Coronavirus Risk Calculators: What You Need to Know
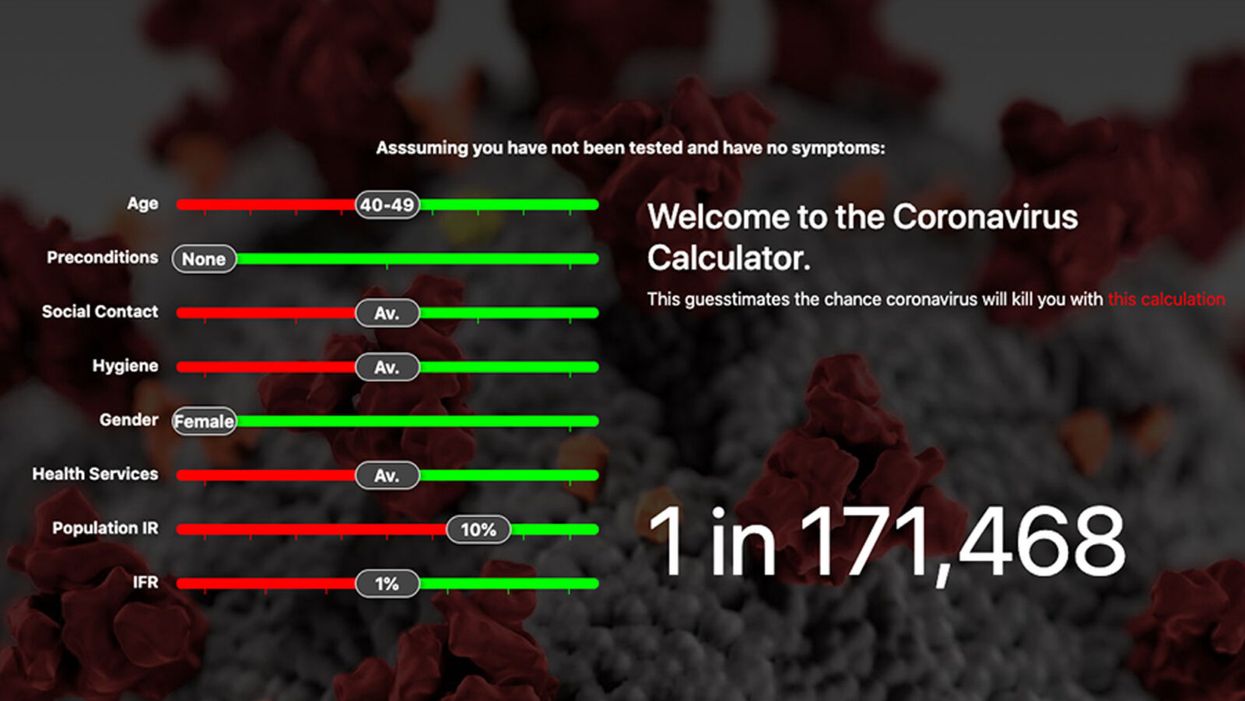
A screenshot of one coronavirus risk calculator.
People in my family seem to develop every ailment in the world, including feline distemper and Dutch elm disease, so I naturally put fingers to keyboard when I discovered that COVID-19 risk calculators now exist.
"It's best to look at your risk band. This will give you a more useful insight into your personal risk."
But the results – based on my answers to questions -- are bewildering.
A British risk calculator developed by the Nexoid software company declared I have a 5 percent, or 1 in 20, chance of developing COVID-19 and less than 1 percent risk of dying if I get it. Um, great, I think? Meanwhile, 19 and Me, a risk calculator created by data scientists, says my risk of infection is 0.01 percent per week, or 1 in 10,000, and it gave me a risk score of 44 out of 100.
Confused? Join the club. But it's actually possible to interpret numbers like these and put them to use. Here are five tips about using coronavirus risk calculators:
1. Make Sure the Calculator Is Designed For You
Not every COVID-19 risk calculator is designed to be used by the general public. Cleveland Clinic's risk calculator, for example, is only a tool for medical professionals, not sick people or the "worried well," said Dr. Lara Jehi, Cleveland Clinic's chief research information officer.
Unfortunately, the risk calculator's web page fails to explicitly identify its target audience. But there are hints that it's not for lay people such as its references to "platelets" and "chlorides."
The 19 and Me or the Nexoid risk calculators, in contrast, are both designed for use by everyone, as is a risk calculator developed by Emory University.
