Blood Money: Paying for Convalescent Plasma to Treat COVID-19
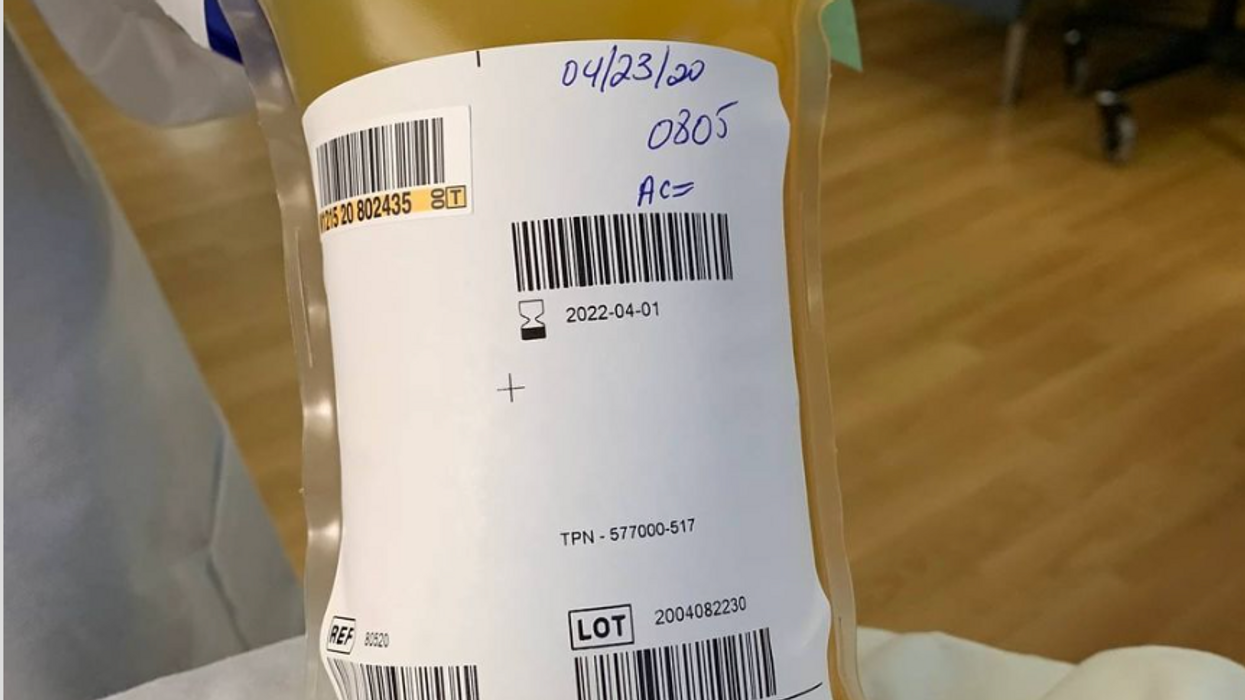
A bag of plasma that Tom Hanks donated back in April 2020 after his coronavirus infection. (He was not paid to donate.)
Convalescent plasma – first used to treat diphtheria in 1890 – has been dusted off the shelf to treat COVID-19. Does it work? Should we rely strictly on the altruism of donors or should people be paid for it?
The biologic theory is that a person who has recovered from a disease has chemicals in their blood, most likely antibodies, that contributed to their recovery, and transferring those to a person who is sick might aid their recovery. Whole blood won't work because there are too few antibodies in a single unit of blood and the body can hold only so much of it.
Plasma comprises about 55 percent of whole blood and is what's left once you take out the red blood cells that carry oxygen and the white blood cells of the immune system. Most of it is water but the rest is a complex mix of fats, salts, signaling molecules and proteins produced by the immune system, including antibodies.
A process called apheresis circulates the donors' blood through a machine that separates out the desired parts of blood and returns the rest to the donor. It takes several times the length of a regular whole blood donation to cycle through enough blood for the process. The end product is a yellowish concentration called convalescent plasma.
