Coronavirus Risk Calculators: What You Need to Know
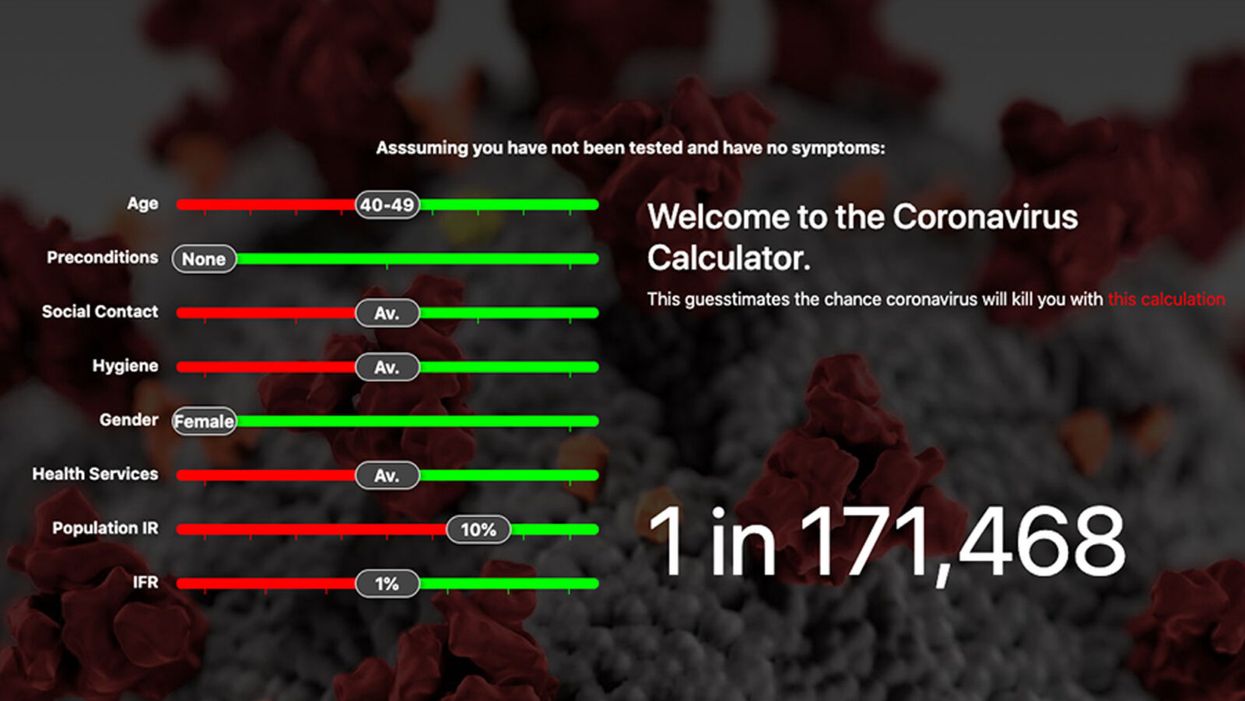
A screenshot of one coronavirus risk calculator.
People in my family seem to develop every ailment in the world, including feline distemper and Dutch elm disease, so I naturally put fingers to keyboard when I discovered that COVID-19 risk calculators now exist.
"It's best to look at your risk band. This will give you a more useful insight into your personal risk."
But the results – based on my answers to questions -- are bewildering.
A British risk calculator developed by the Nexoid software company declared I have a 5 percent, or 1 in 20, chance of developing COVID-19 and less than 1 percent risk of dying if I get it. Um, great, I think? Meanwhile, 19 and Me, a risk calculator created by data scientists, says my risk of infection is 0.01 percent per week, or 1 in 10,000, and it gave me a risk score of 44 out of 100.
Confused? Join the club. But it's actually possible to interpret numbers like these and put them to use. Here are five tips about using coronavirus risk calculators:
1. Make Sure the Calculator Is Designed For You
Not every COVID-19 risk calculator is designed to be used by the general public. Cleveland Clinic's risk calculator, for example, is only a tool for medical professionals, not sick people or the "worried well," said Dr. Lara Jehi, Cleveland Clinic's chief research information officer.
Unfortunately, the risk calculator's web page fails to explicitly identify its target audience. But there are hints that it's not for lay people such as its references to "platelets" and "chlorides."
