Bivalent Boosters for Young Children Are Elusive. The Search Is On for Ways to Improve Access.

Theo, an 18-month-old in rural Nebraska, walks with his father in their backyard. For many toddlers, the barriers to accessing COVID-19 vaccines are many, such as few locations giving vaccines to very young children.
It’s Theo’s* first time in the snow. Wide-eyed, he totters outside holding his father’s hand. Sarah Holmes feels great joy in watching her 18-month-old son experience the world, “His genuine wonder and excitement gives me so much hope.”
In the summer of 2021, two months after Theo was born, Holmes, a behavioral health provider in Nebraska lost her grandparents to COVID-19. Both were vaccinated and thought they could unmask without any risk. “My grandfather was a veteran, and really trusted the government and faith leaders saying that COVID-19 wasn’t a threat anymore,” she says.” The state of emergency in Louisiana had ended and that was the message from the people they respected. “That is what killed them.”
The current official public health messaging is that regardless of what variant is circulating, the best way to be protected is to get vaccinated. These warnings no longer mention masking, or any of the other Swiss-cheese layers of mitigation that were prevalent in the early days of this ongoing pandemic.
The problem with the prevailing, vaccine centered strategy is that if you are a parent with children under five, barriers to access are real. In many cases, meaningful tools and changes that would address these obstacles are lacking, such as offering vaccines at more locations, mandating masks at these sites, and providing paid leave time to get the shots.
Children are at risk
Data presented at the most recent FDA advisory panel on COVID-19 vaccines showed that in the last year infants under six months had the third highest rate of hospitalization. “From the beginning, the message has been that kids don’t get COVID, and then the message was, well kids get COVID, but it’s not serious,” says Elias Kass, a pediatrician in Seattle. “Then they waited so long on the initial vaccines that by the time kids could get vaccinated, the majority of them had been infected.”
A closer look at the data from the CDC also reveals that from January 2022 to January 2023 children aged 6 to 23 months were more likely to be hospitalized than all other vaccine eligible pediatric age groups.
“We sort of forced an entire generation of kids to be infected with a novel virus and just don't give a shit, like nobody cares about kids,” Kass says. In some cases, COVID has wreaked havoc with the immune systems of very young children at his practice, making them vulnerable to other illnesses, he said. “And now we have kids that have had COVID two or three times, and we don’t know what is going to happen to them.”
Jumping through hurdles
Children under five were the last group to have an emergency use authorization (EUA) granted for the COVID-19 vaccine, a year and a half after adult vaccine approval. In June 2022, 30,000 sites were initially available for children across the country. Six months later, when boosters became available, there were only 5,000.
Currently, only 3.8% of children under two have completed a primary series, according to the CDC. An even more abysmal 0.2% under two have gotten a booster.
Ariadne Labs, a health center affiliated with Harvard, is trying to understand why these gaps exist. In conjunction with Boston Children’s Hospital, they have created a vaccine equity planner that maps the locations of vaccine deserts based on factors such as social vulnerability indexes and transportation access.
“People are having to travel farther because the sites are just few and far between,” says Benjy Renton, a research assistant at Ariadne.
Michelle Baltes-Breitwisch, a pharmacist, and her two-year-old daughter, Charlee, live in Iowa. When the boosters first came out she expected her toddler could get it close to home, but her husband had to drive Charlee four hours roundtrip.
This experience hasn’t been uncommon, especially in rural parts of the U.S. If parents wanted vaccines for their young children shortly after approval, they faced the prospect of loading babies and toddlers, famous for their calm demeanor, into cars for lengthy rides. The situation continues today. Mrs. Smith*, a grant writer and non-profit advisor who lives in Idaho, is still unable to get her child the bivalent booster because a two-hour one-way drive in winter weather isn’t possible.
It can be more difficult for low wage earners to take time off, which poses challenges especially in a number of rural counties across the country, where weekend hours for getting the shots may be limited.
Protect Their Future (PTF), a grassroots organization focusing on advocacy for the health care of children, hears from parents several times a week who are having trouble finding vaccines. The vaccine rollout “has been a total mess,” says Tamara Lea Spira, co-founder of PTF “It’s been very hard for people to access vaccines for children, particularly those under three.”
