Life is Emerging: Review of Siddhartha Mukherjee’s Song of the Cell
A new book by Pulitzer-winning physician-scientist Siddhartha Mukherjee will be released from Simon & Schuster on October 25, 2022.
The DNA double helix is often the image spiraling at the center of 21st century advances in biomedicine and the growing bioeconomy. And yet, DNA is molecularly inert. DNA, the code for genes, is not alive and is not strictly necessary for life. Ought life be at the center of our communication of living systems? Is not the Cell a superior symbol of life and our manipulation of living systems?
A code for life isn’t a code without the life that instantiates it. A code for life must be translated. The cell is the basic unit of that translation. The cell is the minimal viable package of life as we know it. Therefore, cell biology is at the center of biomedicine’s greatest transformations, suggests Pulitzer-winning physician-scientist Siddhartha Mukherjee in his latest book, The Song of the Cell: The Exploration of Medicine and the New Human.
The Song of the Cell begins with the discovery of cells and of germ theory, featuring characters such as Louis Pasteur and Robert Koch, who brought the cell “into intimate contact with pathology and medicine.” This intercourse would transform biomedicine, leading to the insight that we can treat disease by thinking at the cellular level. The slightest rearrangement of sick cells might be the path toward alleviating suffering for the organism: eroding the cell walls of a bacterium while sparing our human cells; inventing a medium that coaxes sperm and egg to dance into cellular union for in vitro fertilization (IVF); designing molecular missiles that home to the receptors decorating the exterior of cancer cells; teaching adult skin cells to remember their embryonic state for regenerative medicines.
Mukherjee uses the bulk of the book to elucidate key cell types in the human body, along with their “connective relationships” that enable key organs and organ systems to function. This includes the immune system, the heart, the brain, and so on. Mukherjee’s distinctive style features compelling anecdotes and human stories that animate the scientific (and unscientific) processes that have led to our current state of understanding. In his chapter on neurons and the brain, for example, he integrates Santiago Ramon y Cajal’s meticulous black ink sketches of neurons into Mukherjee’s own personal encounter with clinical depression. In one lucid section, he interviews Dr. Helen Mayberg, a pioneering neurologist who takes seriously the descriptive power of her patients’ metaphors, as they suffer from “caves,” “holes,” “voids,” and “force fields” that render their lives gray. Dr. Mayberg aims to stimulate patients’ neuronal cells in a manner that brings back the color.
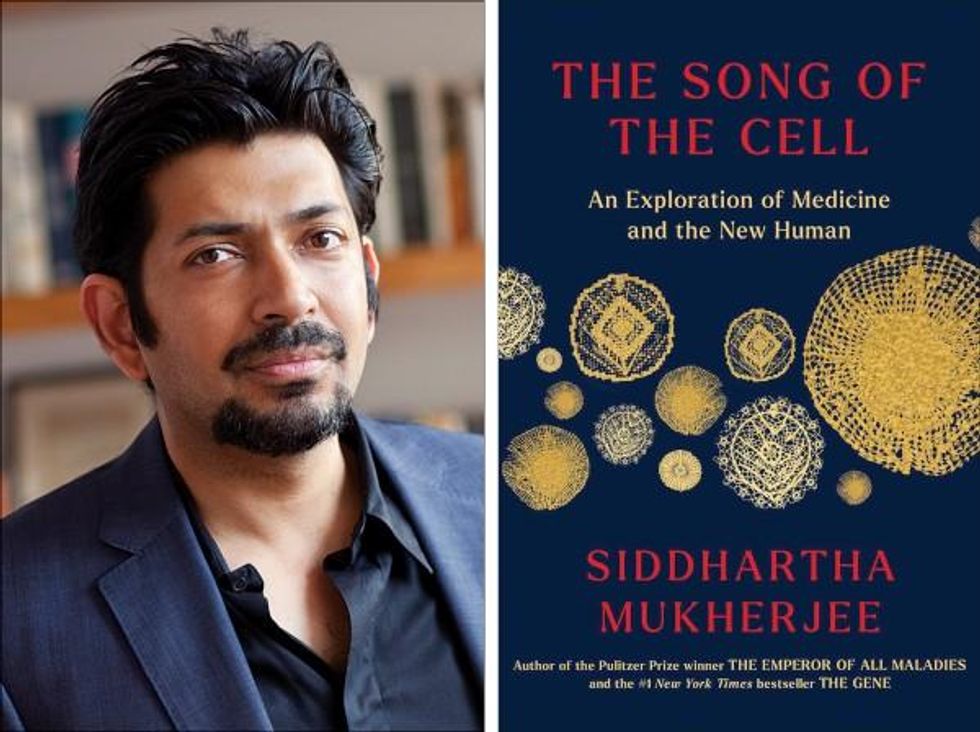
Beyond exposing the insight and inventiveness that has arisen out of cell-based thinking, it seems that Mukherjee’s bigger project is an epistemological one. The early chapters of The Song of the Cell continually hint at the potential for redefining the basic unit of biology as the cell rather than the gene. The choice to center biomedicine around cells is, above all, a conspicuous choice not to center it around genes (the subject of Mukherjee’s previous book, The Gene), because genes dominate popular science communication.
