A blood test may catch colorectal cancer before it's too late
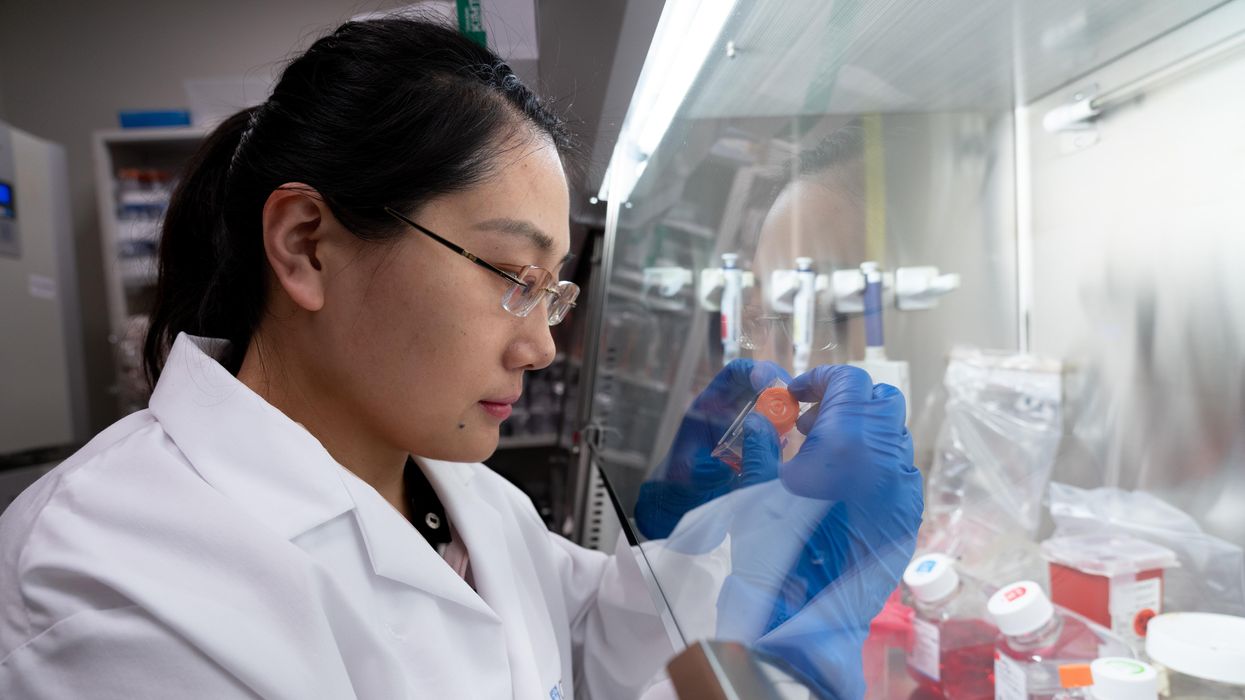
A scientist works on a blood test in the Ajay Goel Lab, one of many labs that are developing blood tests to screen for different types of cancer.
Soon it may be possible to find different types of cancer earlier than ever through a simple blood test.
Among the many blood tests in development, researchers announced in July that they have developed one that may screen for early-onset colorectal cancer. The new potential screening tool, detailed in a study in the journal Gastroenterology, represents a major step in noninvasively and inexpensively detecting nonhereditary colorectal cancer at an earlier and more treatable stage.
In recent years, this type of cancer has been on the upswing in adults under age 50 and in those without a family history. In 2021, the American Cancer Society's revised guidelines began recommending that colorectal cancer screenings with colonoscopy begin at age 45. But that still wouldn’t catch many early-onset cases among people in their 20s and 30s, says Ajay Goel, professor and chair of molecular diagnostics and experimental therapeutics at City of Hope, a Los Angeles-based nonprofit cancer research and treatment center that developed the new blood test.
“These people will mostly be missed because they will never be screened for it,” Goel says. Overall, colorectal cancer is the fourth most common malignancy, according to the U.S. Centers for Disease Control and Prevention.
Goel is far from the only one working on this. Dozens of companies are in the process of developing blood tests to screen for different types of malignancies.