The 19 and Me or the Nexoid risk calculators, in contrast, are both designed for use by everyone, as is a risk calculator developed by Emory University.
2. Take a Look at the Calculator's Privacy Policy
COVID-19 risk calculators ask for a lot of personal information. The Nexoid calculator, for example, wanted to know my age, weight, drug and alcohol history, pre-existing conditions, blood type and more. It even asked me about the prescription drugs I take.
It's wise to check the privacy policy and be cautious about providing an email address or other personal information. Nexoid's policy says it provides the information it gathers to researchers but it doesn't release IP addresses, which can reveal your location in certain circumstances.
John-Arne Skolbekken, a professor and risk specialist at Norwegian University of Science and Technology, entered his own data in the Nexoid calculator after being contacted by LeapsMag for comment. He noted that the calculator, among other things, asks for information about use of recreational drugs that could be illegal in some places. "I have given away some of my personal data to a company that I can hope will not misuse them," he said. "Let's hope they are trustworthy."
The 19 and Me calculator, by contrast, doesn't gather any data from users, said Cindy Hu, data scientist at Mathematica, which created it. "As soon as the window is closed, that data is gone and not captured."
The Emory University risk calculator, meanwhile, has a long privacy policy that states "the information we collect during your assessment will not be correlated with contact information if you provide it." However, it says personal information can be shared with third parties.
3. Keep an Eye on Time Horizons
Let's say a risk calculator says you have a 1 percent risk of infection. That's fairly low if we're talking about this year as a whole, but it's quite worrisome if the risk percentage refers to today and jumps by 1 percent each day going forward. That's why it's helpful to know exactly what the numbers mean in terms of time.
Unfortunately, this information isn't always readily available. You may have to dig around for it or contact a risk calculator's developers for more information. The 19 and Me calculator's risk percentages refer to this current week based on your behavior this week, Hu said. The Nexoid calculator, by contrast, has an "infinite timeline" that assumes no vaccine is developed, said Jonathon Grantham, the company's managing director. But your results will vary over time since the calculator's developers adjust it to reflect new data.
When you use a risk calculator, focus on this question: "How does your risk compare to the risk of an 'average' person?"
4. Focus on the Big Picture
The Nexoid calculator gave me numbers of 5 percent (getting COVID-19) and 99.309 percent (surviving it). It even provided betting odds for gambling types: The odds are in favor of me not getting infected (19-to-1) and not dying if I get infected (144-to-1).
However, Grantham told me that these numbers "are not the whole story." Instead, he said, "it's best to look at your risk band. This will give you a more useful insight into your personal risk." Risk bands refer to a segmentation of people into five categories, from lowest to highest risk, according to how a person's result sits relative to the whole dataset.
The Nexoid calculator says I'm in the "lowest risk band" for getting COVID-19, and a "high risk band" for dying of it if I get it. That suggests I'd better stay in the lowest-risk category because my pre-existing risk factors could spell trouble for my survival if I get infected.
Michael J. Pencina, a professor and biostatistician at Duke University School of Medicine, agreed that focusing on your general risk level is better than focusing on numbers. When you use a risk calculator, he said, focus on this question: "How does your risk compare to the risk of an 'average' person?"
The 19 and Me calculator, meanwhile, put my risk at 44 out of 100. Hu said that a score of 50 represents the typical person's risk of developing serious consequences from another disease – the flu.
5. Remember to Take Action
Hu, who helped develop the 19 and Me risk calculator, said it's best to use it to "understand the relative impact of different behaviors." As she noted, the calculator is designed to allow users to plug in different answers about their behavior and immediately see how their risk levels change.
This information can help us figure out if we should change the way we approach the world by, say, washing our hands more or avoiding more personal encounters.
"Estimation of risk is only one part of prevention," Pencina said. "The other is risk factors and our ability to reduce them." In other words, odds, percentages and risk bands can be revealing, but it's what we do to change them that matters.
Smartwatches can track COVID-19 symptoms, study finds
University of Michigan researchers found that new signals embedded in heart rate indicated when individuals were infected with COVID-19 and how ill they became.
If a COVID-19 infection develops, a wearable device may eventually be able to clue you in. A study at the University of Michigan found that a smartwatch can monitor how symptoms progress.