2. Take a Look at the Calculator's Privacy Policy
COVID-19 risk calculators ask for a lot of personal information. The Nexoid calculator, for example, wanted to know my age, weight, drug and alcohol history, pre-existing conditions, blood type and more. It even asked me about the prescription drugs I take.
It's wise to check the privacy policy and be cautious about providing an email address or other personal information. Nexoid's policy says it provides the information it gathers to researchers but it doesn't release IP addresses, which can reveal your location in certain circumstances.
John-Arne Skolbekken, a professor and risk specialist at Norwegian University of Science and Technology, entered his own data in the Nexoid calculator after being contacted by LeapsMag for comment. He noted that the calculator, among other things, asks for information about use of recreational drugs that could be illegal in some places. "I have given away some of my personal data to a company that I can hope will not misuse them," he said. "Let's hope they are trustworthy."
The 19 and Me calculator, by contrast, doesn't gather any data from users, said Cindy Hu, data scientist at Mathematica, which created it. "As soon as the window is closed, that data is gone and not captured."
The Emory University risk calculator, meanwhile, has a long privacy policy that states "the information we collect during your assessment will not be correlated with contact information if you provide it." However, it says personal information can be shared with third parties.
3. Keep an Eye on Time Horizons
Let's say a risk calculator says you have a 1 percent risk of infection. That's fairly low if we're talking about this year as a whole, but it's quite worrisome if the risk percentage refers to today and jumps by 1 percent each day going forward. That's why it's helpful to know exactly what the numbers mean in terms of time.
Unfortunately, this information isn't always readily available. You may have to dig around for it or contact a risk calculator's developers for more information. The 19 and Me calculator's risk percentages refer to this current week based on your behavior this week, Hu said. The Nexoid calculator, by contrast, has an "infinite timeline" that assumes no vaccine is developed, said Jonathon Grantham, the company's managing director. But your results will vary over time since the calculator's developers adjust it to reflect new data.
When you use a risk calculator, focus on this question: "How does your risk compare to the risk of an 'average' person?"
4. Focus on the Big Picture
The Nexoid calculator gave me numbers of 5 percent (getting COVID-19) and 99.309 percent (surviving it). It even provided betting odds for gambling types: The odds are in favor of me not getting infected (19-to-1) and not dying if I get infected (144-to-1).
However, Grantham told me that these numbers "are not the whole story." Instead, he said, "it's best to look at your risk band. This will give you a more useful insight into your personal risk." Risk bands refer to a segmentation of people into five categories, from lowest to highest risk, according to how a person's result sits relative to the whole dataset.
The Nexoid calculator says I'm in the "lowest risk band" for getting COVID-19, and a "high risk band" for dying of it if I get it. That suggests I'd better stay in the lowest-risk category because my pre-existing risk factors could spell trouble for my survival if I get infected.
Michael J. Pencina, a professor and biostatistician at Duke University School of Medicine, agreed that focusing on your general risk level is better than focusing on numbers. When you use a risk calculator, he said, focus on this question: "How does your risk compare to the risk of an 'average' person?"
The 19 and Me calculator, meanwhile, put my risk at 44 out of 100. Hu said that a score of 50 represents the typical person's risk of developing serious consequences from another disease – the flu.
5. Remember to Take Action
Hu, who helped develop the 19 and Me risk calculator, said it's best to use it to "understand the relative impact of different behaviors." As she noted, the calculator is designed to allow users to plug in different answers about their behavior and immediately see how their risk levels change.
This information can help us figure out if we should change the way we approach the world by, say, washing our hands more or avoiding more personal encounters.
"Estimation of risk is only one part of prevention," Pencina said. "The other is risk factors and our ability to reduce them." In other words, odds, percentages and risk bands can be revealing, but it's what we do to change them that matters.
Stacey Khoury felt more fatigued and out of breath than she was used to from just walking up the steps to her job in retail jewelry sales in Nashville, Tennessee. By the time she got home, she was more exhausted than usual, too.
"I just thought I was working too hard and needed more exercise," recalls the native Nashvillian about those days in December 2010. "All of the usual excuses you make when you're not feeling 100%."
As a professional gemologist, being hospitalized during peak holiday sales season wasn't particularly convenient. There was no way around it though when her primary care physician advised Khoury to see a blood disorder oncologist because of her disturbing blood count numbers. As part of a routine medical exam, a complete blood count screens for a variety of diseases and conditions that affect blood cells, such as anemia, infection, inflammation, bleeding disorders and cancer.
"If approved, it will allow more patients to potentially receive a transplant than would have gotten one before."
