A blood test may catch colorectal cancer before it's too late
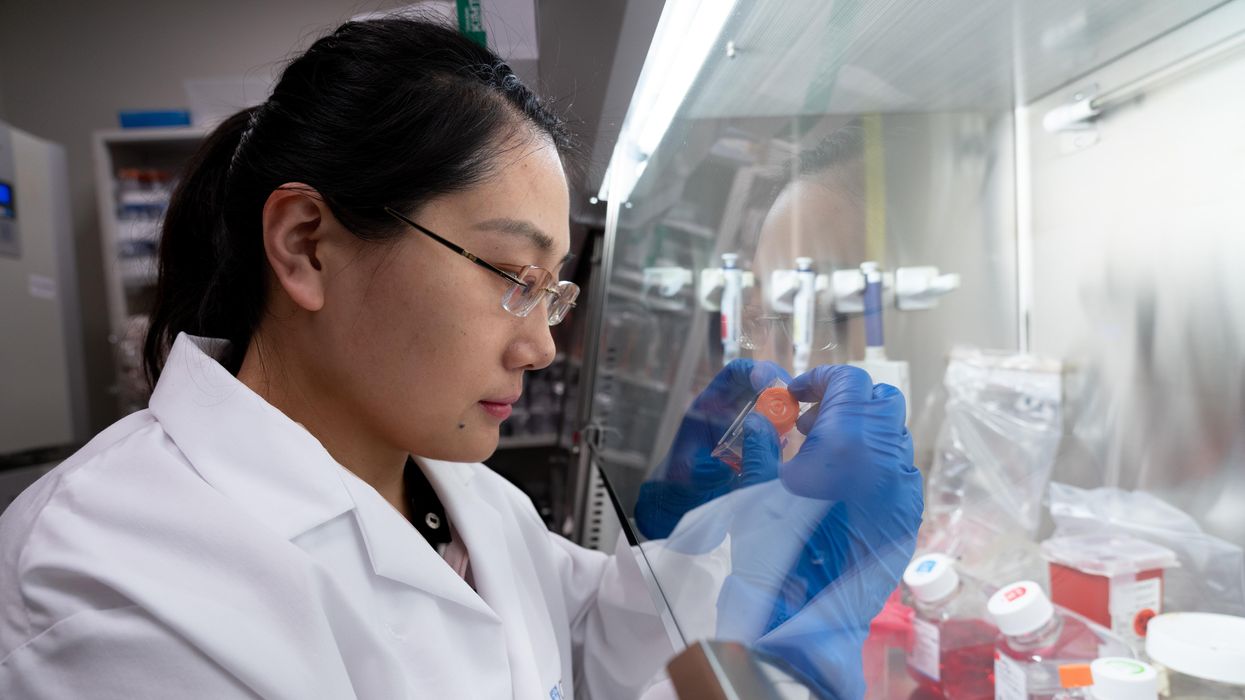
A scientist works on a blood test in the Ajay Goel Lab, one of many labs that are developing blood tests to screen for different types of cancer.
Soon it may be possible to find different types of cancer earlier than ever through a simple blood test.
Among the many blood tests in development, researchers announced in July that they have developed one that may screen for early-onset colorectal cancer. The new potential screening tool, detailed in a study in the journal Gastroenterology, represents a major step in noninvasively and inexpensively detecting nonhereditary colorectal cancer at an earlier and more treatable stage.
In recent years, this type of cancer has been on the upswing in adults under age 50 and in those without a family history. In 2021, the American Cancer Society's revised guidelines began recommending that colorectal cancer screenings with colonoscopy begin at age 45. But that still wouldn’t catch many early-onset cases among people in their 20s and 30s, says Ajay Goel, professor and chair of molecular diagnostics and experimental therapeutics at City of Hope, a Los Angeles-based nonprofit cancer research and treatment center that developed the new blood test.
“These people will mostly be missed because they will never be screened for it,” Goel says. Overall, colorectal cancer is the fourth most common malignancy, according to the U.S. Centers for Disease Control and Prevention.
Goel is far from the only one working on this. Dozens of companies are in the process of developing blood tests to screen for different types of malignancies.
Some estimates indicate that between one-fourth and one-third of all newly diagnosed colorectal cancers are early-onset. These patients generally present with more aggressive and advanced disease at diagnosis compared to late-onset colorectal cancer detected in people 50 years or older.
