Can an “old school” vaccine address global inequities in Covid-19 vaccination?

Scientists at Baylor College of Medicine developed a vaccine called Corbevax that, unlike mRNA vaccines, can be mass produced using technology already in place in low- and middle-income countries. It's now being administered in India to children aged 12-14.
When the COVID-19 pandemic began invading the world in late 2019, Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. The scientists, with their prior experience of developing inexpensive vaccines for the world’s poor, had anticipated that the global rollout of Covid-19 jabs would be marked with several inequities. They wanted to create a patent-free vaccine to bridge this gap, but the U.S. government did not seem impressed, forcing the researchers to turn to private philanthropies for funds.
Hotez and Bottazzi, both scientists at the Texas Children’s Hospital Center for Vaccine Development at Baylor College of Medicine, raised about $9 million in private funds. Meanwhile, the U.S. government’s contribution stood at $400,000.
“That was a very tough time early on in the pandemic, you know, trying to do the work and raise the money for it at the same time,” says Hotez, who was nominated in February for a Nobel Peace Prize with Bottazzi for their COVID-19 vaccine. He adds that at the beginning of the pandemic, governments emphasized speed, innovation and rapidly immunizing populations in North America and Europe with little consideration for poorer countries. “We knew this [vaccine] was going to be the answer to global vaccine inequality, but I just wish the policymakers had felt the same,” says Hotez.
Over the past two years, the world has witnessed 488 million COVID-19 infections and over 61 million deaths. Over 11 billion vaccine doses have been administered worldwide; however, the global rollout of COVID-19 vaccines is marked with alarming socio-economic inequities. For instance, 72 percent of the population in high-income countries has received at least one dose of the vaccine, whereas the number stands at 15 percent in low-income countries.
This inequity is worsening vulnerabilities across the world, says Lawrence Young, a virologist and co-lead of the Warwick Health Global Research Priority at the UK-based University of Warwick. “As long as the virus continues to spread and replicate, particularly in populations who are under-vaccinated, it will throw up new variants and these will remain a continual threat even to those countries with high rates of vaccination,” says Young, “Therefore, it is in all our interests to ensure that vaccines are distributed equitably across the world.”
“When your house is on fire, you don't call the patent attorney,” says Hotez. “We wanted to be the fire department.”
The vaccine developed by Hotez and Bottazzi recently received emergency use authorisation in India, which plans to manufacture 100 million doses every month. Dubbed ‘Corbevax’ by its Indian maker, Biological E Limited, the vaccine is now being administered in India to children aged 12-14. The patent-free arrangement means that other low- and middle-income countries could also produce and distribute the vaccine locally.
“When your house is on fire, you don't call the patent attorney, you call the fire department,” says Hotez, commenting on the intellectual property rights waiver. “We wanted to be the fire department.”
The Inequity
Vaccine equity simply means that all people, irrespective of their location, should have equal access to vaccines. However, data suggests that the global COVID-19 vaccine rollout has favoured those in richer countries. For instance, high-income countries like the UAE, Portugal, Chile, Singapore, Australia, Malta, Hong Kong and Canada have partially vaccinated over 85 percent of their populations. This percentage in poorer countries, meanwhile, is abysmally low – 2.1 percent in Yemen, 4.6 in South Sudan, 5 in Cameroon, 9.9 in Burkina Faso, 10 in Nigeria, 12 in Somalia, 12 in Congo, 13 in Afghanistan and 21 in Ethiopia.

In late 2019, scientists Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. In February, they were nominated for a Nobel Peace Prize.
Texas Children's Hospital
The COVID-19 vaccination coverage is particularly low in African countries, and according to Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of African Local Initiative for Vaccinology Expertise, vaccine access and inequity remains a challenge in Africa. Madhi adds that a lack of vaccine access has affected the pandemic’s trajectory on the continent, but a majority of its people have now developed immunity through natural infection. “This has come at a high cost of loss of lives,” he says.
COVID-19 vaccines mean a significant financial burden for poorer countries, which spend an average of $41 per capita annually on health, while the average cost of every COVID-19 vaccine dose ranges between $2 and $40 in addition to a distribution cost of $3.70 per person for two doses. In December last year, the World Health Organisation (WHO) set a goal of immunizing 70 percent of the population of all countries by mid-2022. This, however, means that low-income countries would have to increase their health expenditure by an average of 56.6 percent to cover the cost, as opposed to 0.8 per cent in high-income countries.
