sterilizes the pacemakers and finds them a new life in East Africa. Studies show that reused pacemakers carry no greater risk for the patients than new ones.
In the U.S., University of Michigan professor Thomas Crawford heads up a similar initiative, My Heart, Your Heart. “Each year 1 to 2 million individuals worldwide die due to a lack of access to pacemakers and defibrillators,” the organization notes on its website. The nonprofit was founded in 2009, but it took four years for the doctors to get permission from the FDA to export pacemakers. Since receiving permission, the organization has sent dozens of devices to the Philippines, Haiti, Venezuela, Kenya, Sierra Leone and Ukraine. “We were the first doctors ever to implant a pacemaker in Sierra Leone in 2018,” says Crawford, who has traveled extensively to most of the recipient countries.
Even individuals can donate their pacemakers; the organization offers a prepaid envelope. “My mother recently passed and she donated her device,” says Tina Alexandris-Souphis, one of the doctors at University of Michigan who collaborates on My Heart, Your Heart. The organization works with World Medical Relief and the U.K. based charity Pace4Life to maintain a registry of the most urgent patients and send devices to where they are needed the most.
My Heart, Your Heart is also conducting a randomized controlled trial to provide further evidence that reused pacemakers pose no additional risk. “Our vision is that we establish this is safe and create a blueprint for organizations around the world to safely reuse these devices instead of them being thrown in the trash,” says Eva Kline Rogers, the program’s coordinator. “If we get this right, we have lots of devices we can implant, hips and knees, etc. Where this will lead is limitless.” She points out that in addition to receiving the donated devices, the doctors in the global South also benefit from the expertise of renowned cardiologists, such as Crawford, who sometimes advise them in complex cases.
And Adrian Baranchuk, a Canadian doctor at the Kingston General Hospital at the Queen’s University, regularly travels through South America with his “cardiology van” to help villagers in remote areas with heart problems.
Israel says that he’s been accused of racism, in thinking that these pacemakers are suitable for those in the global South - many of whom are people of color - even though officials in wealthier countries consider them to be trash. The cardiologist counters such criticism with stories about desperate need of his patients. At his first medical visit to Nairobi that he organized with a local cardiologist, six patients were waiting for him. “In Germany, they would all be considered emergencies,” Israel says. One eighty-year old grandmother had a heartrate of 18. “I’ve never before seen anything like this,” Israel exclaims. “At first I thought I couldn’t find her pulse before I realized that her heart was only beating once every three seconds.” After the surgery, she got up, dressed herself and hurriedly packed her bag, explaining she had a ton of work to accomplish. Her family was in disbelief, Israel says. “They told me she had been bedridden for five years because as soon as she tried to get up she would faint.”

Israel has been accused of racism, in thinking that these pacemakers are suitable for those in the global South even though they're considered to be trash by officials in wealthier countries. The cardiologist counters such criticism with stories about desperate need of his patients.
Carsten Israel
The hospital in Nairobi where Israel conducts the surgeries, charges patients $200 for the use of its facilities. If patients can’t afford that sum, Israel will pay it from the funds of his nonprofit. For some people, $200 far exceeds their resources. Once, a family from the extremely poor Northern region of Kenya told him they couldn’t afford the $3 for the bus ride to Nairobi. Israel suspected this was a pretense because they were afraid of the surgery and agreed to reimburse the $3, “but when they came, they were wearing rags and were so rail-thin, I understood that they really needed every cent they had for food.”
Israel is a renowned cardiologists in Germany. And yet, he considers his work in East Africa to be particularly meaningful. “Generally, most patients in Germany will get the treatment they need,” he says, “and I never before experienced that people have an illness that is easily curable but simply won’t be treated.” He also feels a heavy responsibility. Many patients have his personal cell phone and call him when they have problems or good news about how they’re doing.
Some of those progress reports come much faster than in Israel’s home country. Before he implanted a pacemaker in a tall Massai in Kenya, the man had been picked on by his family because he wouldn’t help much with the hard work on the family peanut farm. “When I examined him, he had a pulse of 40,” Israel says. “It’s a miracle he was even standing upright, let alone hauling heavy bags.” After the surgery, Israel advised his patient to stay the night for observation, but the patient couldn’t wait to leave. Two hours later, he returned, covered in sweat. He’d been running sprints with his brothers to test the new device. Israel shakes his head. In Germany, it would be unthinkable for a patient to engage in athletics immediately after surgery. But the patient was exuberant: “I was the fastest!”
The success stories are notable partly because the challenges remain so steep. In Zambia, for instance, there is a single cardiologist; she determined to become one after losing her younger sister to an easily curable heart disease. Often, the hospitals not only lack pacemakers but also sterile surgery equipment, antibiotics and other essential material. Therefore, Israel and his team import everything they need for the surgeries, including medication. If necessary, they improvise. “I’ve done surgery with a desk lamp hanging from the ceiling by threads,” Israel says. He already knows that he will need to return to Kenya in six months to replace the pacemaker of one of his patients and replace the batteries in others. If he doesn’t travel, lives are at risk.