Seventeen states have passed laws that give pharmacists authority to vaccinate as young as six months. Under federal law, the minimum age in other states is three. Even in the states that allow vaccination of toddlers, each pharmacy chain varies. Some require prescriptions.
It takes time to make phone calls to confirm availability and book appointments online. “So it means that the parents who are getting their children vaccinated are those who are even more motivated and with the time and the resources to understand whether and how their kids can get vaccinated,” says Tiffany Green, an associate professor in population health sciences at the University of Wisconsin at Madison.
Green adds, “And then we have the contraction of vaccine availability in terms of sites…who is most likely to be affected? It's the usual suspects, children of color, disabled children, low-income children.”
It can be more difficult for low wage earners to take time off, which poses challenges especially in a number of rural counties across the country, where weekend hours for getting the shots may be limited. In Bibb County, Ala., vaccinations take place only on Wednesdays from 1:45 to 3:00 pm.
“People who are focused on putting food on the table or stressed about having enough money to pay rent aren't going to prioritize getting vaccinated that day,” says Julia Raifman, assistant professor of health law, policy and management at Boston University. She created the COVID-19 U.S. State Policy Database, which tracks state health and economic policies related to the pandemic.
Most states in the U.S. lack paid sick leave policies, and the average paid sick days with private employers is about one week. Green says, “I think COVID should have been a wake-up call that this is necessary.”
Maskless waiting rooms
For her son, Holmes spent hours making phone calls but could uncover no clear answers. No one could estimate an arrival date for the booster. “It disappoints me greatly that the process for locating COVID-19 vaccinations for young children requires so much legwork in terms of time and resources,” she says.
In January, she found a pharmacy 30 minutes away that could vaccinate Theo. With her son being too young to mask, she waited in the car with him as long as possible to avoid a busy, maskless waiting room.
Kids under two, such as Theo, are advised not to wear masks, which make it too hard for them to breathe. With masking policies a rarity these days, waiting rooms for vaccines present another barrier to access. Even in healthcare settings, current CDC guidance only requires masking during high transmission or when treating COVID positive patients directly.
“This is a group that is really left behind,” says Raifman. “They cannot wear masks themselves. They really depend on others around them wearing masks. There's not even one train car they can go on if their parents need to take public transportation… and not risk COVID transmission.”
Yet another challenge is presented for those who don’t speak English or Spanish. According to Translators without Borders, 65 million people in America speak a language other than English. Most state departments of health have a COVID-19 web page that redirects to the federal vaccines.gov in English, with an option to translate to Spanish only.
The main avenue for accessing information on vaccines relies on an internet connection, but 22 percent of rural Americans lack broadband access. “People who lack digital access, or don’t speak English…or know how to navigate or work with computers are unable to use that service and then don’t have access to the vaccines because they just don’t know how to get to them,” Jirmanus, an affiliate of the FXB Center for Health and Human Rights at Harvard and a member of The People’s CDC explains. She sees this issue frequently when working with immigrant communities in Massachusetts. “You really have to meet people where they’re at, and that means physically where they’re at.”
Equitable solutions
Grassroots and advocacy organizations like PTF have been filling a lot of the holes left by spotty federal policy. “In many ways this collective care has been as important as our gains to access the vaccine itself,” says Spira, the PTF co-founder.
PTF facilitates peer-to-peer networks of parents that offer support to each other. At least one parent in the group has crowdsourced information on locations that are providing vaccines for the very young and created a spreadsheet displaying vaccine locations. “It is incredible to me still that this vacuum of information and support exists, and it took a totally grassroots and volunteer effort of parents and physicians to try and respond to this need.” says Spira.
Kass, who is also affiliated with PTF, has been vaccinating any child who comes to his independent practice, regardless of whether they’re one of his patients or have insurance. “I think putting everything on retail pharmacies is not appropriate. By the time the kids' vaccines were released, all of our mass vaccination sites had been taken down.” A big way to help parents and pediatricians would be to allow mixing and matching. Any child who has had the full Pfizer series has had to forgo a bivalent booster.
