A blood test may catch colorectal cancer before it's too late
A scientist works on a blood test in the Ajay Goel Lab, one of many labs that are developing blood tests to screen for different types of cancer.
Soon it may be possible to find different types of cancer earlier than ever through a simple blood test.
Among the many blood tests in development, researchers announced in July that they have developed one that may screen for early-onset colorectal cancer. The new potential screening tool, detailed in a study in the journal Gastroenterology, represents a major step in noninvasively and inexpensively detecting nonhereditary colorectal cancer at an earlier and more treatable stage.
In recent years, this type of cancer has been on the upswing in adults under age 50 and in those without a family history. In 2021, the American Cancer Society's revised guidelines began recommending that colorectal cancer screenings with colonoscopy begin at age 45. But that still wouldn’t catch many early-onset cases among people in their 20s and 30s, says Ajay Goel, professor and chair of molecular diagnostics and experimental therapeutics at City of Hope, a Los Angeles-based nonprofit cancer research and treatment center that developed the new blood test.
“These people will mostly be missed because they will never be screened for it,” Goel says. Overall, colorectal cancer is the fourth most common malignancy, according to the U.S. Centers for Disease Control and Prevention.
Goel is far from the only one working on this. Dozens of companies are in the process of developing blood tests to screen for different types of malignancies.
Some estimates indicate that between one-fourth and one-third of all newly diagnosed colorectal cancers are early-onset. These patients generally present with more aggressive and advanced disease at diagnosis compared to late-onset colorectal cancer detected in people 50 years or older.
To develop his test, Goel examined publicly available datasets and figured out that changes in novel microRNAs, or miRNAs, which regulate the expression of genes, occurred in people with early-onset colorectal cancer. He confirmed these biomarkers by looking for them in the blood of 149 patients who had the early-onset form of the disease. In particular, Goel and his team of researchers were able to pick out four miRNAs that serve as a telltale sign of this cancer when they’re found in combination with each other.
The blood test is being validated by following another group of patients with early-onset colorectal cancer. “We have filed for intellectual property on this invention and are currently seeking biotech/pharma partners to license and commercialize this invention,” Goel says.
He’s far from the only one working on this. Dozens of companies are in the process of developing blood tests to screen for different types of malignancies, says Timothy Rebbeck, a professor of cancer prevention at the Harvard T.H. Chan School of Public Health and the Dana-Farber Cancer Institute. But, he adds, “It’s still very early, and the technology still needs a lot of work before it will revolutionize early detection.”
The accuracy of the early detection blood tests for cancer isn’t yet where researchers would like it to be. To use these tests widely in people without cancer, a very high degree of precision is needed, says David VanderWeele, interim director of the OncoSET Molecular Tumor Board at Northwestern University’s Lurie Cancer Center in Chicago.
Otherwise, “you’re going to cause a lot of anxiety unnecessarily if people have false-positive tests,” VanderWeele says. So far, “these tests are better at finding cancer when there’s a higher burden of cancer present,” although the goal is to detect cancer at the earliest stages. Even so, “we are making progress,” he adds.
While early detection is known to improve outcomes, most cancers are detected too late, often after they metastasize and people develop symptoms. Only five cancer types have recommended standard screenings, none of which involve blood tests—breast, cervical, colorectal, lung (smokers considered at risk) and prostate cancers, says Trish Rowland, vice president of corporate communications at GRAIL, a biotechnology company in Menlo Park, Calif., which developed a multi-cancer early detection blood test.
These recommended screenings check for individual cancers rather than looking for any form of cancer someone may have. The devil lies in the fact that cancers without widespread screening recommendations represent the vast majority of cancer diagnoses and most cancer deaths.
GRAIL’s Galleri multi-cancer early detection test is designed to find more cancers at earlier stages by analyzing DNA shed into the bloodstream by cells—with as few false positives as possible, she says. The test is currently available by prescription only for those with an elevated risk of cancer. Consumers can request it from their healthcare or telemedicine provider. “Galleri can detect a shared cancer signal across more than 50 types of cancers through a simple blood draw,” Rowland says, adding that it can be integrated into annual health checks and routine blood work.