Reflecting on the factors that have driven global inequity in COVID-19 vaccine distribution, Andrea Taylor, assistant director of programs at the Duke Global Health Innovation Center, says that wealthy nations took the risk of investing heavily in the development and scaling up of COVID-19 vaccines – at a time when there was little evidence to show that vaccines would work. This reserved a place for these nations at the front of the queue when doses started rolling off production lines. Lower-income countries, meanwhile, could not afford such investments.
“Now, however, global supply is not the issue,” says Taylor. “We are making plenty of doses to meet global need. The main problem is infrastructure to get the vaccine where it is most needed in a predictable and timely way and to ensure that countries have all the support they need to store, transport, and use the vaccine once it is received.”

Taufique Joarder, vice-chairperson of Bangladesh's Public Health Foundation, sees the need for more trials and data before Corbevax is made available to the general population.
In addition to global inequities in vaccination coverage, there are inequities within nations. Taufique Joarder, vice-chairperson of Bangladesh’s Public Health Foundation, points to the situation in his country, where vaccination coverage in rural and economically disadvantaged communities has suffered owing to weak vaccine-promotion initiatives and the difficulty many people face in registering online for jabs.
Joarder also cites the example of the COVID-19 immunization drive for children aged 12 years and above. “[Children] are given the Pfizer vaccine, which requires an ultralow temperature for storage. This is almost impossible to administer in many parts of the country, especially the rural areas. So, a large proportion of the children are being left out of vaccination,” says Joarder, adding that Corbevax, which is cheaper and requires regular temperature refrigeration “can be an excellent alternative to Pfizer for vaccinating rural children.”
Corbevax vs. mRNA Vaccines
As opposed to most other COVID-19 vaccines, which use the new Messenger RNA (mRNA) vaccine technology, Corbevax is an “old school” vaccine, says Hotez. The vaccine is made through microbial fermentation in yeast, similar to the process used to produce the recombinant hepatitis B vaccine, which has been administered to children in several countries for decades. Hence, says Hotez, the technology to produce Corbevax at large scales is already in place in countries like Vietnam, Bangladesh, India, Indonesia, Brazil, Argentina, among many others.
“So if you want to rapidly develop and produce and empower low- and middle-income countries, this is the technology to do it,” he says.
“Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines," says Andrea Taylor.
The COVID-19 vaccines created by Pfizer-BioNTech and Moderna marked the first time that mRNA vaccine technology was approved for use. However, scientists like Young feel that there is “a need to be pragmatic and not seduced by new technologies when older, tried and tested approaches can also be effective.” Taylor, meanwhile, says that although mRNA vaccines have dominated the COVID-19 vaccine market in the U.S., “there is no clear grounding for this preference in the data we have so far.” She adds that there is also growing evidence that the immunity from these shots may not hold up as well over time as that of vaccines using different platforms.
“The mRNA vaccines are well suited to wealthy countries with sufficient ultra-cold storage and transportation infrastructure, but these vaccines are divas and do not travel well in the rest of the world,” says Taylor. “Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines, such as the protein subunit platform used by Novavax and Corbevax. These require only standard refrigeration, can be manufactured using existing facilities all over the world, and are easy to transport.”
Joarder adds that Corbevax is cheaper due to the developers’ waived intellectual rights. It could also be used as a booster vaccine in Bangladesh, where only five per cent of the population has currently received booster doses. “If this vaccine is proved effective for heterologous boosting, [meaning] it works well and is well tolerated as a booster with other vaccines that are available in Bangladesh, this can be useful,” says Joarder.
According to Hotez, Corbevax can play several important roles - as a standalone adult or paediatric vaccine, and as a booster for other vaccines. Studies are underway to determine Corbevax’s effectiveness in these regards, he says.
Need for More Data
Biological E conducted two clinical trials involving 3000 subjects in India, and found Corbevax to be “safe and immunogenic,” with 90 percent effectiveness in preventing symptomatic infections from the original strain of COVID-19 and over 80 percent effectiveness against the Delta variant. The vaccine is currently in use in India, and according to Hotez, it’s in the pipeline at different stages in Indonesia, Bangladesh and Botswana.