“I think getting those first two or three doses into kids should still be a priority, and I don’t want to lose sight of all that,” states Renton, the researcher at Ariadne Labs. Through the vaccine equity planner, he has been trying to see if there are places where mobile clinics can go to improve access. Renton continues to work with local and state planners to aid in vaccine planning. “I think any way we can make that process a lot easier…will go a long way into building vaccine confidence and getting people vaccinated,” Renton says.

Michelle Baltes-Breitwisch, a pharmacist, and her two-year-old daughter, Charlee, live in Iowa. Her husband had to drive four hours roundtrip to get the boosters for Charlee.
Michelle Baltes-Breitwisch
Other changes need to come from the CDC. Even though the CDC “has this historic reputation and a mission of valuing equity and promoting health,” Jirmanus says, “they’re really failing. The emphasis on personal responsibility is leaving a lot of people behind.” She believes another avenue for more equitable access is creating legislation for upgraded ventilation in indoor public spaces.
Given the gaps in state policies, federal leadership matters, Raifman says. With the FDA leaning toward a yearly COVID vaccine, an equity lens from the CDC will be even more critical. “We can have data driven approaches to using evidence based policies like mask policies, when and where they're most important,” she says. Raifman wants to see a sustainable system of vaccine delivery across the country complemented with a surge preparedness plan.
With the public health emergency ending and vaccines going to the private market sometime in 2023, it seems unlikely that vaccine access is going to improve. Now more than ever, ”We need to be able to extend to people the choice of not being infected with COVID,” Jirmanus says.
*Some names were changed for privacy reasons.
New Options Are Emerging in the Search for Better Birth Control
Photo by JPC-PROD on Adobe Stock
About decade ago, Elizabeth Summers' options for birth control suddenly narrowed. Doctors diagnosed her with Factor V Leiden, a rare genetic disorder, after discovering blood clots in her lungs. The condition increases the risk of clotting, so physicians told Summers to stay away from the pill and other hormone-laden contraceptives. "Modern medicine has generally failed to provide me with an effective and convenient option," she says.
But new birth control options are emerging for women like Summers. These alternatives promise to provide more choices to women who can't ingest hormones or don't want to suffer their unpleasant side effects.
These new products have their own pros and cons. Still, doctors are welcoming new contraceptives following a long drought in innovation. "It's been a long time since we've had something new in the world of contraception," says Heather Irobunda, an obstetrician and gynecologist at NYC Health and Hospitals.
On social media, Irobunda often fields questions about one of these new options, a lubricating gel called Phexxi. San Diego-based Evofem, the company behind Phexxi, has been advertising the product on Hulu and Instagram after the gel was approved by the Food and Drug Administration in May 2020. The company's trendy ads target women who feel like condoms diminish the mood, but who also don't want to mess with an IUD or hormones.
Here's how it works: Phexxi is inserted via a tampon-like device up to an hour before sex. The gel regulates vaginal pH — essentially, the acidity levels — in a range that's inhospitable to sperm. It sounds a lot like spermicide, which is also placed in the vagina prior to sex to prevent pregnancy. But spermicide can damage the vagina's cell walls, which can increase the risk of contracting sexually transmitted diseases.
"Not only is innovation needed, but women want a non-hormonal option."
Phexxi isn't without side effects either. The most common one is vaginal burning, according to a late-stage trial. It's also possible to develop a urinary tract infection while using the product. That same study found that during typical use, Phexxi is about 86 percent effective at preventing pregnancy. The efficacy rate is comparable to condoms but lower than birth control pills (91 percent) and significantly lower than an IUD (99 percent).
Phexxi – which comes in a pack of 12 – represents a tiny but growing part of the birth control market. Pharmacies dispensed more than 14,800 packs from April through June this year, a 65 percent increase over the previous quarter, according to data from Evofem.
"We've been able to demonstrate that not only is innovation needed, but women want a non-hormonal option," says Saundra Pelletier, Evofem's CEO.
Beyond contraception, the company is carrying out late-stage tests to gauge Phexxi's effectiveness at preventing the sexually transmitted infections chlamydia and gonorrhea.

Phexxi is inserted via a tampon-like device up to an hour before sex.