To develop his test, Goel examined publicly available datasets and figured out that changes in novel microRNAs, or miRNAs, which regulate the expression of genes, occurred in people with early-onset colorectal cancer. He confirmed these biomarkers by looking for them in the blood of 149 patients who had the early-onset form of the disease. In particular, Goel and his team of researchers were able to pick out four miRNAs that serve as a telltale sign of this cancer when they’re found in combination with each other.
The blood test is being validated by following another group of patients with early-onset colorectal cancer. “We have filed for intellectual property on this invention and are currently seeking biotech/pharma partners to license and commercialize this invention,” Goel says.
He’s far from the only one working on this. Dozens of companies are in the process of developing blood tests to screen for different types of malignancies, says Timothy Rebbeck, a professor of cancer prevention at the Harvard T.H. Chan School of Public Health and the Dana-Farber Cancer Institute. But, he adds, “It’s still very early, and the technology still needs a lot of work before it will revolutionize early detection.”
The accuracy of the early detection blood tests for cancer isn’t yet where researchers would like it to be. To use these tests widely in people without cancer, a very high degree of precision is needed, says David VanderWeele, interim director of the OncoSET Molecular Tumor Board at Northwestern University’s Lurie Cancer Center in Chicago.
Otherwise, “you’re going to cause a lot of anxiety unnecessarily if people have false-positive tests,” VanderWeele says. So far, “these tests are better at finding cancer when there’s a higher burden of cancer present,” although the goal is to detect cancer at the earliest stages. Even so, “we are making progress,” he adds.
While early detection is known to improve outcomes, most cancers are detected too late, often after they metastasize and people develop symptoms. Only five cancer types have recommended standard screenings, none of which involve blood tests—breast, cervical, colorectal, lung (smokers considered at risk) and prostate cancers, says Trish Rowland, vice president of corporate communications at GRAIL, a biotechnology company in Menlo Park, Calif., which developed a multi-cancer early detection blood test.
These recommended screenings check for individual cancers rather than looking for any form of cancer someone may have. The devil lies in the fact that cancers without widespread screening recommendations represent the vast majority of cancer diagnoses and most cancer deaths.
GRAIL’s Galleri multi-cancer early detection test is designed to find more cancers at earlier stages by analyzing DNA shed into the bloodstream by cells—with as few false positives as possible, she says. The test is currently available by prescription only for those with an elevated risk of cancer. Consumers can request it from their healthcare or telemedicine provider. “Galleri can detect a shared cancer signal across more than 50 types of cancers through a simple blood draw,” Rowland says, adding that it can be integrated into annual health checks and routine blood work.
Cancer patients—even those with early and curable disease—often have tumor cells circulating in their blood. “These tumor cells act as a biomarker and can be used for cancer detection and diagnosis,” says Andrew Wang, a radiation oncologist and professor at the University of Texas Southwestern Medical Center in Dallas. “Our research goal is to be able to detect these tumor cells to help with cancer management.” Collaborating with Seungpyo Hong, the Milton J. Henrichs Chair and Professor at the University of Wisconsin-Madison School of Pharmacy, “we have developed a highly sensitive assay to capture these circulating tumor cells.”
Even if the quality of a blood test is superior, finding cancer early doesn’t always mean it’s absolutely best to treat it. For example, prostate cancer treatment’s potential side effects—the inability to control urine or have sex—may be worse than living with a slow-growing tumor that is unlikely to be fatal. “[The test] needs to tell me, am I going to die of that cancer? And, if I intervene, will I live longer?” says John Marshall, chief of hematology and oncology at Medstar Georgetown University Hospital in Washington, D.C.

Ajay Goel Lab
A blood test developed at the University of Texas MD Anderson Cancer Center in Houston helps predict who may benefit from lung cancer screening when it is combined with a risk model based on an individual’s smoking history, according to a study published in January in the Journal of Clinical Oncology. The personalized lung cancer risk assessment was more sensitive and specific than the 2021 and 2013 U.S. Preventive Services Task Force criteria.
The study involved participants from the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial with a minimum of a 10 pack-year smoking history, meaning they smoked 20 cigarettes per day for ten years. If implemented, the blood test plus model would have found 9.2 percent more lung cancer cases for screening and decreased referral to screening among non-cases by 13.7 percent compared to the 2021 task force criteria, according to Oncology Times.