Recent History
It was used extensively during the great influenza epidemic off 1918 but fell out of favor with the development of antibiotics. Still, whenever a new disease emerges – SARS, MERS, Ebola, even antibiotic-resistant bacteria – doctors turn to convalescent plasma, often as a stopgap until more effective antibiotic and antiviral drugs are developed. The process is certainly safe when standard procedures for handling blood products are followed, and historically it does seem to be beneficial in at least some patients if administered early enough in the disease.
With few good treatment options for COVID-19, doctors have given convalescent plasma to more than a hundred thousand Americans and tens of thousand of people elsewhere, to mixed results. Placebo-controlled trials could give a clearer picture of plasma's value but it is difficult to enroll patients facing possible death when the flip of a coin will determine who will receive a saline solution or plasma.
And the plasma itself isn't some uniform pill stamped out in a factory, it's a natural product that is shaped by the immune history of the donor's body and its encounter not just with SARS-CoV-2 but a lifetime of exposure to different pathogens.
Researchers believe antibodies in plasma are a key factor in directly fighting the virus. But the variety and quantity of antibodies vary from donor to donor, and even over time from the same donor because once the immune system has cleared the virus from the body, it stops putting out antibodies to fight the virus. Often the quality and quantity of antibodies being given to a patient are not measured, making it somewhat hit or miss, which is why several companies have recently developed monoclonal antibodies, a single type of antibody found in blood that is effective against SARS-CoV-2 and that is multiplied in the lab for use as therapy.
Plasma may also contain other unknown factors that contribute to fighting disease, say perhaps signaling molecules that affect gene expression, which might affect the movement of immune cells, their production of antiviral molecules, or the regulation of inflammation. The complexity and lack of standardization makes it difficult to evaluate what might be working or not with a convalescent plasma treatment. Thus researchers are left with few clues about how to make it more effective.
Industrializing Plasma
Many Americans living along the border with Mexico regularly head south to purchase prescription drugs at a significant discount. Less known is the medical traffic the other way, Mexicans who regularly head north to be paid for plasma donations, which are prohibited in their country; the U.S. allows payment for plasma donations but not whole blood. A typical payment is about $35 for a donation but the sudden demand for convalescent plasma from people who have recovered from COVID-19 commands a premium price, sometimes as high as $200. These donors are part of a fast-growing plasma industry that surpassed $25 billion in 2018. The U.S. supplies about three-quarters of the world's needs for plasma.
Payment for whole blood donation in the U.S. is prohibited, and while payment for plasma is allowed, there is a stigma attached to payment and much plasma is donated for free.
The pharmaceutical industry has shied away from natural products they cannot patent but they have identified simpler components from plasma, such as clotting factors and immunoglobulins, that have been turned into useful drugs from this raw material of plasma. While some companies have retooled to provide convalescent plasma to treat COVID-19, often paying those donors who have recovered a premium of several times the normal rate, most convalescent plasma has come as donations through traditional blood centers.
In April the Mayo Clinic, in cooperation with the FDA, created an expanded access program for convalescent plasma to treat COVID-19. It was meant to reduce the paperwork associated with gaining access to a treatment not yet approved by the FDA for that disease. Initially it was supposed to be for 5000 units but it quickly grew to more than twenty times that size. Michael Joyner, the head of the program, discussed that experience in an extended interview in September.
The Centers for Medicare and Medicaid Services (CMS) also created associated reimbursement codes, which became permanent in August.
Mayo published an analysis of the first 35,000 patients as a preprint in August. It concluded, "The relationships between mortality and both time to plasma transfusion, and antibody levels provide a signature that is consistent with efficacy for the use of convalescent plasma in the treatment of hospitalized COVID-19 patients."
It seemed to work best when given early in infection and in larger doses; a similar pattern has been seen in studies of monoclonal antibodies. A revised version will soon be published in a major medical journal. Some criticized the findings as not being from a randomized clinical trial.
Convalescent plasma is not the only intervention that seems to work better when used earlier in the course of disease. Recently the pharmaceutical company Eli Lilly stopped a clinical trial of a monoclonal antibody in hospitalized COVID-19 patients when it became apparent it wasn't helping. It is continuing trials for patients who are less sick and begin treatment earlier, as well as in persons who have been exposed to the virus but not yet diagnosed as infected, to see if it might prevent infection. In November the FDA eased access to this drug outside of clinical trials, though it is not yet approved for sale.