Phexxi
A New Pill
The first birth control pill arrived in 1960, combining the hormones estrogen and progestin to stop sperm from joining with an egg, giving women control over their fertility. Subsequent formulations sought to ease side effects, by way of lower amounts of estrogen. But some women still experience headaches and nausea – or more serious complications like blood clots. On social media, women noted that birth control pills are much more likely to cause blood clots than Johnson & Johnson's COVID-19 vaccine that was briefly paused to evaluate the risk of clots in women under age 50. What will it take, they wondered, for safer birth control?
Mithra Pharmaceuticals of Belgium sought to create a gentler pill. In April 2021, the FDA approved Mithra's Nextstellis, which includes a naturally occurring estrogen, the first new estrogen in the U.S. in 50 years. Nextstellis selectively acts on tissues lining the uterus, while other birth control pills have a broader target.
A Phase 3 trial showed a 98 percent efficacy rate. Andrew London, an obstetrician and gynecologist, who practices at several Maryland hospitals, says the results are in line with some other birth control pills. But, he added, early studies indicate that Nextstellis has a lower risk of blood clotting, along with other potential benefits, which additional clinical testing must confirm.
"It's not going to be worse than any other pill. We're hoping it's going to be significantly better," says London.
The estrogen in Nexstellis, called estetrol, was skipped over by the pharmaceutical industry after its discovery in the 1960s. Estetrol circulates between the mother and fetus during pregnancy. Decades later, researchers took a new look, after figuring out how to synthesize estetrol in a lab, as well as produce estetrol from plants.
"That allowed us to really start to investigate the properties and do all this stuff you have to do for any new drug," says Michele Gordon, vice president of marketing in women's health at Mayne Pharma, which licensed Nextstellis.
Bonnie Douglas, who followed the development of Nextstellis as part of a search for better birth control, recently switched to the product. "So far, it's much more tolerable," says Douglas. Previously, the Midwesterner was so desperate to find a contraceptive with fewer side effects that she turned to an online pharmacy to obtain a different birth control pill that had been approved in Canada but not in the U.S.
Contraceptive Access
Even if a contraceptive lands FDA approval, access poses a barrier. Getting insurers to cover new contraceptives can be difficult. For the uninsured, state and federal programs can help, and companies should keep prices in a reasonable range, while offering assistance programs. So says Kelly Blanchard, president of the nonprofit Ibis Reproductive Health. "For innovation to have impact, you want to reach as many folks as possible," she says.
In addition, companies developing new contraceptives have struggled to attract venture capital. That's changing, though.
In 2015, Sabrina Johnson founded DARÉ Bioscience around the idea of women's health. She estimated the company would be fully funded in six months, based on her track record in biotech and the demand for novel products.
But it's been difficult to get male investors interested in backing new contraceptives. It took Johnson two and a half years to raise the needed funds, via a reverse merger that took the company public. "There was so much education that was necessary," Johnson says, adding: "The landscape has changed considerably."
Johnson says she would like to think DARÉ had something to do with the shift, along with companies like Organon, a spinout of pharma company Merck that's focused on reproductive health. In surveying the fertility landscape, DARÉ saw limited non-hormonal options. On-demand options – like condoms – can detract from the moment. Copper IUDs must be inserted by a doctor and removed if a woman wants to return to fertility, and this method can have onerous side effects.
So, DARÉ created Ovaprene, a hormone-free device that's designed to be inserted into the vagina monthly by the user. The mesh product acts as a barrier, while releasing a chemical that immobilizes sperm. In an early study, the company reported that Ovaprene prevented almost all sperm from entering the cervical canal. The results, DARÉ believes, indicate high efficacy. Should Ovaprene eventually win regulatory approval, drug giant Bayer will handle commercializing the device.
Other new forms of birth control in development are further out, and that's assuming they perform well in clinical trials. Among them: a once-a-month birth control pill, along with a male version of the birth control pill. The latter is often brought up among women who say it's high time that men take a more proactive role in birth control.
For Summers, her search for a safe and convenient birth control continues. She tried Phexxi, which caused irritation. Still, she's excited that a non-hormonal option now exists. "I'm sure it will work for others," she says.
This article was first published by Leaps.org on August 31, 2021.