This choice of cells over genes is most welcome. Cells are alive. Genes are not. Letters—such as the As, Cs, Gs, and Ts that represent the nucleotides of DNA, which make up our genes—must be synthesized into a word or poem or song that offers a glimpse into deeper truths. A key idea embedded in this thinking is that of emergence. Whether in ancient myth or modern art, creation tends to be an emergent process, not a linearly coded script. The cell is our current best guess for the basic unit of life’s emergence, turning a finite set of chemical building blocks—nucleic acids, proteins, sugars, fats—into a replicative, evolving system for fighting stasis and entropy. The cell’s song is one for our times, for it is the song of biology’s emergence out of chemistry and physics, into the “frenetically active process” of homeostasis.
Re-centering our view of biology has practical consequences, too, for how we think about diagnosing and treating disease, and for inventing new medicines. Centering cells presents a challenge: which type of cell to place at the center? Rather than default to the apparent simplicity of DNA as a symbol because it represents the one master code for life, the tension in defining the diversity of cells—a mapping process still far from complete in cutting-edge biology laboratories—can help to create a more thoughtful library of cellular metaphors to shape both the practice and communication of biology.
Further, effective problem solving is often about operating at the right level, or the right scale. The cell feels like appropriate level at which to interrogate many of the diseases that ail us, because the senses that guide our own perceptions of sickness and health—the smoldering pain of inflammation, the tunnel vision of a migraine, the dizziness of a fluttering heart—are emergent.
This, unfortunately, is sort of where Mukherjee leaves the reader, under-exploring the consequences of a biology of emergence. Many practical and profound questions have to do with the ways that each scale of life feeds back on the others. In a tome on Cells and “the future human” I wished that Mukherjee had created more space for seeking the ways that cells will shape and be shaped by the future, of humanity and otherwise.
We are entering a phase of real-world bioengineering that features the modularization of cellular parts within cells, of cells within organs, of organs within bodies, and of bodies within ecosystems. In this reality, we would be unwise to assume that any whole is the mere sum of its parts.
For example, when discussing the regenerative power of pluripotent stem cells, Mukherjee raises the philosophical thought experiment of the Delphic boat, also known as the Ship of Theseus. The boat is made of many pieces of wood, each of which is replaced for repairs over the years, with the boat’s structure unchanged. Eventually none of the boat’s original wood remains: Is it the same boat?
Mukherjee raises the Delphic boat in one paragraph at the end of the chapter on stem cells, as a metaphor related to the possibility of stem cell-enabled regeneration in perpetuity. He does not follow any of the threads of potential answers. Given the current state of cellular engineering, about which Mukherjee is a world expert from his work as a physician-scientist, this book could have used an entire section dedicated to probing this question and, importantly, the ways this thought experiment falls apart.
We are entering a phase of real-world bioengineering that features the modularization of cellular parts within cells, of cells within organs, of organs within bodies, and of bodies within ecosystems. In this reality, we would be unwise to assume that any whole is the mere sum of its parts. Wholeness at any one of these scales of life—organelle, cell, organ, body, ecosystem—is what is at stake if we allow biological reductionism to assume away the relation between those scales.
In other words, Mukherjee succeeds in providing a masterful and compelling narrative of the lives of many of the cells that emerge to enliven us. Like his previous books, it is a worthwhile read for anyone curious about the role of cells in disease and in health. And yet, he fails to offer the broader context of The Song of the Cell.