Show Me the Money
The antibodies that seem to give plasma its curative powers are fragile proteins that the body produces to fight the virus. Production shuts down once the virus is cleared and the remaining antibodies survive only for a few weeks before the levels fade. [Vaccines are used to train immune cells to produce antibodies and other defenses to respond to exposure to future pathogens.] So they can be usefully harvested from a recovered patient for only a few short weeks or months before they decline precipitously. The question becomes, how does one mobilize this resource in that short window of opportunity?
The program run by the Mayo Clinic explains the process and criteria for donating convalescent plasma for COVID-19, as well as links to local blood centers equipped to handle those free donations. Commercial plasma centers also are advertising and paying for donations.
A majority of countries prohibit paying donors for blood or blood products, including India. But an investigation by India Today touted a black market of people willing to donate convalescent plasma for the equivalent of several hundred dollars. Officials vowed to prosecute, saying donations should be selfless.
But that enforcement threat seemed to be undercut when the health minister of the state of Assam declared "plasma donors will get preference in several government schemes including the government job interview." It appeared to be a form of compensation that far surpassed simple cash.
The small city of Rexburg, Idaho, with a population a bit over 50,000, overwhelmingly Mormon and home to a campus of Brigham Young University, at one point had one of the highest per capita rates of COVID-19 in the current wave of infection. Rumors circulated that some students were intentionally trying to become infected so they could later sell their plasma for top dollar, potentially as much as $200 a visit.
Troubled university officials investigated the allegations but could come up with nothing definitive; how does one prove intentionality with such an omnipresent yet elusive virus? They chalked it up to idle chatter, perhaps an urban legend, which might be associated with alcohol use on some other campus.
Doctors, hospitals, and drug companies are all rightly praised for their altruism in the fight against COVID-19, but they also get paid. Payment for whole blood donation in the U.S. is prohibited, and while payment for plasma is allowed, there is a stigma attached to payment and much plasma is donated for free. "Why do we expect the donors [of convalescent plasma] to be the only uncompensated people in the process? It really makes no sense," argues Mark Yarborough, an ethicist at the UC Davis School of Medicine in Sacramento.
"When I was in grad school, two of my closest friends, at least once a week they went and gave plasma. That was their weekend spending money," Yarborough recalls. He says upper and middle-income people may have the luxury of donating blood products but prohibiting people from selling their plasma is a bit paternalistic and doesn't do anything to improve the economic status of poor people.
"Asking people to dedicate two hours a week for an entire year in exchange for cookies and milk is demonstrably asking too much," says Peter Jaworski, an ethicist who teaches at Georgetown University.
He notes that companies that pay plasma donors have much lower total costs than do operations that rely solely on uncompensated donations. The companies have to spend less to recruit and retain donors because they increase payments to encourage regular repeat donations. They are able to more rationally schedule visits to maximize use of expensive apheresis equipment and medical personnel used for the collection.
It seems that COVID-19 has been with us forever, but in reality it is less than a year. We have learned much over that short time, can now better manage the disease, and have lower mortality rates to prove it. Just how much convalescent plasma may have contributed to that remains an open question. Access to vaccines is months away for many people, and even then some people will continue to get sick. Given the lack of proven treatments, it makes sense to keep plasma as part of the mix, and not close the door to any legitimate means to obtain it.
Time to visit your TikTok doc? The good and bad of doctors on social media
Rakhi Patel is among an increasing number of health care professionals, including doctors and nurses, who maintain an active persona on Instagram, TikTok and other social media sites.
Rakhi Patel has carved a hobby out of reviewing pizza — her favorite food — on Instagram. In a nod to her preferred topping, she calls herself thepepperoniqueen. Photos and videos show her savoring slices from scores of pizzerias. In some of them, she’s wearing scrubs — her attire as an inpatient neurology physician associate at Tufts Medical Center in Boston.
“Depending on how you dress your pizza, it can be more nutritious,” said Patel, who suggests a thin crust, sugarless tomato sauce and vegetables galore as healthier alternatives. “There are no boundaries for a health care professional to enjoy pizza.”