The study evaluated the effects of COVID-19 with various factors derived from heart-rate data. This method also could be employed to detect other diseases, such as influenza and the common cold, at home or when medical resources are limited, such as during a pandemic or in developing countries.
Tracking students and medical interns across the country, the University of Michigan researchers found that new signals embedded in heart rate indicated when individuals were infected with COVID-19 and how ill they became.
For instance, they discovered that individuals with COVID-19 experienced an increase in heart rate per step after the onset of their symptoms. Meanwhile, people who reported a cough as one of their COVID-19 symptoms had a much more elevated heart rate per step than those without a cough.
“We previously developed a variety of algorithms to analyze data from wearable devices. So, when the COVID-19 pandemic hit, it was only natural to apply some of these algorithms to see if we can get a better understanding of disease progression,” says Caleb Mayer, a doctoral student in mathematics at the University of Michigan and a co-first author of the study.
People may not internally sense COVID-19’s direct impact on the heart, but “heart rate is a vital sign that gives a picture of overall health," says Daniel Forger, a University of Michigan professor.
Millions of people are tracking their heart rate through wearable devices. This information is already generating a tremendous amount of data for researchers to analyze, says co-author Daniel Forger, professor of mathematics and research professor of computational medicine and bioinformatics at the University of Michigan.
“Heart rate is affected by many different physiological signals,” Forger explains. “For instance, if your lungs aren’t functioning properly, your heart may need to beat faster to meet metabolic demands. Your heart rate has a natural daily rhythm governed by internal biological clocks.” While people may not internally sense COVID-19’s direct impact on the heart, he adds that “heart rate is a vital sign that gives a picture of overall health.”
Among the total of 2,164 participants who enrolled in the student study, 72 undergraduate and graduate students contracted COVID-19, providing wearable data from 50 days before symptom onset to 14 days after. The researchers also analyzed this type of data for 43 medical interns from the Intern Health Study by the Michigan Neuroscience Institute and 29 individuals (who are not affiliated with the university) from the publicly available dataset.
Participants could wear the device on either wrist. They also documented their COVID-19 symptoms, such as fever, shortness of breath, cough, runny nose, vomiting, diarrhea, body aches, loss of taste, loss of smell, and sore throat.
Experts not involved in the study found the research to be productive. “This work is pioneering and reveals exciting new insights into the many important ways that we can derive clinically significant information about disease progression from consumer-grade wearable devices,” says Lisa A. Marsch, director of the Center for Technology and Behavioral Health and a professor in the Geisel School of Medicine at Dartmouth College. “Heart-rate data are among the highest-quality data that can be obtained via wearables.”
Beyond the heart, she adds, “Wearable devices are providing novel insights into individuals’ physiology and behavior in many health domains.” In particular, “this study beautifully illustrates how digital-health methodologies can markedly enhance our understanding of differences in individuals’ experience with disease and health.”
Previous studies had demonstrated that COVID-19 affects cardiovascular functions. Capitalizing on this knowledge, the University of Michigan endeavor took “a giant step forward,” says Gisele Oda, a researcher at the Institute of Biosciences at the University of Sao Paulo in Brazil and an expert in chronobiology—the science of biological rhythms. She commends the researchers for developing a complex algorithm that “could extract useful information beyond the established knowledge that heart rate increases and becomes more irregular in COVID patients.”
Wearable devices open the possibility of obtaining large-scale, long, continuous, and real-time heart-rate data on people performing everyday activities or while sleeping. “Importantly, the conceptual basis of this algorithm put circadian rhythms at the center stage,” Oda says, referring to the physical, mental, and behavioral changes that follow a 24-hour cycle. “What we knew before was often based on short-time heart rate measured at any time of day,” she adds, while noting that heart rate varies between day and night and also changes with activity.
However, without comparison to a control group of people having the common flu, it is difficult to determine if the heart-rate signals are unique to COVID-19 or also occur with other illnesses, says John Torous, an assistant professor of psychiatry at Harvard Medical School who has researched wearable devices. In addition, he points to recent data showing that many wearables, which work by beaming light through the skin, may be less accurate in people with darker skin due to variations in light absorption.