Some estimates indicate that between one-fourth and one-third of all newly diagnosed colorectal cancers are early-onset. These patients generally present with more aggressive and advanced disease at diagnosis compared to late-onset colorectal cancer detected in people 50 years or older.
To develop his test, Goel examined publicly available datasets and figured out that changes in novel microRNAs, or miRNAs, which regulate the expression of genes, occurred in people with early-onset colorectal cancer. He confirmed these biomarkers by looking for them in the blood of 149 patients who had the early-onset form of the disease. In particular, Goel and his team of researchers were able to pick out four miRNAs that serve as a telltale sign of this cancer when they’re found in combination with each other.
The blood test is being validated by following another group of patients with early-onset colorectal cancer. “We have filed for intellectual property on this invention and are currently seeking biotech/pharma partners to license and commercialize this invention,” Goel says.
He’s far from the only one working on this. Dozens of companies are in the process of developing blood tests to screen for different types of malignancies, says Timothy Rebbeck, a professor of cancer prevention at the Harvard T.H. Chan School of Public Health and the Dana-Farber Cancer Institute. But, he adds, “It’s still very early, and the technology still needs a lot of work before it will revolutionize early detection.”
The accuracy of the early detection blood tests for cancer isn’t yet where researchers would like it to be. To use these tests widely in people without cancer, a very high degree of precision is needed, says David VanderWeele, interim director of the OncoSET Molecular Tumor Board at Northwestern University’s Lurie Cancer Center in Chicago.
Otherwise, “you’re going to cause a lot of anxiety unnecessarily if people have false-positive tests,” VanderWeele says. So far, “these tests are better at finding cancer when there’s a higher burden of cancer present,” although the goal is to detect cancer at the earliest stages. Even so, “we are making progress,” he adds.
While early detection is known to improve outcomes, most cancers are detected too late, often after they metastasize and people develop symptoms. Only five cancer types have recommended standard screenings, none of which involve blood tests—breast, cervical, colorectal, lung (smokers considered at risk) and prostate cancers, says Trish Rowland, vice president of corporate communications at GRAIL, a biotechnology company in Menlo Park, Calif., which developed a multi-cancer early detection blood test.
These recommended screenings check for individual cancers rather than looking for any form of cancer someone may have. The devil lies in the fact that cancers without widespread screening recommendations represent the vast majority of cancer diagnoses and most cancer deaths.
GRAIL’s Galleri multi-cancer early detection test is designed to find more cancers at earlier stages by analyzing DNA shed into the bloodstream by cells—with as few false positives as possible, she says. The test is currently available by prescription only for those with an elevated risk of cancer. Consumers can request it from their healthcare or telemedicine provider. “Galleri can detect a shared cancer signal across more than 50 types of cancers through a simple blood draw,” Rowland says, adding that it can be integrated into annual health checks and routine blood work.
Cancer patients—even those with early and curable disease—often have tumor cells circulating in their blood. “These tumor cells act as a biomarker and can be used for cancer detection and diagnosis,” says Andrew Wang, a radiation oncologist and professor at the University of Texas Southwestern Medical Center in Dallas. “Our research goal is to be able to detect these tumor cells to help with cancer management.” Collaborating with Seungpyo Hong, the Milton J. Henrichs Chair and Professor at the University of Wisconsin-Madison School of Pharmacy, “we have developed a highly sensitive assay to capture these circulating tumor cells.”
Even if the quality of a blood test is superior, finding cancer early doesn’t always mean it’s absolutely best to treat it. For example, prostate cancer treatment’s potential side effects—the inability to control urine or have sex—may be worse than living with a slow-growing tumor that is unlikely to be fatal. “[The test] needs to tell me, am I going to die of that cancer? And, if I intervene, will I live longer?” says John Marshall, chief of hematology and oncology at Medstar Georgetown University Hospital in Washington, D.C.

Ajay Goel Lab
A blood test developed at the University of Texas MD Anderson Cancer Center in Houston helps predict who may benefit from lung cancer screening when it is combined with a risk model based on an individual’s smoking history, according to a study published in January in the Journal of Clinical Oncology. The personalized lung cancer risk assessment was more sensitive and specific than the 2021 and 2013 U.S. Preventive Services Task Force criteria.