Beyond that, “pizza fuels my mental health and makes me happy, especially when loaded with pepperoni,” she said. “If I’m going to be a pizza connoisseur, then I also need to take care of my physical health by ensuring that I get at least three days of exercise per week and eat nutritiously when I’m not eating pizza.”
She’s among an increasing number of health care professionals, including doctors and nurses, who maintain an active persona on social media, according to bioethics researchers. They share their hobbies and interests with people inside and outside the world of medicine, helping patients and the public become acquainted with the humans behind the scrubs or white coats. Other health care experts limit their posts to medical topics, while some opt for a combination of personal and professional commentaries. Depending on the posts, ethical issues may come into play.
“Health care professionals are quite prevalent on social media,” said Mercer Gary, a postdoctoral researcher at The Hastings Center, an independent bioethics research institute in Garrison, New York. “They’ve been posting on #medTwitter for many years, mainly to communicate with one another, but, of course, anyone can see the threads. Most recently, doctors and nurses have become a presence on TikTok.”
On social media, many health care providers perceive themselves to be “humanizing” their profession by coming across as more approachable — “reminding patients that providers are people and workers, as well as repositories of medical expertise,” Gary said. As a result, she noted that patients who are often intimidated by clinicians may feel comfortable enough to overcome barriers to scheduling health care appointments. The use of TikTok in particular may help doctors and nurses connect with younger followers.
When health care providers post on social media, they must bear in mind that they have legal and ethical duties to their patients, profession and society, said Elizabeth Levy, founder and director of Physicians for Justice.
While enduring three years of pandemic conditions, many health care professionals have struggled with burnout, exhaustion and moral distress. “Much health care provider content on social media seeks to expose the difficulties of the work,” Gary added. “TikTok and Instagram reels have shown health care providers crying after losing a patient or exhausted after a night shift in the emergency department.”
A study conducted in Beijing, China and published last year found that TikTok is the world’s most rapidly growing video application, amassing 1.6 billion users in 2021. “More and more patients are searching for information on genitourinary cancers via TikTok,” the study’s authors wrote in Frontiers in Oncology, referring to cancers of the urinary tracts and male reproductive organs. Among the 61 sample videos examined by the researchers, health care practitioners contributed the content in 29, or 47 percent, of them. Yet, 22 posts, 36 percent, were misinformative, mostly due to outdated information.
More than half of the videos offered good content on disease symptoms and examinations. The authors concluded that “most videos on genitourinary cancers on TikTok are of poor to medium quality and reliability. However, videos posted by media agencies enjoyed great public attention and interaction. Medical practitioners could improve the video quality by cooperating with media agencies and avoiding unexplained terminologies.”
When health care providers post on social media, they must bear in mind that they have legal and ethical duties to their patients, profession and society, said Elizabeth Levy, founder and director of Physicians for Justice in Irvine, Calif., a nonprofit network of volunteer physicians partnering with public interest lawyers to address the social determinants of health.
“Providers are also responsible for understanding the mechanics of their posts,” such as who can see these messages and how long they stay up, Levy said. As a starting point for figuring what’s acceptable, providers could look at social media guidelines put out by their professional associations. Even beyond that, though, they must exercise prudent judgment. “As social media continues to evolve, providers will also need to stay updated with the changing risks and benefits of participation.”
Patients often research their providers online, so finding them on social media can help inform about values and approaches to care, said M. Sara Rosenthal, a professor and founding director of the program for bioethics and chair of the hospital ethics committee at the University of Kentucky College of Medicine.
Health care providers’ posts on social media also could promote patient education. They can advance informed consent and help patients navigate the risks and benefits of various treatments or preventive options. However, providers could violate ethical principles if they espouse “harmful, risky or questionable therapies or medical advice that is contrary to clinical practice guidelines or accepted standards of care,” Rosenthal said.
Inappropriate self-disclosure also can affect a provider’s reputation, said Kelly Michelson, a professor of pediatrics and director of the Center for Bioethics and Medical Humanities at Northwestern University’s Feinberg School of Medicine. A clinician’s obligations to professionalism extend beyond those moments when they are directly taking care of their patients, she said. “Many experts recommend against clinicians ‘friending’ patients or the families on social media because it blurs the patient-clinician boundary.”