Hyperbaric oxygen therapy could treat Long COVID, new study shows
Hyperbaric oxygen therapy has been used in the past to help people with traumatic brain injury, stroke and other conditions involving wounds to the brain. Now, researchers at Shamir Medical Center in Tel Aviv are studying how it could treat Long Covid.
Long COVID is not a single disease, it is a syndrome or cluster of symptoms that can arise from exposure to SARS-CoV-2, a virus that affects an unusually large number of different tissue types. That's because the ACE2 receptor it uses to enter cells is common throughout the body, and inflammation from the immune response fighting that infection can damage surrounding tissue.
One of the most widely shared groups of symptoms is fatigue and what has come to be called “brain fog,” a difficulty focusing and an amorphous feeling of slowed mental functioning and capacity. Researchers have tied these COVID-related symptoms to tissue damage in specific sections of the brain and actual shrinkage in its size.
When Shai Efrati, medical director of the Sagol Center for Hyperbaric Medicine and Research in Tel Aviv, first looked at functional magnetic resonance images (fMRIs) of patients with what is now called long COVID, he saw “micro infarcts along the brain.” It reminded him of similar lesions in other conditions he had treated with hyperbaric oxygen therapy (HBOT). “Once we saw that, we said, this is the type of wound we can treat. It doesn't matter if the primary cause is mechanical injury like TBI [traumatic brain injury] or stroke … we know how to oxidize them.”Efrati came to HBOT almost by accident. The physician had seen how it had helped heal diabetic ulcers and improved the lives of other patients, but he was busy with his own research. Then the director of his Tel Aviv hospital threatened to shut down the small HBOT chamber unless Efrati took on administrative responsibility for it. He reluctantly agreed, a decision that shifted the entire focus of his research.
“The main difference between wounds in the leg and wounds in the brain is that one is something we can see, it's tangible, and the wound in the brain is hidden,” says Efrati. With fMRIs, he can measure how a limited supply of oxygen in blood is shuttled around to fuel activity in various parts of the brain. Years of research have mapped how specific areas of the brain control activity ranging from thinking to moving. An fMRI captures the brain area as it’s activated by supplies of oxygen; lack of activity after the same stimuli suggests damage has occurred in that tissue. Suddenly, what was hidden became visible to researchers using fMRI. It helped to make a diagnosis and measure response to treatment.
HBOT is not a single thing but rather a tool, a process or approach with variations depending on the condition being treated. It aims to increase the amount of oxygen that gets to damaged tissue and speed up healing. Regular air is about 21 percent oxygen. But inside the HBOT chamber the atmospheric pressure can be increased to up to three times normal pressure at sea level and the patient breathes pure oxygen through a mask; blood becomes saturated with much higher levels of oxygen. This can defuse through the damaged capillaries of a wound and promote healing.
The trial
Efrati’s clinical trials started in December 2020, barely a year after SARS-CoV-2 had first appeared in Israel. Patients who’d experienced cognitive issues after having COVID received 40 sessions in the chamber over a period of 60 days. In each session, they spent 90 minutes breathing through a mask at two atmospheres of pressure. While inside, they performed mental exercises to train the brain. The only difference between the two groups of patients was that one breathed pure oxygen while the other group breathed normal air. No one knew who was receiving which level of oxygen.
The results were striking. Before and after fMRIs showed significant repair of damaged tissue in the brain and functional cognition tests improved substantially among those who received pure oxygen. Importantly, 80 percent of patients said they felt back to “normal,” but Efrati says they didn't include patient evaluation in the paper because there was no baseline data to show how they functioned before COVID. After the study was completed, the placebo group was offered a new round of treatments using 100 percent oxygen, and the team saw similar results.