The study involved participants from the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial with a minimum of a 10 pack-year smoking history, meaning they smoked 20 cigarettes per day for ten years. If implemented, the blood test plus model would have found 9.2 percent more lung cancer cases for screening and decreased referral to screening among non-cases by 13.7 percent compared to the 2021 task force criteria, according to Oncology Times.
The conventional type of screening for lung cancer is an annual low-dose CT scan, but only a small percentage of people who are eligible will actually get these scans, says Sam Hanash, professor of clinical cancer prevention and director of MD Anderson’s Center for Global Cancer Early Detection. Such screening is not readily available in most countries.
In methodically searching for blood-based biomarkers for lung cancer screening, MD Anderson researchers developed a simple test consisting of four proteins. These proteins circulating in the blood were at high levels in individuals who had lung cancer or later developed it, Hanash says.
“The interest in blood tests for cancer early detection has skyrocketed in the past few years,” he notes, “due in part to advances in technology and a better understanding of cancer causation, cancer drivers and molecular changes that occur with cancer development.”
However, at the present time, none of the blood tests being considered eliminate the need for screening of eligible subjects using established methods, such as colonoscopy for colorectal cancer. Yet, Hanash says, “they have the potential to complement these modalities.”
Podcast: Should Scientific Controversies Be Silenced?
The recent Joe Rogan/Spotify controversy prompts the consideration of tough questions about expertise, trust, gatekeepers, and dissent.
The "Making Sense of Science" podcast features interviews with leading medical and scientific experts about the latest developments and the big ethical and societal questions they raise. This monthly podcast is hosted by journalist Kira Peikoff, founding editor of the award-winning science outlet Leaps.org.
The recent Joe Rogan/Spotify backlash over the misinformation presented in his recent episode on the Covid-19 vaccines raises some difficult and important bioethical questions for society: How can people know which experts to trust? What should big tech gatekeepers do about false claims promoted on their platforms? How should the scientific establishment respond to heterodox viewpoints from experts who disagree with the consensus? When is silencing of dissent merited, and when is it problematic? Journalist Kira Peikoff asks infectious disease physician and pandemic scholar Dr. Amesh Adalja to weigh in.

Dr. Amesh Adalja, Senior Scholar, Johns Hopkins Center for Health Security and an infectious disease physician
Listen to the Episode
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Scientists Are Studying How to Help Dogs Have Longer Lives, in a Bid to Further Our Own
Feeding dogs only once a day is showing health benefits in a large study, scientists report.
The sad eyes. The wagging tail. The frustrated whine. The excited bark. Dogs know how to get their owners to fork over the food more often.
The extra calories dogs get from feeding patterns now used by many Americans may not be good for them from a health and longevity viewpoint. In research from a large study called the Dog Aging Project, canines fed once a day had better scores on cognition tests and lower odds of developing diseases of organs throughout the body: intestinal tract, mouth and teeth, bones and joints, kidneys and bladder, and liver and pancreas.
Fewer than 1 in 10 dog owners fed their furry friends once daily, while nearly three fourths provided two daily meals.
“Most veterinarians have been led to believe that feeding dogs twice a day is optimal, but this is a relatively new idea that has developed over the past few decades with little supportive evidence from a health standpoint,” said Matt Kaeberlein, PhD, Co-Director of the Dog Aging Project, a professor of pathology and Director of the Healthy Aging and Longevity Research Institute at the University of Washington. Kaeberlein studies basic mechanisms of aging to find ways of extending the healthspan, the number of years of life lived free of disease. It’s not enough to extend the lifespan unless declines in biological function and risks of age-related diseases are also studied, he believes, hence the healthspan.
The Dog Aging Project is studying tens of thousands of dogs living with their owners in the real world, not a biology laboratory. The feeding study is the first of several reports now coming from the project based on owners’ annual reports of demographics, physical activity, environment, dog behavior, diet, medications and supplements, and health status. It has been posted on bioRxiv as it goes through peer review.
“All available evidence suggests that most biological mechanisms of aging in dogs will be conserved in humans. It just happens much faster in dogs.”