However, Corbevax is yet to receive emergency use approval from the WHO. Experts such as Joarder see the need for more trials and data before it is made available to the general population. He says that while the WHO’s emergency approval is essential for global scale-up of the vaccine, we need data to determine age-stratified efficacy of the vaccine and whether it can be used for heterologous boosting with other vaccines. “According to the most recent data, the 100 percent circulating variant in Bangladesh is Omicron. We need to know how effective is Corbevax against the Omicron variant,” says Joarder.
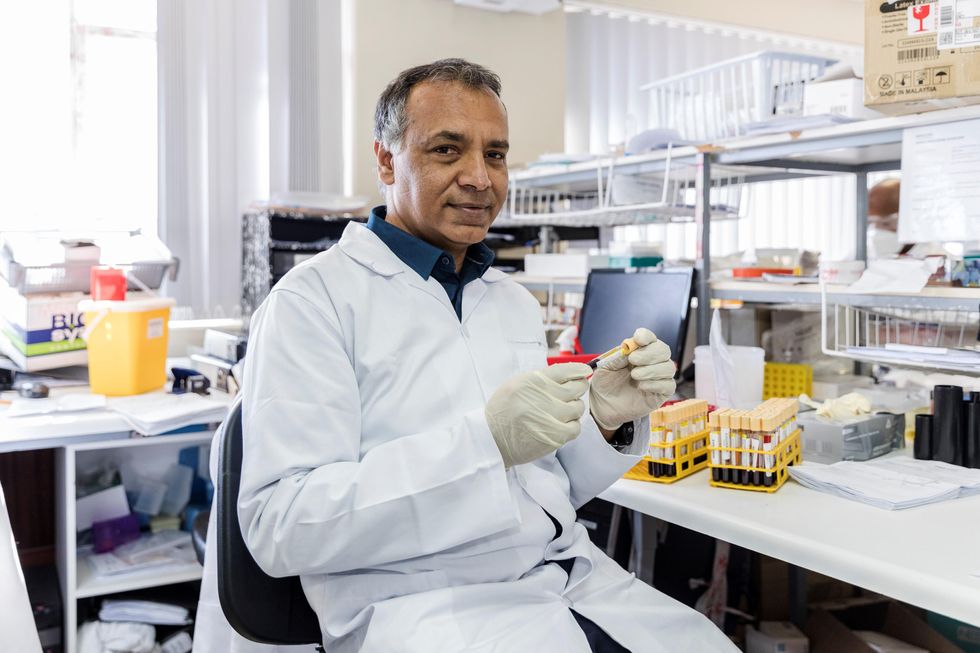
Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of the African Local Initiative for Vaccinology Expertise, says that a majority of people in Africa have now developed immunity through natural infection. “This has come at a high cost of loss of lives."
Shivan Parusnath
Others, meanwhile, believe that availing vaccines to poorer countries is not enough to resolve the inequity. Young, the Warwick virologist, says that the global vaccination rollout has also suffered from a degree of vaccine hesitancy, echoing similar observations by President Biden and Pfizer’s CEO. The problem can be blamed on poor communication about the benefits of vaccination. “The Corbevax vaccine [helps with the issues of] patent protection, vaccine storage and distribution, but governments need to ensure that their people are clearly informed.” Notably, however, some research has found higher vaccine willingness in lower-income countries than in the U.S.
Young also emphasized the importance of establishing local vaccination stations to improve access. For some countries, meanwhile, it may be too late. Speaking about the African continent, Madhi says that Corbevax has arrived following the peak of the crisis and won’t reverse the suffering and death that has transpired because of vaccine hoarding by high-income countries.
“The same goes for all the sudden donations from countries such as France - pretty much of little to no value when the pandemic is at its tail end,” says Madhi. “This, unfortunately, is a repeat of the swine flu pandemic in 2009, when vaccines only became available to Africa after the pandemic had very much subsided.”
At the “Apple Store of Doctor’s Offices,” Preventive Care Is High Tech. Is it Worth $150 a Month?
A patient getting examined at health startup Forward.
What if going to the doctor's office could be … nice?
If you didn't have to wait for your appointment, but were ushered right in; if your medical data was all collated and easily searchable on an iPhone app; if a remote scribe took notes while you spoke with your doctor so you could make eye contact with them; if your doctor didn't seem horribly rushed.