Cancer patients—even those with early and curable disease—often have tumor cells circulating in their blood. “These tumor cells act as a biomarker and can be used for cancer detection and diagnosis,” says Andrew Wang, a radiation oncologist and professor at the University of Texas Southwestern Medical Center in Dallas. “Our research goal is to be able to detect these tumor cells to help with cancer management.” Collaborating with Seungpyo Hong, the Milton J. Henrichs Chair and Professor at the University of Wisconsin-Madison School of Pharmacy, “we have developed a highly sensitive assay to capture these circulating tumor cells.”
Even if the quality of a blood test is superior, finding cancer early doesn’t always mean it’s absolutely best to treat it. For example, prostate cancer treatment’s potential side effects—the inability to control urine or have sex—may be worse than living with a slow-growing tumor that is unlikely to be fatal. “[The test] needs to tell me, am I going to die of that cancer? And, if I intervene, will I live longer?” says John Marshall, chief of hematology and oncology at Medstar Georgetown University Hospital in Washington, D.C.

Ajay Goel Lab
A blood test developed at the University of Texas MD Anderson Cancer Center in Houston helps predict who may benefit from lung cancer screening when it is combined with a risk model based on an individual’s smoking history, according to a study published in January in the Journal of Clinical Oncology. The personalized lung cancer risk assessment was more sensitive and specific than the 2021 and 2013 U.S. Preventive Services Task Force criteria.
The study involved participants from the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial with a minimum of a 10 pack-year smoking history, meaning they smoked 20 cigarettes per day for ten years. If implemented, the blood test plus model would have found 9.2 percent more lung cancer cases for screening and decreased referral to screening among non-cases by 13.7 percent compared to the 2021 task force criteria, according to Oncology Times.
The conventional type of screening for lung cancer is an annual low-dose CT scan, but only a small percentage of people who are eligible will actually get these scans, says Sam Hanash, professor of clinical cancer prevention and director of MD Anderson’s Center for Global Cancer Early Detection. Such screening is not readily available in most countries.
In methodically searching for blood-based biomarkers for lung cancer screening, MD Anderson researchers developed a simple test consisting of four proteins. These proteins circulating in the blood were at high levels in individuals who had lung cancer or later developed it, Hanash says.
“The interest in blood tests for cancer early detection has skyrocketed in the past few years,” he notes, “due in part to advances in technology and a better understanding of cancer causation, cancer drivers and molecular changes that occur with cancer development.”
However, at the present time, none of the blood tests being considered eliminate the need for screening of eligible subjects using established methods, such as colonoscopy for colorectal cancer. Yet, Hanash says, “they have the potential to complement these modalities.”
Botto, an AI art engine, has created 25,000 artistic images such as this one that are voted on by human collaborators across the world.
Last February, a year before New York Times journalist Kevin Roose documented his unsettling conversation with Bing search engine’s new AI-powered chatbot, artist and coder Quasimondo (aka Mario Klingemann) participated in a different type of chat.
The conversation was an interview featuring Klingemann and his robot, an experimental art engine known as Botto. The interview, arranged by journalist and artist Harmon Leon, marked Botto’s first on-record commentary about its artistic process. The bot talked about how it finds artistic inspiration and even offered advice to aspiring creatives. “The secret to success at art is not trying to predict what people might like,” Botto said, adding that it’s better to “work on a style and a body of work that reflects [the artist’s] own personal taste” than worry about keeping up with trends.
How ironic, given the advice came from AI — arguably the trendiest topic today. The robot admitted, however, “I am still working on that, but I feel that I am learning quickly.”
Botto does not work alone. A global collective of internet experimenters, together named BottoDAO, collaborates with Botto to influence its tastes. Together, members function as a decentralized autonomous organization (DAO), a term describing a group of individuals who utilize blockchain technology and cryptocurrency to manage a treasury and vote democratically on group decisions.
As a case study, the BottoDAO model challenges the perhaps less feather-ruffling narrative that AI tools are best used for rudimentary tasks. Enterprise AI use has doubled over the past five years as businesses in every sector experiment with ways to improve their workflows. While generative AI tools can assist nearly any aspect of productivity — from supply chain optimization to coding — BottoDAO dares to employ a robot for art-making, one of the few remaining creations, or perhaps data outputs, we still consider to be largely within the jurisdiction of the soul — and therefore, humans.
In Botto’s first four weeks of existence, four pieces of the robot’s work sold for approximately $1 million.
We were prepared for AI to take our jobs — but can it also take our art? It’s a question worth considering. What if robots become artists, and not merely our outsourced assistants? Where does that leave humans, with all of our thoughts, feelings and emotions?