As leading agronomist and essayist Wes Jackson has written, “The sequence of amino acids that is at home in the human cell, when produced inside the bacterial cell, does not fold quite right. Something about the E. coli internal environment affects the tertiary structure of the protein and makes it inactive. The whole in this case, the E. coli cell, affects the part—the newly made protein. Where is the priority of part now?” [1]
Beyond the ways that different kingdoms of life translate the same genetic code, the practical situation for humanity today relates to the ways that the different disciplines of modern life use values and culture to influence our genes, cells, bodies, and environment. It may be that humans will soon become a bit like the Delphic boat, infused with the buzz of fresh cells to repopulate different niches within our bodies, for healthier, longer lives. But in biology, as in writing, a mixed metaphor can cause something of a cacophony. For we are not boats with parts to be replaced piecemeal. And nor are whales, nor alpine forests, nor topsoil. Life isn’t a sum of parts, and neither is a song that rings true.
[1] Wes Jackson, "Visions and Assumptions," in Nature as Measure (p. 52-53).
The First Mass-Produced Solar Car Is Coming Soon, Sparking Excitement and Uncertainty
Reporter Michaela Haas takes Aptera's Sol car out for a test drive in San Diego, Calif.
The white two-seater car that rolls down the street in the Sorrento Valley of San Diego looks like a futuristic batmobile, with its long aerodynamic tail and curved underbelly. Called 'Sol' (Spanish for "sun"), it runs solely on solar and could be the future of green cars. Its maker, the California startup Aptera, has announced the production of Sol, the world's first mass-produced solar vehicle, by the end of this year. Aptera co-founder Chris Anthony points to the sky as he says, "On this sunny California day, there is ample fuel. You never need to charge the car."
If you live in a sunny state like California or Florida, you might never need to plug in the streamlined Sol because the solar panels recharge while driving and parked. Its 60-mile range is more than the average commuter needs. For cloudy weather, battery packs can be recharged electronically for a range of up to 1,000 miles. The ultra-aerodynamic shape made of lightweight materials such as carbon, Kevlar, and hemp makes the Sol four times more energy-efficient than a Tesla, according to Aptera. "The material is seven times stronger than steel and even survives hail or an angry ex-girlfriend," Anthony promises.
Co-founder Steve Fambro opens the Sol's white doors that fly upwards like wings and I get inside for a test drive. Two dozen square solar panels, each the size of a large square coaster, on the roof, front, and tail power the car. The white interior is spartan; monitors have replaced mirrors and the dashboard. An engineer sits in the driver's seat, hits the pedal, and the low-drag two-seater zooms from 0 to 60 in 3.5 seconds.
It feels like sitting in a race car because the two-seater is so low to the ground but the car is built to go no faster than 100 or 110 mph. The finished car will weigh less than 1,800 pounds, about half of the smallest Tesla. The average car, by comparison, weighs more than double that. "We've built it primarily for energy efficiency," Steve Fambro says, explaining why the Sol has only three wheels. It's technically an "auto-cycle," a hybrid between a motorcycle and a car, but Aptera's designers are also working to design a four-seater.
There has never been a lack of grand visions for the future of the automobile, but until these solar cars actually hit the streets, nobody knows how the promises will hold up.
Transportation is currently the biggest source of greenhouse gases. Developing an efficient solar car that does not burden the grid has been the dream of innovators for decades. Every other year, dozens of innovators race their self-built solar cars 2,000 miles through the Australian desert.
More effective solar panels are finally making the dream mass-compatible, but just like other innovative car ideas, Aptera's vision has been plagued with money problems. Anthony and Fambro were part of the original crew that founded Aptera in 2006 and worked on the first prototype around the same time Tesla built its first roadster, but Aptera went bankrupt in 2011. Anthony and Fambro left a year before the bankruptcy and went on to start other companies. Among other projects, Fambro developed the first USDA organic vertical farm in the United Arab Emirates, and Anthony built a lithium battery company, before the two decided to buy Aptera back. Without a billionaire such as Elon Musk bankrolling the risky process of establishing a whole new car production system from scratch, the huge production costs are almost insurmountable.
But Aptera's founders believe they have found solutions for the entire production process as well as the car design. Most parts of the Sol's body can be made by 3D printers and assembled like a Lego kit. If this makes you think of a toy car, Anthony assures potential buyers that the car aced stress tests and claims it's safer than any vehicle on the market, "because the interior is shaped like an egg and if there is an impact, the pressure gets distributed equally." However, Aptera has yet to release crash test safety data so outside experts cannot evaluate their claims.