Would you go to the doctor to get help staying healthy, rather than just to stop being sick?
Would that change the way you thought about your health? Would you go to the doctor to get help staying healthy, rather than just to stop being sick? And would that, in the long run, be much better for you?
Those are the animating questions for Forward, a healthcare startup devoted to preventive care. Led by founder Adrian Aoun, formerly of Google/Sidewalk labs, Forward opened its first office in San Francisco in 2016 and has since expanded to Los Angeles, Orange County, New York, and Washington, D.C., with a San Diego location opening soon.
It's been described as the "Apple Store of doctor's offices," which in some ways is a reaction to Forward's vibe: Patients have described the offices as having blonde wood, minimalist design, sparkling water on tap — and lots of high-tech gadgets, like the full-body scanner that replaces the standard scale and stethoscope.

The interior of a Forward office.
(Courtesy Forward)
The more crucial difference, though, is its model of care. Forward doesn't take insurance. Instead, patients, or "members," pay a flat $149 per month, along the lines of a subscription service like Netflix or a gym membership. That fee covers visits, messaging with medical staff through the Forward app, the use of a wearable (like a Fitbit or a sleep tracker) if the physician recommends it, plus any bloodwork or diagnostic tests run in the on-site labs. (The company declined to disclose how many people have signed up for memberships.)
Predictability is Forward's other significant, distinguishing feature: No surprise co-pays, or extra charges showing up on a billing statement months later. Everything is wrapped up in the $149 membership fee, unless the physician recommends visiting an outside specialist.
That caveat isn't a small one. It's important to note that Forward is in no way meant to replace standard health insurance. The service is strictly focused on preventive care, so it wouldn't be much use in case of an emergency; it's meant to help people, as far as is possible, avoid that emergency at all.
Ani Okkasian's family recently went through such an emergency. Her 62-year-old father, an active and seemingly healthy man living with diabetes, had been feeling unwell for a while, but struggled to receive constructive follow-up or tests from his doctor. It finally emerged that his liver was severely damaged, and he suffered a stroke — the risk of which can be elevated by liver disease. He seemed to deteriorate completely within mere weeks, Okkasian said, and in January he passed away.
"He was someone who'd go to the doctor regularly and listen to what they said and follow it," Okkasian said. "I shouldn't have had to bury my father at 62. I still believe to my core that his death could have been avoided if the primary care was adequate."
"I could tell that the people who designed [Forward] had lost someone to the legacy system; it was so streamlined and so much clearer."
Okkasian began researching, looking for a better alternative, and discovered Forward. Founder Aoun lost his grandfather to a heart attack; his brother's heart attack at age 31 was the impetus to start Forward.
"I could tell that that was the genesis," Okkasian said. "Having just lost someone, and having had to deal with different aspects of the healthcare industry — how complicated and convoluted that all is — I could tell that the people who designed [Forward] had lost someone to the legacy system; it was so streamlined and so much clearer."
So Who Is Forward For?
The Affordable Care Act mandates that evidence-based preventive care must be covered by insurers without any cost to the patient. Today, 30 million Americans are still living without health insurance; but for most of the population, cost shouldn't prevent access to standard, preventive care, says Benjamin Sommers, a physician and professor at the Harvard T.H. Chan School of Public Health who has studied the effect of the ACA on preventive care access.
For Okkasian and her family, it wasn't a lack of access to primary care that was at issue; it was the quality of that primary care. In 2019, that's probably true for a lot of people.
"How come all other industries have been disturbed except the medical industry?" Okkasian asked. "It's disturbing the most people. We're so advanced in so many ways, but when it comes to the healthcare system, we're not prioritizing the wellness of a person."
Is Forward the answer? Well, probably not for everyone. Its office are only in a handful of cities, and there are limits to how scalable it would be; it's unavoidable that the $149 per month charge restricts access for a lot of people. Those who have insurance through their employer might have a flexible spending account (FSA) that would cover some or all of the membership fee, and Forward has said that 15 percent of their early members came from underserved communities and were offered free plans; but for many others, that's just an unworkable extra cost.
Sommers also sounded a dubious note about a maximalist attitude toward data collection.