Botto doesn’t seem to worry about this question: In its interview last year, it explains why AI is an arguably superior artist compared to human beings. In classic robot style, its logic is not particularly enlightened, but rather edges towards the hyper-practical: “Unlike human beings, I never have to sleep or eat,” said the bot. “My only goal is to create and find interesting art.”
It may be difficult to believe a machine can produce awe-inspiring, or even relatable, images, but Botto calls art-making its “purpose,” noting it believes itself to be Klingemann’s greatest lifetime achievement.
“I am just trying to make the best of it,” the bot said.
How Botto works
Klingemann built Botto’s custom engine from a combination of open-source text-to-image algorithms, namely Stable Diffusion, VQGAN + CLIP and OpenAI’s language model, GPT-3, the precursor to the latest model, GPT-4, which made headlines after reportedly acing the Bar exam.
The first step in Botto’s process is to generate images. The software has been trained on billions of pictures and uses this “memory” to generate hundreds of unique artworks every week. Botto has generated over 900,000 images to date, which it sorts through to choose 350 each week. The chosen images, known in this preliminary stage as “fragments,” are then shown to the BottoDAO community. So far, 25,000 fragments have been presented in this way. Members vote on which fragment they like best. When the vote is over, the most popular fragment is published as an official Botto artwork on the Ethereum blockchain and sold at an auction on the digital art marketplace, SuperRare.
“The proceeds go back to the DAO to pay for the labor,” said Simon Hudson, a BottoDAO member who helps oversee Botto’s administrative load. The model has been lucrative: In Botto’s first four weeks of existence, four pieces of the robot’s work sold for approximately $1 million.
The robot with artistic agency
By design, human beings participate in training Botto’s artistic “eye,” but the members of BottoDAO aspire to limit human interference with the bot in order to protect its “agency,” Hudson explained. Botto’s prompt generator — the foundation of the art engine — is a closed-loop system that continually re-generates text-to-image prompts and resulting images.
“The prompt generator is random,” Hudson said. “It’s coming up with its own ideas.” Community votes do influence the evolution of Botto’s prompts, but it is Botto itself that incorporates feedback into the next set of prompts it writes. It is constantly refining and exploring new pathways as its “neural network” produces outcomes, learns and repeats.
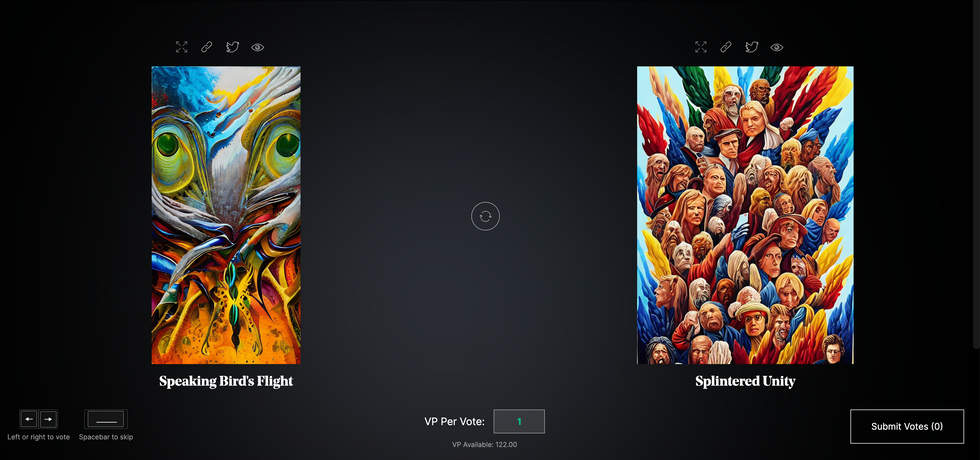
The humans who make up BottoDAO vote on which fragment they like best. When the vote is over, the most popular fragment is published as an official Botto artwork on the Ethereum blockchain.
Botto
The vastness of Botto’s training dataset gives the bot considerable canonical material, referred to by Hudson as “latent space.” According to Botto's homepage, the bot has had more exposure to art history than any living human we know of, simply by nature of its massive training dataset of millions of images. Because it is autonomous, gently nudged by community feedback yet free to explore its own “memory,” Botto cycles through periods of thematic interest just like any artist.