While the results sound interesting, they lack the level of conclusive evidence that would be needed to transform how physicians care for patients. “But it is a good step in learning more about what these wearables can tell us,” says Torous, who is also director of digital psychiatry at Beth Israel Deaconess Medical Center, a Harvard affiliate, in Boston. A follow-up step would entail replicating the results in a different pool of people to “help us realize the full value of this work.”
It is important to note that this research was conducted in university settings during the early phases of the pandemic, with remote learning in full swing amid strict isolation and quarantine mandates in effect. The findings demonstrate that physiological monitoring can be performed using consumer-grade wearable sensors, allowing research to continue without in-person contact, says Sung Won Choi, a professor of pediatrics at the University of Michigan who is principal investigator of the student study.
“The worldwide COVID-19 pandemic interrupted a lot of activities that relied on face-to-face interactions, including clinical research,” Choi says. “Mobile technology proved to be tremendously beneficial during that time, because it allowed us to collect detailed physiological data from research participants remotely over an entire semester.” In fact, the researchers did not have any in-person contact with the students involved in the study. “Everything was done virtually," Choi explains. "Importantly, their willingness to participate in research and share data during this historical time, combined with the capacity of secure cloud storage and novel mathematical analytics, enabled our research teams to identify unique patterns in heart-rate data associated with COVID-19.”
Trading syphilis for malaria: How doctors treated one deadly disease by infecting patients with another
In the 1920s, doctors induced a high fever in patients - so called "fever therapy" - as a way to help them recover from syphilis, though it involved ethical problems.
If you had lived one hundred years ago, syphilis – a bacterial infection spread by sexual contact – would likely have been one of your worst nightmares. Even though syphilis still exists, it can now be detected early and cured quickly with a course of antibiotics. Back then, however, before antibiotics and without an easy way to detect the disease, syphilis was very often a death sentence.
To understand how feared syphilis once was, it’s important to understand exactly what it does if it’s allowed to progress: the infections start off as small, painless sores or even a single sore near the vagina, penis, anus, or mouth. The sores disappear around three to six weeks after the initial infection – but untreated, syphilis moves into a secondary stage, often presenting as a mild rash in various areas of the body (such as the palms of a person’s hands) or through other minor symptoms. The disease progresses from there, often quietly and without noticeable symptoms, sometimes for decades before it reaches its final stages, where it can cause blindness, organ damage, and even dementia. Research indicates, in fact, that as much as 10 percent of psychiatric admissions in the early 20th century were due to dementia caused by syphilis, also known as neurosyphilis.
Like any bacterial disease, syphilis can affect kids, too. Though it’s spread primarily through sexual contact, it can also be transmitted from mother to child during birth, causing lifelong disability.
The poet-physician Aldabert Bettman, who wrote fictionalized poems based on his experiences as a doctor in the 1930s, described the effect syphilis could have on an infant in his poem Daniel Healy:
I always got away clean
when I went out
With the boys.
The night before
I was married
I went out,—But was not so fortunate;
And I infected
My bride.
When little Daniel
Was born
His eyes discharged;
And I dared not tell
That because
I had seen too much
Little Daniel sees not at all
Given the horrors of untreated syphilis, it’s maybe not surprising that people would go to extremes to try and treat it. One of the earliest remedies for syphilis, dating back to 15th century Naples, was using mercury – either rubbing it on the skin where blisters appeared, or breathing it in as a vapor. (Not surprisingly, many people who underwent this type of “treatment” died of mercury poisoning.)
Other primitive treatments included using tinctures made of a flowering plant called guaiacum, as well as inducing “sweat baths” to eliminate the syphilitic toxins. In 1910, an arsenic-based drug called Salvarsan hit the market and was hailed as a “magic bullet” for its ability to target and destroy the syphilis-causing bacteria without harming the patient. However, while Salvarsan was effective in treating early-stage syphilis, it was largely ineffective by the time the infection progressed beyond the second stage. Tens of thousands of people each year continued to die of syphilis or were otherwise shipped off to psychiatric wards due to neurosyphilis.
It was in one of these psychiatric units in the early 20th century that Dr. Julius Wagner-Juaregg got the idea for a potential cure.
Wagner-Juaregg was an Austrian-born physician trained in “experimental pathology” at the University of Vienna. Wagner-Juaregg started his medical career conducting lab experiments on animals and then moved on to work at different psychiatric clinics in Vienna, despite having no training in psychiatry or neurology.