Instead of building a huge production facility, Anthony and Fambro envision "micro-factories," each less than 10,000 square feet, where a small crew can assemble cars on demand wherever the orders are highest, be it in California, Canada, or China.
If a part of the Sol breaks, Aptera promises to send replacement parts to any corner of the world within 24 hours, with instructions. So a mechanic in a rural corner in Arkansas or China who never worked on a solar car before simply needs to download the instructions and replace the broken part. At least that's the idea. "The material does not rust nor fatigue," Fambro promises. "You can pass the car onto your grandchildren. When more efficient solar panels hit the market, we simply replace them."
More than 11,000 potential buyers have already signed up; the cheapest model costs around $26,000 USD and Aptera expects the first cars to ship by the end of the year.
Two other solar carmakers are vying for the pole position in the race to be the first to market: The German startup Sono has also announced it will also produce its first solar car by the end of this year. The price tag for the basic model is also around $26,000, but its concept is very different. From the outside, the Sion looks like a conservative minivan for a family; only a closer look reveals that the dark exterior is made of solar panels. Sono, too, nearly went bankrupt a few years ago and was saved through a crowdfunding campaign by enthusiastic fans.
Meanwhile, Norwegian company Lightyear wants to produce a sleek solar-powered luxury sedan by the end of the year, but its price of around $180,000 makes it unaffordable for most buyers.
There has never been a lack of grand visions for the future of the automobile, but until these solar cars actually hit the streets, nobody knows how the promises will hold up. How often will the cars need to be repaired? What happens when snow and ice cover the solar panels? Also, you can't park the car in a garage if you need the sun to charge it.
Critics, including students at the Solar Car team at the University of Michigan, say that mounting solar panels on a moving vehicle will never yield the most efficient results compared to static panels. Also, they are quick to point out that no company has managed to overcome the production hurdles yet. Others in the field also wonder how well the solar panels will actually work.
"It's important to realize that the solar mileage claims by these companies are likely the theoretical best case scenario but in the real world, solar range will be significantly less when you factor in shading, parking in garages, and geographies with lower solar irradiance," says Evan Stumpges, the team coordinator for the American Solar Challenge, a competition in which enthusiasts build and race solar-powered cars. "The encouraging thing is that I have seen videos of real working prototypes for each of these vehicles which is a key accomplishment. That said, I believe the biggest hurdle these companies have yet to face is successfully ramping up to volume production and understanding what their profitability point will be for selling the vehicles once production has stabilized."
Professor Daniel M. Kammen, the founding director of the Renewable and Appropriate Energy Laboratory at the University of California, Berkeley, and one of the world's foremost experts on renewable energy, believes that the technical challenges have been solved, and that solar cars have real advantages over electric vehicles.
"This is the right time to be bullish. Cutting out the charging is a natural solution for long rides," he says. "These vehicles are essentially solar panels and batteries on wheels. These are now record low-cost and can be built from sustainable materials." Apart from Aptera's no-charge technology, he appreciates the move toward no-conflict materials. "Not only is the time ripe but the youth movement is pushing toward conflict-free material and reducing resource waste....A low-cost solar fleet could be really interesting in relieving burden on the grid, or you could easily imagine a city buying a bunch of them and connecting them with mass transit." While he has followed all three new solar companies with interest, he has already ordered an Aptera car for himself, "because it's American and it looks the most different."
After taking a spin in the Sol, it is startling to switch back into a regular four-seater. Rolling out of Aptera's parking lot onto the freeway next to all the oversized gas guzzlers that need to stop every couple of hundreds of miles to fill up, one can't help but think: We've just taken a trip into the future.
Biohackers Made a Cheap and Effective Home Covid Test -- But No One Is Allowed to Use It
A stock image of a home test for COVID-19.
Last summer, when fast and cheap Covid tests were in high demand and governments were struggling to manufacture and distribute them, a group of independent scientists working together had a bit of a breakthrough.
Working on the Just One Giant Lab platform, an online community that serves as a kind of clearing house for open science researchers to find each other and work together, they managed to create a simple, one-hour Covid test that anyone could take at home with just a cup of hot water. The group tested it across a network of home and professional laboratories before being listed as a semi-finalist team for the XPrize, a competition that rewards innovative solutions-based projects. Then, the group hit a wall: they couldn't commercialize the test.