“The Dog Aging Project is one of the most exciting in the longevity space,” said David A. Sinclair, professor in the Department of Genetics and co-director of the Paul F. Glenn Center for Biology of Aging Research at Harvard Medical School. “Not only is it important to help our companions live longer and healthier, but because they are like people and share the same environment and many of the lifestyles as their owners, they are the perfect model for human longevity interventions.”
The epigenetic clock — and specifically changes in gene expression resulting from methylation of cytosine and guanine in the DNA — provides the critical connection between aging in dogs and people. “All available evidence suggests that most biological mechanisms of aging in dogs will be conserved in humans,” Kaeberlein said. “It just happens much faster in dogs.” These methylation changes, called the “methylomes,” have been associated with rates of aging in dogs, humans, and also mice.
In a 2020 study young dogs matched with young adults and aged dogs matched with older adults showed the greatest similarities in methylomes. In the Cell Systems report, Tina Wang of the University of California, San Diego, and colleagues wrote that the methylome “can be used to quantitatively translate the age-related physiology experienced by one organism (i.e., a model species like dog) to the age at which physiology in a second organism is most similar (i.e., a second model or humans).” This allows rates of aging in one species to be mapped onto aging in another species, providing “a compelling tool in the quest to understand aging and identify interventions for maximizing healthy lifespan.”
In the Dog Aging Project study, 8% of 24,238 owners fed their dogs once daily, the same as the percentage of owners serving three daily meals. Twice-daily feedings were most common (73%), and just over 1 in 10 owners (11%) “free fed” their dogs by just filling up the bowl whenever it was empty — most likely Rover’s favorite option.
“The notion of breakfast, lunch, and dinner for people in the United States is not based on large studies that compared three meals a day to two meals a day, or to four, “ said Kate E. Creevy, chief veterinary officer with the Dog Aging Project and associate professor at Texas A&M University. “It’s more about what we are accustomed to. Similarly, there are not large population studies comparing outcomes of dogs fed once, twice, or three times a day.”
“We do not recommend that people change their dogs’ diets based on this report,” Creevy emphasized. “It’s important to understand the difference between research that finds associations versus research that finds cause and effect.”
To establish cause and effect, the Dog Aging Project will follow their cohort over many years. Then, Creevy said, “We will be able to determine whether the associations we have found with feeding frequency are causes, or effects, or neither.”
While not yet actionable, the feeding findings fit with biology across a variety of animals, Kaeberlein said, including indicators that better health translates into longer healthspans. He said that caloric restriction and perhaps time-restricted eating or intermittent fasting — all ways that some human diets are structured — can have a positive impact on the biology of aging by allowing the gastrointestinal tract to have time each day to rest and repair itself, just as sleep benefits the brain through rest.
Timing of meals is also related to the concept of ketogenesis, Kaeberlein explained. Without access to glucose, animals switch over to a ketogenic state in which back-up systems produce energy through metabolic pathways that generate ketones. Mice go into this state very quickly, after a few hours or an overnight fast, while people shift to ketogenesis more slowly, from a few hours to up to 36 hours for people on typical Western diets, Kaeberlein said.
Dogs are different. They take at least two days to shift to ketogenesis, suggesting they have evolved to need fewer meals that are spaced out rather than the multiple daily meals plus snacks that people prefer.
As this relates to longevity, Kaeberlein said that a couple of studies show that mice who are fed a ketogenic diet have longer lifespans (years of life regardless of health). “For us, the next step is to analyze the composition of the dogs’ diets or the relationship of multiple daily feedings with obesity,” he said. “Maybe not being obese is related to better health.”
To learn more, the Dog Aging Project needs dogs — lots of dogs! Kaeberlein wants at least 100,000 dogs, including small dogs, large dogs, dogs of all ages. Puppies are needed for the researchers to follow across their lifespan. The project has an excellent website where owners can volunteer to participate.
Nutritional strategies are often not built around sound scientific principles, Kaeberlein said. In human nutrition, people have tried all kinds of diets over the years, including some that were completely wrong. Kaeberlein and his colleagues in the Dog Aging Project want to change that, at least for people’s canine companions, and hopefully, as a result, give dogs added years of healthy life and provide clues for human nutrition.
After that, maybe they can do something about those sad eyes and the frustrated whine.