The conventional type of screening for lung cancer is an annual low-dose CT scan, but only a small percentage of people who are eligible will actually get these scans, says Sam Hanash, professor of clinical cancer prevention and director of MD Anderson’s Center for Global Cancer Early Detection. Such screening is not readily available in most countries.
In methodically searching for blood-based biomarkers for lung cancer screening, MD Anderson researchers developed a simple test consisting of four proteins. These proteins circulating in the blood were at high levels in individuals who had lung cancer or later developed it, Hanash says.
“The interest in blood tests for cancer early detection has skyrocketed in the past few years,” he notes, “due in part to advances in technology and a better understanding of cancer causation, cancer drivers and molecular changes that occur with cancer development.”
However, at the present time, none of the blood tests being considered eliminate the need for screening of eligible subjects using established methods, such as colonoscopy for colorectal cancer. Yet, Hanash says, “they have the potential to complement these modalities.”
The large genetic studies underlying certain disease risk tests have primarily been done in populations of European ancestry, limiting their accuracy.
Earlier this year, California-based Ambry Genetics announced that it was discontinuing a test meant to estimate a person's risk of developing prostate or breast cancer. The test looks for variations in a person's DNA that are known to be associated with these cancers.
Known as a polygenic risk score, this type of test adds up the effects of variants in many genes — often in the dozens or hundreds — and calculates a person's risk of developing a particular health condition compared to other people. In this way, polygenic risk scores are different from traditional genetic tests that look for mutations in single genes, such as BRCA1 and BRCA2, which raise the risk of breast cancer.
Traditional genetic tests look for mutations that are relatively rare in the general population but have a large impact on a person's disease risk, like BRCA1 and BRCA2. By contrast, polygenic risk scores scan for more common genetic variants that, on their own, have a small effect on risk. Added together, however, they can raise a person's risk for developing disease.
These scores could become a part of routine healthcare in the next few years. Researchers are developing polygenic risk scores for cancer, heart, disease, diabetes and even depression. Before they can be rolled out widely, they'll have to overcome a key limitation: racial bias.
"The issue with these polygenic risk scores is that the scientific studies which they're based on have primarily been done in individuals of European ancestry," says Sara Riordan, president of the National Society of Genetics Counselors. These scores are calculated by comparing the genetic data of people with and without a particular disease. To make these scores accurate, researchers need genetic data from tens or hundreds of thousands of people.
Myriad's old test would have shown that a Black woman had twice as high of a risk for breast cancer compared to the average woman even if she was at low or average risk.
A 2018 analysis found that 78% of participants included in such large genetic studies, known as genome-wide association studies, were of European descent. That's a problem, because certain disease-associated genetic variants don't appear equally across different racial and ethnic groups. For example, a particular variant in the TTR gene, known as V1221, occurs more frequently in people of African descent. In recent years, the variant has been found in 3 to 4 percent of individuals of African ancestry in the United States. Mutations in this gene can cause protein to build up in the heart, leading to a higher risk of heart failure. A polygenic risk score for heart disease based on genetic data from mostly white people likely wouldn't give accurate risk information to African Americans.
Accuracy in genetic testing matters because such polygenic risk scores could help patients and their doctors make better decisions about their healthcare.
For instance, if a polygenic risk score determines that a woman is at higher-than-average risk of breast cancer, her doctor might recommend more frequent mammograms — X-rays that take a picture of the breast. Or, if a risk score reveals that a patient is more predisposed to heart attack, a doctor might prescribe preventive statins, a type of cholesterol-lowering drug.
"Let's be clear, these are not diagnostic tools," says Alicia Martin, a population and statistical geneticist at the Broad Institute of MIT and Harvard. "We can't use a polygenic score to say you will or will not get breast cancer or have a heart attack."
But combining a patient's polygenic risk score with other factors that affect disease risk — like age, weight, medication use or smoking status — may provide a better sense of how likely they are to develop a specific health condition than considering any one risk factor one its own. The accuracy of polygenic risk scores becomes even more important when considering that these scores may be used to guide medication prescription or help patients make decisions about preventive surgery, such as a mastectomy.
In a study published in September, researchers used results from large genetics studies of people with European ancestry and data from the UK Biobank to calculate polygenic risk scores for breast and prostate cancer for people with African, East Asian, European and South Asian ancestry. They found that they could identify individuals at higher risk of breast and prostate cancer when they scaled the risk scores within each group, but the authors say this is only a temporary solution. Recruiting more diverse participants for genetics studies will lead to better cancer detection and prevent, they conclude.