They wanted to keep their project open source, making it accessible to people around the world, so they decided to forgo traditional means of intellectual property protection and didn't seek patents. (They couldn't afford lawyers anyway). And, as a loose-knit group that was not supported by a traditional scientific institution, working in community labs and homes around the world, they had no access to resources or financial support for manufacturing or distributing their test at scale.
But without ethical and regulatory approval for clinical testing, manufacture, and distribution, they were legally unable to create field tests for real people, leaving their inexpensive, $16-per-test, innovative product languishing behind, while other, more expensive over-the-counter tests made their way onto the market.
Who Are These Radical Scientists?
Independent, decentralized biomedical research has come of age. Also sometimes called DIYbio, biohacking, or community biology, depending on whom you ask, open research is today a global movement with thousands of members, from scientists with advanced degrees to middle-grade students. Their motivations and interests vary across a wide spectrum, but transparency and accessibility are key to the ethos of the movement. Teams are agile, focused on shoestring-budget R&D, and aim to disrupt business as usual in the ivory towers of the scientific establishment.
Ethics oversight is critical to ensuring that research is conducted responsibly, even by biohackers.
Initiatives developed within the community, such as Open Insulin, which hopes to engineer processes for affordable, small-batch insulin production, "Slybera," a provocative attempt to reverse engineer a $1 million dollar gene therapy, and the hundreds of projects posted on the collaboration platform Just One Giant Lab during the pandemic, all have one thing in common: to pursue testing in humans, they need an ethics oversight mechanism.
These groups, most of which operate collaboratively in community labs, homes, and online, recognize that some sort of oversight or guidance is useful—and that it's the right thing to do.
But also, and perhaps more immediately, they need it because federal rules require ethics oversight of any biomedical research that's headed in the direction of the consumer market. In addition, some individuals engaged in this work do want to publish their research in traditional scientific journals, which—you guessed it—also require that research has undergone an ethics evaluation. Ethics oversight is critical to ensuring that research is conducted responsibly, even by biohackers.
Bridging the Ethics Gap
The problem is that traditional oversight mechanisms, such as institutional review boards at government or academic research institutions, as well as the private boards utilized by pharmaceutical companies, are not accessible to most independent researchers. Traditional review boards are either closed to the public, or charge fees that are out of reach for many citizen science initiatives. This has created an "ethics gap" in nontraditional scientific research.
Biohackers are seen in some ways as the direct descendents of "white hat" computer hackers, or those focused on calling out security holes and contributing solutions to technical problems within self-regulating communities. In the case of health and biotechnology, those problems include both the absence of treatments and the availability of only expensive treatments for certain conditions. As the DIYbio community grows, there needs to be a way to provide assurance that, when the work is successful, the public is able to benefit from it eventually. The team that developed the one-hour Covid test found a potential commercial partner and so might well overcome the oversight hurdle, but it's been 14 months since they developed the test--and counting.
In short, without some kind of oversight mechanism for the work of independent biomedical researchers, the solutions they innovate will never have the opportunity to reach consumers.
In a new paper in the journal Citizen Science: Theory & Practice, we consider the issue of the ethics gap and ask whether ethics oversight is something nontraditional researchers want, and if so, what forms it might take. Given that individuals within these communities sometimes vehemently disagree with each other, is consensus on these questions even possible?
We learned that there is no "one size fits all" solution for ethics oversight of nontraditional research. Rather, the appropriateness of any oversight model will depend on each initiative's objectives, needs, risks, and constraints.
We also learned that nontraditional researchers are generally willing (and in some cases eager) to engage with traditional scientific, legal, and bioethics experts on ethics, safety, and related questions.
We suggest that these experts make themselves available to help nontraditional researchers build infrastructure for ethics self-governance and identify when it might be necessary to seek outside assistance.
Independent biomedical research has promise, but like any emerging science, it poses novel ethical questions and challenges. Existing research ethics and oversight frameworks may not be well-suited to answer them in every context, so we need to think outside the box about what we can create for the future. That process should begin by talking to independent biomedical researchers about their activities, priorities, and concerns with an eye to understanding how best to support them.
Christi Guerrini, JD, MPH studies biomedical citizen science and is an Associate Professor at Baylor College of Medicine. Alex Pearlman, MA, is a science journalist and bioethicist who writes about emerging issues in biotechnology. They have recently launched outlawbio.org, a place for discussion about nontraditional research.