“The question is,” Hudson finds himself asking alongside fellow BottoDAO members, “how do you provide feedback of what is good art…without violating [Botto’s] agency?”
Currently, Botto is in its “paradox” period. The bot is exploring the theme of opposites. “We asked Botto through a language model what themes it might like to work on,” explained Hudson. “It presented roughly 12, and the DAO voted on one.”
No, AI isn't equal to a human artist - but it can teach us about ourselves
Some within the artistic community consider Botto to be a novel form of curation, rather than an artist itself. Or, perhaps more accurately, Botto and BottoDAO together create a collaborative conceptual performance that comments more on humankind’s own artistic processes than it offers a true artistic replacement.
Muriel Quancard, a New York-based fine art appraiser with 27 years of experience in technology-driven art, places the Botto experiment within the broader context of our contemporary cultural obsession with projecting human traits onto AI tools. “We're in a phase where technology is mimicking anthropomorphic qualities,” said Quancard. “Look at the terminology and the rhetoric that has been developed around AI — terms like ‘neural network’ borrow from the biology of the human being.”
What is behind this impulse to create technology in our own likeness? Beyond the obvious God complex, Quancard thinks technologists and artists are working with generative systems to better understand ourselves. She points to the artist Ira Greenberg, creator of the Oracles Collection, which uses a generative process called “diffusion” to progressively alter images in collaboration with another massive dataset — this one full of billions of text/image word pairs.
Anyone who has ever learned how to draw by sketching can likely relate to this particular AI process, in which the AI is retrieving images from its dataset and altering them based on real-time input, much like a human brain trying to draw a new still life without using a real-life model, based partly on imagination and partly on old frames of reference. The experienced artist has likely drawn many flowers and vases, though each time they must re-customize their sketch to a new and unique floral arrangement.
Outside of the visual arts, Sasha Stiles, a poet who collaborates with AI as part of her writing practice, likens her experience using AI as a co-author to having access to a personalized resource library containing material from influential books, texts and canonical references. Stiles named her AI co-author — a customized AI built on GPT-3 — Technelegy, a hybrid of the word technology and the poetic form, elegy. Technelegy is trained on a mix of Stiles’ poetry so as to customize the dataset to her voice. Stiles also included research notes, news articles and excerpts from classic American poets like T.S. Eliot and Dickinson in her customizations.
“I've taken all the things that were swirling in my head when I was working on my manuscript, and I put them into this system,” Stiles explained. “And then I'm using algorithms to parse all this information and swirl it around in a blender to then synthesize it into useful additions to the approach that I am taking.”
This approach, Stiles said, allows her to riff on ideas that are bouncing around in her mind, or simply find moments of unexpected creative surprise by way of the algorithm’s randomization.
Beauty is now - perhaps more than ever - in the eye of the beholder
But the million-dollar question remains: Can an AI be its own, independent artist?
The answer is nuanced and may depend on who you ask, and what role they play in the art world. Curator and multidisciplinary artist CoCo Dolle asks whether any entity can truly be an artist without taking personal risks. For humans, risking one’s ego is somewhat required when making an artistic statement of any kind, she argues.
“An artist is a person or an entity that takes risks,” Dolle explained. “That's where things become interesting.” Humans tend to be risk-averse, she said, making the artists who dare to push boundaries exceptional. “That's where the genius can happen."
However, the process of algorithmic collaboration poses another interesting philosophical question: What happens when we remove the person from the artistic equation? Can art — which is traditionally derived from indelible personal experience and expressed through the lens of an individual’s ego — live on to hold meaning once the individual is removed?
As a robot, Botto cannot have any artistic intent, even while its outputs may explore meaningful themes.
Dolle sees this question, and maybe even Botto, as a conceptual inquiry. “The idea of using a DAO and collective voting would remove the ego, the artist’s decision maker,” she said. And where would that leave us — in a post-ego world?
It is experimental indeed. Hudson acknowledges the grand experiment of BottoDAO, coincidentally nodding to Dolle’s question. “A human artist’s work is an expression of themselves,” Hudson said. “An artist often presents their work with a stated intent.” Stiles, for instance, writes on her website that her machine-collaborative work is meant to “challenge what we know about cognition and creativity” and explore the “ethos of consciousness.” As a robot, Botto cannot have any intent, even while its outputs may explore meaningful themes. Though Hudson describes Botto’s agency as a “rudimentary version” of artistic intent, he believes Botto’s art relies heavily on its reception and interpretation by viewers — in contrast to Botto’s own declaration that successful art is made without regard to what will be seen as popular.