While she was in the hospital, a bone marrow biopsy revealed that Khoury had acute myeloid leukemia, or AML, a high-risk blood cancer. After Khoury completed an intense first round of chemotherapy, her oncologist recommended a bone marrow transplant. The potentially curative treatment for blood-cancer patients requires them to first receive a high dose of chemotherapy. Next, an infusion of stem cells from a healthy donor's bone marrow helps form new blood cells to fight off the cancer long-term.
Each year, approximately 8,000 patients in the U.S. with AML and other blood cancers receive a bone marrow transplant from a donor, according to the Center for International Blood and Marrow Transplant Research. But Khoury wasn't so lucky. She ended up being among the estimated 40% of patients eligible for bone marrow transplants who don't receive one, usually because there's no matched donor available.
Khoury's oncologist told her about another option. She could enter a clinical trial for an investigational cell therapy called omidubicel, which is being developed by Israeli biotech company Gamida Cell. The company's cell therapy, which is still experimental, could up a new avenue of treatment for cancer patients who can't get a bone marrow transplant.
Omidubicel consists of stem cells from cord blood that have been expanded using Gamida's technology to ensure there are enough cells for a therapeutic dose. The company's technology allows the immature cord blood cells to multiply quickly in the lab. Like a bone marrow transplant, the goal of the therapy is to make sure the donor cells make their way to the bone marrow and begin producing healthy new cells — a process called engraftment.
"If approved, it will allow more patients to potentially receive a transplant than would have gotten one before, so there's something very novel and exciting about that," says Ronit Simantov, Gamida Cell's chief medical officer.
Khoury and her husband Rick packed up their car and headed to the closest trial site, the Duke University School of Medicine, roughly 500 miles away. There they met with Mitchell Horowitz, a stem cell transplant specialist at Duke and principal investigator for Gamida's omidubicel study in the U.S.
He told Khoury she was a perfect candidate for the trial, and she enrolled immediately. "When you have one of two decisions, and it's either do this or you're probably not going to be around, it was a pretty easy decision to make, and I am truly thankful for that," she says.
Khoury's treatment started at the end of March 2011, and she was home by July 4 that year. She say the therapy "worked the way the doctors wanted it to work." Khoury's blood counts were rising quicker than the people who had bone marrow matches, and she was discharged from Duke earlier than other patients were.
By expanding the number of cord blood cells — which are typically too few to treat an adult — omidubicel allows doctors to use cord blood for patients who require a transplant but don't have a donor match for bone marrow.
Patients receiving omidubicel first get a blood test to determine their human leukocyte antigen, or HLA, type. This protein is found on most cells in the body and is an important regulator of the immune system. HLA typing is used to match patients to bone marrow and cord blood donors, but cord blood doesn't require as close of a match.
Like bone marrow transplants, one potential complication of omidubicel is graft-versus-host disease, when the donated bone marrow or stem cells register the recipient's body as foreign and attack the body. Depending on the severity of the response, according to the Mayo Clinic, treatment includes medication to suppress the immune system, such as steroids. In clinical trials, the occurrence of graft-versus-host disease with omidubicel was comparable with traditional bone marrow transplants.
"Transplant doctors are working on improving that," Simantov says. "A number of new therapies that specifically address graft-versus-host disease will be making some headway in the coming months and years."
Gamida released the results of the Phase 3 study in February and continues to follow Khoury and the other study patients for their long-term outcomes. The large randomized trial evaluated the safety and efficacy of omidubicel compared to standard umbilical cord blood transplants in patients with blood cancer who didn't have a suitable bone marrow donor. Around 120 patients aged 12 to 65 across the U.S., Europe and Asia were included in the trial. The study found that omidubicel resulted in faster recovery, fewer bacterial and viral infections and fewer days in the hospital.
The company plans to seek FDA approval this year. Simantov anticipates the therapy will receive FDA approval by 2022.
"Opening up cord blood transplants is very important, especially for people of diverse ethnic backgrounds," says oncologist Gary Schiller, principal investigator at the David Geffen School of Medicine at UCLA for Gamida Cell's mid- and late-stage trials. "This expansion technology makes a big difference because it makes cord blood an available option for those who do not have another donor source."
As for Khoury, who proudly celebrated the anniversary of her first transplant in April—she remains cancer free and continues to work full-time as a gemologist. When she has a little free time, she enjoys gardening, sewing, or maybe traveling to national parks like Yellowstone or the Grand Canyon with her husband Rick.