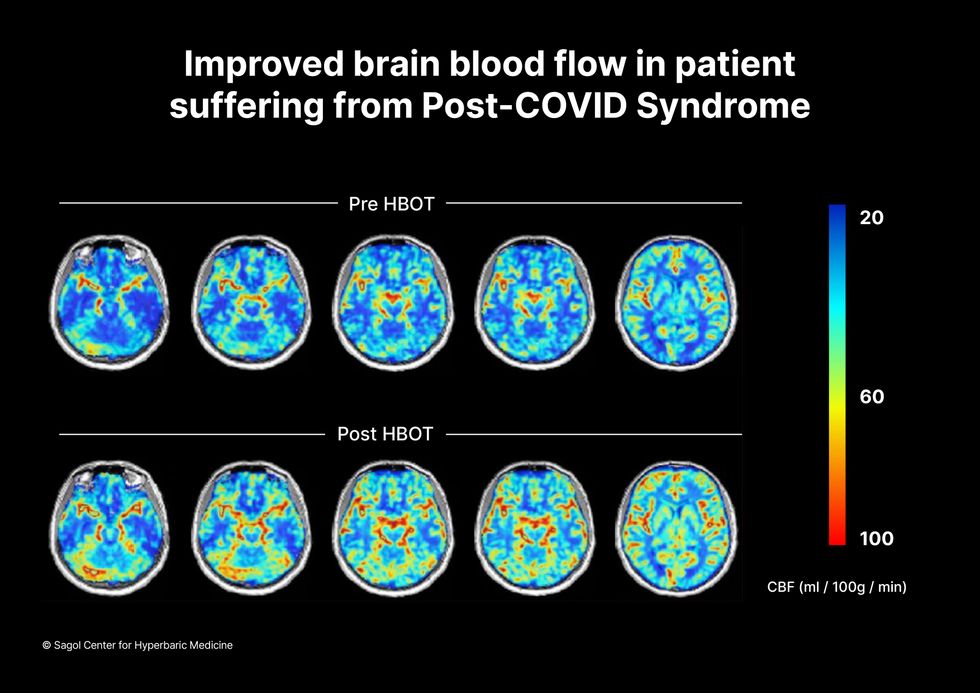
Scans show improved blood flow in a patient suffering from Long Covid.
Sagol Center for Hyperbaric Medicine
Efrati's use of HBOT is part of an emerging geroscience approach to diseases associated with aging. These researchers see systems dysfunctions that are common to several diseases, such as inflammation, which has been shown to play a role in micro infarcts, heart disease and Alzheimer’s disease. Preliminary research suggests that HBOT can retard some underlying mechanisms of aging, which might address several medical conditions. However, the drug approval process is set up to regulate individual disease, not conditions as broad as aging, and so they concentrate on treating the low hanging fruit: disorders where effective treatments currently are limited and success might be demonstrated.
The key to HBOT's effectiveness is something called the hyperoxic-hypoxic paradox where a body does not react to an increase in available oxygen, only to a decrease, regardless of the starting point. That danger signal has a powerful effect on gene expression, resulting in changes in metabolism, and the proliferation of stem cells. That occurs with each cycle of 20 minutes of pure oxygen followed by 5 minutes of regular air circulating through the masks, while the chamber remains pressurized. The high levels of oxygen in the blood provide the fuel necessary for tissue regeneration.
The hyperbaric chamber that Efrati has built can hold a dozen patients and attending medical staff. Think of it as a pressurized airplane cabin, only with much more space than even in first class. In the U.S., people think of HBOT as “a sack of air or some tube that you can buy on Amazon” or find at a health spa. “That is total bullshit,” Efrati says. “It has to be a medical class center where a physician can lose their license if they are not operating it properly.”

Shai Efrati
Alexander Charney, a research psychiatrist at the Icahn School of Medicine at Mount Sinai in New York City, calls Efrati’s study thoughtful and well designed. But it demands a lot from patients with its intense number of sessions. Those types of regimens have proven difficult to roll out to large numbers of patients. Still, the results are intriguing enough to merit additional trials.
John J. Miller, a physician and editor in chief of Psychiatric Times, has seen “many physicians that use hyperbaric oxygen for various brain disorders such as TBI.” He is intrigued by Efrati's work and believes the approach “has great potential to help patients with long COVID whose symptoms are related to brain tissue changes.”
Efrati believes so much in the power of the hyperoxic-hypoxic paradox to heal a variety of tissue injuries that he is leading the medical advisory board at Aviv Clinic, an international network of clinics that are delivering HBOT treatments based on research conducted in Israel. His goal is to silence doubters by quickly opening about 50 such clinics worldwide, based on the model of standalone dialysis clinics in the United States. Sagol Center is treating 300 patients per day, and clinics have opened in Florida and Dubai. There are plans to open another in Manhattan.