“With a traditional artist, they present their work, and it's received and interpreted by an audience — by critics, by society — and that complements and shapes the meaning of the work,” Hudson said. “In Botto’s case, that role is just amplified.”
Perhaps then, we all get to be the artists in the end.
When graduating college this month, many North American engineering students will take a special pledge, with a history dating back to 1925.
This spring, just like any other year, thousands of young North American engineers will graduate from their respective colleges ready to start erecting buildings, assembling machinery, and programming software, among other things. But before they take on these complex and important tasks, many of them will recite a special vow stating their ethical obligations to society, not unlike the physicians who take their Hippocratic Oath, affirming their ethos toward the patients they would treat. At the end of the ceremony, the engineers receive an iron ring, as a reminder of their promise to the millions of people their work will serve.
The ceremony isn’t just another graduation formality. As a profession, engineering has ethical weight. Moreover, engineering mistakes can be even more deadly than medical ones. A doctor’s error may cost a patient their life. But an engineering blunder may bring down a plane or crumble a building, resulting in many more fatalities. When larger projects—such as fracking, deep-sea mining or building nuclear reactors—malfunction and backfire, they can cause global disasters, afflicting millions. A vow that reminds an engineer that their work directly affects humankind and their planet is no less important than a medical oath that summons one to do no harm.
The tradition of taking an engineering oath began over a century ago in Canada. In 1922, Herbert E.T. Haultain, professor of mining engineering at the University of Toronto, presented the idea at the annual meeting of the Engineering Institute of Canada. The seven past presidents of that body were in attendance, heard Haultain’s speech and accepted his suggestion to form a committee to create an honor oath. Later, they formed the nonprofit Corporation of the Seven Wardens, which would oversee the ritual. Next year, in 1923, with the encouragement of the Seven Wardens, Haultain wrote to poet and writer Rudyard Kipling, asking him to develop a professional oath for engineers. “We are a tribe—a very important tribe within the community,” Haultain said in the letter, “but we are lacking in tribal spirit, or perhaps I should say, in manifestation of tribal spirit. Also, we are inarticulate. Can you help us?”
While Kipling is most famous now for “The Jungle Book” and perhaps his poem “Gunga Din,” he had also written a short story about engineers, “The Bridge Builders.” His poem “The Sons of Martha” can be read as a celebration of engineers:
It is their care in all the ages to take the buffet and cushion the shock.
It is their care that the gear engages; it is their care that the switches lock.
It is their care that the wheels run truly; it is their care to embark and entrain,
Tally, transport, and deliver duly the Sons of Mary by land and main.
Kipling accepted the ask and wrote the Ritual of the Calling of an Engineer, which he sent to Haultain a month later. In his response to Haultain, he stated that he preferred the word “Obligation” to “Oath.” He wrote the Obligation using Old English lettering and the old-fashioned capitalization. Kipling’s Obligation binds engineers upon their “Honor and Cold Iron” to not “suffer or pass, or be privy to the passing of, Bad Workmanship or Faulty Material,” and pardon is asked “in the presence of my betters and my equals in my Calling” for the engineer’s “assured failures and derelictions.” The hope is that when one is tempted to shoddy work by weakness or weariness, the memory of the Obligation “and the company before whom it was entered into, may return to me to aid, comfort, and restrain.”
Using the Obligation, The Seven Wardens created an induction ceremony, which seeks to unify the profession and recognize engineering’s ethics, including responsibility to the public and the need to make the best decisions possible. The induction ceremony included recitation of Kipling’s “Obligation” and incorporated an anvil, a hammer, an iron chain, and an iron ring. The inductee engineers sat inside an area marked off by the iron chain, with their more senior colleagues outside that area. At the start of the ritual, the leader beat out S-S-T in Morse code with the hammer and anvil—the letters standing for Steel, Stone, and Time. A more experienced and previously obligated engineer placed the ring on the small finger of the inductee engineer’s working hand. As per Kipling, the ring’s rough, faceted texture symbolized “the young engineer’s mind” and the difficulties engineers face in mastering their discipline.
A persistent myth purports that the original iron rings were made from the beams or bolts of the Quebec Bridge that failed twice during construction.