Paralyzed By Polio, This British Tea Broker Changed the Course Of Medical History Forever
Robin Cavendish in his special wheelchair with his son Jonathan in the 1960s.
In December 1958, on a vacation with his wife in Kenya, a 28-year-old British tea broker named Robin Cavendish became suddenly ill. Neither he nor his wife Diana knew it at the time, but Robin's illness would change the course of medical history forever.
Robin was rushed to a nearby hospital in Kenya where the medical staff delivered the crushing news: Robin had contracted polio, and the paralysis creeping up his body was almost certainly permanent. The doctors placed Robin on a ventilator through a tracheotomy in his neck, as the paralysis from his polio infection had rendered him unable to breathe on his own – and going off the average life expectancy at the time, they gave him only three months to live. Robin and Diana (who was pregnant at the time with their first child, Jonathan) flew back to England so he could be admitted to a hospital. They mentally prepared to wait out Robin's final days.
But Robin did something unexpected when he returned to the UK – just one of many things that would astonish doctors over the next several years: He survived. Diana gave birth to Jonathan in February 1959 and continued to visit Robin regularly in the hospital with the baby. Despite doctors warning that he would soon succumb to his illness, Robin kept living.
After a year in the hospital, Diana suggested something radical: She wanted Robin to leave the hospital and live at home in South Oxfordshire for as long as he possibly could, with her as his nurse. At the time, this suggestion was unheard of. People like Robin who depended on machinery to keep them breathing had only ever lived inside hospital walls, as the prevailing belief was that the machinery needed to keep them alive was too complicated for laypeople to operate. But Diana and Robin were up for the challenges – and the risks. Because his ventilator ran on electricity, if the house were to unexpectedly lose power, Diana would either need to restore power quickly or hand-pump air into his lungs to keep him alive.
Robin's wheelchair was not only the first of its kind; it became the model for the respiratory wheelchairs that people still use today.
In an interview as an adult, Jonathan Cavendish reflected on his parents' decision to live outside the hospital on a ventilator: "My father's mantra was quality of life," he explained. "He could have stayed in the hospital, but he didn't think that was as good of a life as he could manage. He would rather be two minutes away from death and living a full life."
After a few years of living at home, however, Robin became tired of being confined to his bed. He longed to sit outside, to visit friends, to travel – but had no way of doing so without his ventilator. So together with his friend Teddy Hall, a professor and engineer at Oxford University, the two collaborated in 1962 to create an entirely new invention: a battery-operated wheelchair prototype with a ventilator built in. With this, Robin could now venture outside the house – and soon the Cavendish family became famous for taking vacations. It was something that, by all accounts, had never been done before by someone who was ventilator-dependent. Robin and Hall also designed a van so that the wheelchair could be plugged in and powered during travel. Jonathan Cavendish later recalled a particular family vacation that nearly ended in disaster when the van broke down outside of Barcelona, Spain:
"My poor old uncle [plugged] my father's chair into the wrong socket," Cavendish later recalled, causing the electricity to short. "There was fire and smoke, and both the van and the chair ground to a halt." Johnathan, who was eight or nine at the time, his mother, and his uncle took turns hand-pumping Robin's ventilator by the roadside for the next thirty-six hours, waiting for Professor Hall to arrive in town and repair the van. Rather than being panicked, the Cavendishes managed to turn the vigil into a party. Townspeople came to greet them, bringing food and music, and a local priest even stopped by to give his blessing.
Robin had become a pioneer, showing the world that a person with severe disabilities could still have mobility, access, and a fuller quality of life than anyone had imagined. His mission, along with Hall's, then became gifting this independence to others like himself. Robin and Hall raised money – first from the Ernest Kleinwort Charitable Trust, and then from the British Department of Health – to fund more ventilator chairs, which were then manufactured by Hall's company, Littlemore Scientific Engineering, and given to fellow patients who wanted to live full lives at home. Robin and Hall used themselves as guinea pigs, testing out different models of the chairs and collaborating with scientists to create other devices for those with disabilities. One invention, called the Possum, allowed paraplegics to control things like the telephone and television set with just a nod of the head. Robin's wheelchair was not only the first of its kind; it became the model for the respiratory wheelchairs that people still use today.
Robin went on to enjoy a long and happy life with his family at their house in South Oxfordshire, surrounded by friends who would later attest to his "down-to-earth" personality, his sense of humor, and his "irresistible" charm. When he died peacefully at his home in 1994 at age 64, he was considered the world's oldest-living person who used a ventilator outside the hospital – breaking yet another barrier for what medical science thought was possible.