Wagner-Juaregg’s work was controversial to say the least. At the time, medicine – particularly psychiatric medicine – did not have anywhere near the same rigorous ethical standards that doctors, researchers, and other scientists are bound to today. Wagner-Juaregg would devise wild theories about the cause of their psychiatric ailments and then perform experimental procedures in an attempt to cure them. (As just one example, Wagner-Juaregg would sterilize his adolescent male patients, thinking “excessive masturbation” was the cause of their schizophrenia.)
But sometimes these wild theories paid off. In 1883, during his residency, Wagner-Juaregg noted that a female patient with mental illness who had contracted a skin infection and suffered a high fever experienced a sudden (and seemingly miraculous) remission from her psychosis symptoms after the fever had cleared. Wagner-Juaregg theorized that inducing a high fever in his patients with neurosyphilis could help them recover as well.
Eventually, Wagner-Juaregg was able to put his theory to the test. Around 1890, Wagner-Juaregg got his hands on something called tuberculin, a therapeutic treatment created by the German microbiologist Robert Koch in order to cure tuberculosis. Tuberculin would later turn out to be completely ineffective for treating tuberculosis, often creating severe immune responses in patients – but for a short time, Wagner-Juaregg had some success in using tuberculin to help his dementia patients. Giving his patients tuberculin resulted in a high fever – and after completing the treatment, Wagner-Jauregg reported that his patient’s dementia was completely halted. The success was short-lived, however: Wagner-Juaregg eventually had to discontinue tuberculin as a treatment, as it began to be considered too toxic.
By 1917, Wagner-Juaregg’s theory about syphilis and fevers was becoming more credible – and one day a new opportunity presented itself when a wounded soldier, stricken with malaria and a related fever, was accidentally admitted to his psychiatric unit.
When his findings were published in 1918, Wagner-Juaregg’s so-called “fever therapy” swept the globe.
What Wagner-Juaregg did next was ethically deplorable by any standard: Before he allowed the soldier any quinine (the standard treatment for malaria at the time), Wagner-Juaregg took a small sample of the soldier’s blood and inoculated three syphilis patients with the sample, rubbing the blood on their open syphilitic blisters.
It’s unclear how well the malaria treatment worked for those three specific patients – but Wagner-Juaregg’s records show that in the span of one year, he inoculated a total of nine patients with malaria, for the sole purpose of inducing fevers, and six of them made a full recovery. Wagner-Juaregg’s treatment was so successful, in fact, that one of his inoculated patients, an actor who was unable to work due to his dementia, was eventually able to find work again and return to the stage. Two additional patients – a military officer and a clerk – recovered from their once-terminal illnesses and returned to their former careers as well.
When his findings were published in 1918, Wagner-Juaregg’s so-called “fever therapy” swept the globe. The treatment was hailed as a breakthrough – but it still had risks. Malaria itself had a mortality rate of about 15 percent at the time. Many people considered that to be a gamble worth taking, compared to dying a painful, protracted death from syphilis.
Malaria could also be effectively treated much of the time with quinine, whereas other fever-causing illnesses were not so easily treated. Triggering a fever by way of malaria specifically, therefore, became the standard of care.
Tens of thousands of people with syphilitic dementia would go on to be treated with fever therapy until the early 1940s, when a combination of Salvarsan and penicillin caused syphilis infections to decline. Eventually, neurosyphilis became rare, and then nearly unheard of.
Despite his contributions to medicine, it’s important to note that Wagner-Juaregg was most definitely not a person to idolize. In fact, he was an outspoken anti-Semite and proponent of eugenics, arguing that Jews were more prone to mental illness and that people who were mentally ill should be forcibly sterilized. (Wagner-Juaregg later became a Nazi sympathizer during Hitler’s rise to power even though, bizarrely, his first wife was Jewish.) Another problematic issue was that his fever therapy involved experimental treatments on many who, due to their cognitive issues, could not give informed consent.
Lack of consent was also a fundamental problem with the syphilis study at Tuskegee, appalling research that began just 14 years after Wagner-Juaregg published his “fever therapy” findings.
Still, despite his outrageous views, Wagner-Juaregg was awarded the Nobel Prize in Medicine or Physiology in 1927 – and despite some egregious human rights abuses, the miraculous “fever therapy” was partly responsible for taming one of the deadliest plagues in human history.