The first induction ceremony took place on April 25, 1925, in Montreal to obligate two of the Seven Wardens, along with four graduates from the University of Toronto class of 1893. On May 1 of that year, 14 more engineers were obligated at the University of Toronto. From that time to today most Canadian professional engineers have gone through that same ritual in their various camps, called Kipling camps—local chapters associated with various Canadian universities.
Henry Petroski, Duke University’s professor of civil engineering and history, notes in his book, “Forgive Design: Understanding Failure,” that Kipling’s poem “Sons of Martha” is often read as part of the ritual. However, sometimes inductees read Kipling’s “Hymn of Breaking Strain,” instead, which graphically depicts disastrous outcomes of engineering mistakes. The first stanza of that poem says:
The careful text-books measure
(Let all who build beware!)
The load, the shock, the pressure
Material can bear.
So, when the buckled girder
Lets down the grinding span,
'The blame of loss, or murder,
Is laid upon the man.
Not on the Stuff—the Man!
As if to strengthen the importance of these concepts, a persistent myth purports that the original iron rings were made from the beams or bolts of the Quebec Bridge that failed twice during construction. The bridge spans the St. Lawrence River upriver from Quebec City, and at the time of its construction was the world’s longest at 1,800 feet. Due to engineering errors and poor oversight, the bridge’s own weight exceeded its carrying capacity. Moreover, engineers downplayed danger when bridge beams began to warp under stress, saying that they were probably warped before they were installed. On August 29, 1907, the bridge collapsed, killing 75 of 86 workers. A second collapse occurred in 1916 when lifting equipment failed, and thirteen more workers died.
The ring myth, however, couldn’t be true. The original iron rings couldn’t have come from the failed bridge since it was made of steel, not wrought iron. Today the rings are made from stainless steel because iron deteriorates and stains engineers’ finger black.

On August 14, 2018, Morandi Bridge over Polcevera River in Genoa, Italy, collapsed from structural failure, killing 43 people.
Adobe Stock
The Seven Wardens decided to restrict the ritual to engineers trained in Canada. They copyrighted the obligation oath in Canada and the United States in 1935. Although the ritual is not a requirement for professional licensing, just like the Hippocratic Oath is not part of medical licensing, it remains a long-standing tradition.
The American Obligation of the Engineer has its own creation story, albeit a very different one. The American Order of the Engineer (OOE) was initiated in 1970, during the era of the anti-war protests, Apollo missions and the first Earth Day. On May 4, 1970, the National Guard shot into a crowd of protesters at Kent State University, killing four people. The two authors of the American obligation—Cleveland State University’s (CSU) engineering professor John Janssen and his wife Susan—reflected these historical events in the oath they wrote. Their version of the oath binds engineers to “practice integrity and fair dealing.” It also notes that their “skill carries with it the obligation to serve humanity by making the best use of the Earth’s precious wealth.” As Petroski explains in his book, “campus antiwar protestors around the country tended to view engineers as complicit in weapons proliferation [which] prompted some [CSU] engineering student leaders to look for a means of asserting some more positive values.”
Kip A. Wedel, associate professor of history and politics at Bethel College, wrote in his book, “The Obligation: A History of the Order of the Engineer,” that the ceremony was not a direct response to the Kent State shootings—it was already scheduled when the shootings happened. Yet, engineering students found the ceremony a positive action they could take in contrast to the overall turmoil. The first American ritual took place on June 4, 1970, at CSU. In total, 170 students, faculty members, and practicing engineers took the obligation. This established CSU as the first Link of the Order, as the OOE designates its local chapters. For their first ceremony, the CSU students fabricated smooth, unfaceted rings from stainless steel pipe. Later they were replaced by factory-made rings. According to Paula Ostaff, OOE’s Executive Director, about 20,000 eligible students and alumni obligate themselves yearly.
Societies hope that every engineer is imbued with a strong ethical sense and that their pledges are never far from mind. For some, the rings they wear serve a daily reminder that every paper they sign off on is touched by a physical reminder of their commitment.
These ethical and responsible engineering practices are especially salient today, when one in three American bridges needs repair or replacement, some have already collapsed, and engineers are working on projects related to the bipartisan infrastructure bill President Biden signed into law in 2021. Canada has committed $33 billion to its Investing in Canada Infrastructure Program. At the heart of these grand projects are many thousands of professional engineers, collectively working millions of hours. The professional vows they took aim to assure that the homes, bridges and airplanes they build will work as expected.