Recent efforts to do just that are expected to make these scores more accurate in the future. Until then, some genetics companies are struggling to overcome the European bias in their tests.
Acknowledging the limitations of its polygenic risk score, Ambry Genetics said in April that it would stop offering the test until it could be recalibrated. The company launched the test, known as AmbryScore, in 2018.
"After careful consideration, we have decided to discontinue AmbryScore to help reduce disparities in access to genetic testing and to stay aligned with current guidelines," the company said in an email to customers. "Due to limited data across ethnic populations, most polygenic risk scores, including AmbryScore, have not been validated for use in patients of diverse backgrounds." (The company did not make a spokesperson available for an interview for this story.)
In September 2020, the National Comprehensive Cancer Network updated its guidelines to advise against the use of polygenic risk scores in routine patient care because of "significant limitations in interpretation." The nonprofit, which represents 31 major cancer cancers across the United States, said such scores could continue to be used experimentally in clinical trials, however.
Holly Pederson, director of Medical Breast Services at the Cleveland Clinic, says the realization that polygenic risk scores may not be accurate for all races and ethnicities is relatively recent. Pederson worked with Salt Lake City-based Myriad Genetics, a leading provider of genetic tests, to improve the accuracy of its polygenic risk score for breast cancer.
The company announced in August that it had recalibrated the test, called RiskScore, for women of all ancestries. Previously, Myriad did not offer its polygenic risk score to women who self-reported any ancestry other than sole European or Ashkenazi ancestry.
"Black women, while they have a similar rate of breast cancer to white women, if not lower, had twice as high of a polygenic risk score because the development and validation of the model was done in white populations," Pederson said of the old test. In other words, Myriad's old test would have shown that a Black woman had twice as high of a risk for breast cancer compared to the average woman even if she was at low or average risk.
To develop and validate the new score, Pederson and other researchers assessed data from more than 275,000 women, including more than 31,000 African American women and nearly 50,000 women of East Asian descent. They looked at 56 different genetic variants associated with ancestry and 93 associated with breast cancer. Interestingly, they found that at least 95% of the breast cancer variants were similar amongst the different ancestries.
The company says the resulting test is now more accurate for all women across the board, but Pederson cautions that it's still slightly less accurate for Black women.
"It's not only the lack of data from Black women that leads to inaccuracies and a lack of validation in these types of risk models, it's also the pure genomic diversity of Africa," she says, noting that Africa is the most genetically diverse continent on the planet. "We just need more data, not only in American Black women but in African women to really further characterize that continent."
Martin says it's problematic that such scores are most accurate for white people because they could further exacerbate health disparities in traditionally underserved groups, such as Black Americans. "If we were to set up really representative massive genetic studies, we would do a much better job at predicting genetic risk for everybody," she says.
Earlier this year, the National Institutes of Health awarded $38 million to researchers to improve the accuracy of polygenic risk scores in diverse populations. Researchers will create new genome datasets and pool information from existing ones in an effort to diversify the data that polygenic scores rely on. They plan to make these datasets available to other scientists to use.
"By having adequate representation, we can ensure that the results of a genetic test are widely applicable," Riordan says.
New Podcast: George Church on Woolly Mammoths, Organ Transplants, and Covid Vaccines
Dr. George Church, a leading pioneer of gene editing, updates our listeners on several of his noteworthy projects.
The "Making Sense of Science" podcast features interviews with leading medical and scientific experts about the latest developments and the big ethical and societal questions they raise. This monthly podcast is hosted by journalist Kira Peikoff, founding editor of the award-winning science outlet Leaps.org.
This month, our guest is notable genetics pioneer Dr. George Church of Harvard Medical School. Dr. Church has remarkably bold visions for how innovation in science can fundamentally transform the future of humanity and our planet. His current moonshot projects include: de-extincting some of the woolly mammoth's genes to create a hybrid Asian elephant with the cold-tolerance traits of the woolly mammoth, so that this animal can re-populate the Arctic and help stave off climate change; reversing chronic diseases of aging through gene therapy, which he and colleagues are now testing in dogs; and transplanting genetically engineered pig organs to humans to eliminate the tragically long waiting lists for organs. Hear Dr. Church discuss all this and more on our latest episode.
Watch the Trailer:
Listen to the Episode:
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.