Meanwhile, clinicians need to adhere closely to confidentiality. In sharing a patient’s case online for educational purposes, safeguarding identity becomes paramount. Removing names and changing minor details is insufficient, Michelson said.
“The patient-clinician relationship is sacred, and it can only be effective if patients have 100 percent confidence that all that happens with their clinician is kept in the strictest of confidence,” she said, adding that health care providers also should avoid obtaining information about their patients from social media because it can lead to bias and risk jeopardizing objectivity.
Academic clinicians can use social media as a recruitment tool to expand the pool of research participants for their studies, Michelson said. Because the majority of clinical research is conducted at academic medical centers, large segments of the population are excluded. “This affects the quality of the data and knowledge we gain from research,” she said.
Don S. Dizon, a professor of medicine and surgery at the Warren Alpert Medical School of Brown University in Providence, Rhode Island, uses LinkedIn and Doximity, as well as Twitter, Instagram, TikTok, Facebook, and most recently, YouTube and Post. He’s on Twitter nearly every day, where he interacts with the oncology community and his medical colleagues.
Also, he said, “I really like Instagram. It’s where you will see a hybrid of who I am professionally and personally. I’ve become comfortable sharing both up to a limit, but where else can I combine my appreciation of clothes with my professional life?” On that site, he’s seen sporting shirts with polka dots or stripes and an occasional bow-tie. He also posts photos of his cats.

Don S. Dizon, a professor of medicine and surgery at Brown, started using TikTok several years ago, telling medical stories in short-form videos.
Don S. Dizon
Dizon started using TikTok several years ago, telling medical stories in short-form videos. He may talk about an inspirational patient, his views on end-of-life care and death, or memories of people who have passed. But he is careful not to divulge any details that would identify anyone.
Recently, some people have become his patients after viewing his content on social media or on the Internet in general, which he clearly states isn’t a forum for medical advice. “In both situations, they are so much more relaxed when we meet, because it’s as if they have a sense of who I am as a person,” Dizon said. “I think that has helped so much in talking through a cancer diagnosis and a treatment plan, and yes, even discussions about prognosis.”
He also posts about equity and diversity. “I have found myself more likely to repost or react to issues that are inherently political, including racism, homophobia, transphobia and lack-of-access issues, because medicine is not isolated from society, and I truly believe that medicine is a social justice issue,” said Dizon, who is vice chair of diversity, equity, inclusion and professional integrity at the SWOG Cancer Research Network.
Through it all, Dizon likes “to break through the notion of doctor as infallible and all-knowing, the doctor as deity,” he said. “Humanizing what I do, especially in oncology, is something that challenges me on social media, and I appreciate the opportunities to do it on TikTok.”
Could this habit related to eating slow down rates of aging?
Previous research showed that restricting calories results in longer lives for mice, worms and flies. A new study by Columbia University researchers applied those findings to people. But what does this paper actually show?
Last Thursday, scientists at Columbia University published a new study finding that cutting down on calories could lead to longer, healthier lives. In the phase 2 trial, 220 healthy people without obesity dropped their calories significantly and, at least according to one test, their rate of biological aging slowed by 2 to 3 percent in over a couple of years. Small though that may seem, the researchers estimate that it would translate into a decline of about 10 percent in the risk of death as people get older. That's basically the same as quitting smoking.
Previous research has shown that restricting calories results in longer lives for mice, worms and flies. This research is unique because it applies those findings to people. It was published in Nature Aging.
But what did the researchers actually show? Why did two other tests indicate that the biological age of the research participants didn't budge? Does the new paper point to anything people should be doing for more years of healthy living? Spoiler alert: Maybe, but don't try anything before talking with a medical expert about it. I had the chance to chat with someone with inside knowledge of the research -- Dr. Evan Hadley, director of the National Institute of Aging's Division of Geriatrics and Clinical Gerontology, which funded the study. Dr. Hadley describes how the research participants went about reducing their calories, as well as the risks and benefits involved. He also explains the "aging clock" used to measure the benefits.
Evan Hadley, Director of the Division of Geriatrics and Clinical Gerontology at the National Institute of Aging
NIA