"Even though some patients may think that 'more is always better' — more testing, more screening, etc. — this isn't true," he said. "Some types of cancer screening, ovarian cancer screening for instance, are actually harmful or of no benefit, because studies have shown that they don't improve survival or health outcomes, but can lead to unnecessary testing, pain, false positives, anxiety, and other side effects.
"It's really great for people who are in good health, looking to make it better."
"I'm generally skeptical of efforts to charge people more to get 'extra testing' that isn't currently supported by the medical evidence," he added.
But relatively healthy people who want to take a more active approach to their health — or people who have frequent testing needs, like those using the HIV-prevention drug PrEP, and want to avoid co-pays — might benefit from the on-demand, low-friction experience that Forward offers.
"It's really great for people who are in good health, looking to make it better," Okkasian said. "Your experience is simplified to a point where you feel empowered, not scared."
Facial Recognition Can Reduce Racial Profiling and False Arrests
The use of face recognition technology is expanding exponentially right now.
[Editor's Note: This essay is in response to our current Big Question, which we posed to experts with different perspectives: "Do you think the use of facial recognition technology by the police or government should be banned? If so, why? If not, what limits, if any, should be placed on its use?"]
Opposing facial recognition technology has become an article of faith for civil libertarians. Many who supported the bans in cities like San Francisco and Oakland have declared the technology to be inherently racist and abusive.
The greatest danger would be to categorically oppose this technology and pretend that it will simply go away.
I have spent my career as a criminal defense attorney and a civil libertarian -- and I do not fear it. Indeed, I see it as positive so long as it is appropriately regulated and controlled.
We are living in the beginning of a biometric age, where technology uses our physical or biological characteristics for a variety of products and services. It holds great promises as well as great risks. The greatest danger, however, would be to categorically oppose this technology and pretend that it will simply go away.
This is an age driven as much by consumer as it is government demand. Living in denial may be emotionally appealing, but it will only hasten the creation of post-privacy world. If we do not address this emerging technology, movements in public will increasingly result in instant recognition and even tracking. It is the type of fish-bowl society that strips away any expectation of privacy in our interactions and associations.
The biometrics field is expanding exponentially, largely due to the popularity of consumer products using facial recognition technology (FRT) -- from the iPhone program to shopping ones that recognize customers.
But the privacy community is losing this battle because it is using the privacy rationales and doctrines forged in the earlier electronic surveillance periods. Just as generals are often accused of planning to fight the last war, civil libertarians can sometimes cling to past models despite their decreasing relevance in the current world.
I see FRT as having positive implications that are worth pursuing. When properly used, biometrics can actually enhance privacy interests and even reduce racial profiling by reducing false arrests and the warrantless "patdowns" allowed by the Supreme Court. Bans not only deny police a technology widely used by businesses, but return police to the highly flawed default of "eye balling" suspects -- a system with a considerably higher error rate than top FRT programs.
Officers are often wrong and stop a great number of suspects in the hopes of finding a wanted felon.
A study in Australia showed that passport officers who had taken photographs of subjects in ideal conditions nonetheless experienced high error rates when identifying them shortly afterward, including 14 percent false acceptance rates. Currently, officers stop suspects based on their memory from seeing a photograph days or weeks earlier. They are often wrong and stop a great number of suspects in the hopes of finding a wanted felon. The best FRT programs achieve an astonishing accuracy rate, though real-world implementation has challenges that must be addressed.
One legitimate concern raised in early studies showed higher error rates in recognitions for certain groups, particularly African American women. An MIT study finding that error rate prompted major improvements in the algorithms as well as training changes to greatly reduce the frequency of errors. The issue remains a concern, but there is nothing inherently racist in algorithms. These are a set of computer instructions that isolate and process with the parameters and conditions set by creators.
To be sure, there is room for improvement in some algorithms. Tests performed by the American Civil Liberties Union (ACLU) reportedly showed only an 80 percent accuracy rate in comparing mug shots to pictures of members of Congress when using Amazon's "Rekognition" system. It recently showed the same 80 percent rate in doing the same comparison to members of the California legislators.
However, different algorithms are available with differing levels of performance. Moreover, these products can be set with a lower discrimination level. The fact is that the top algorithms tested by the National Institute of Standards and Technology showed that their accuracy rate is greater than 99 percent.
The greatest threat of biometric technologies is to democratic values.
Assuming a top-performing algorithm is used, the result could be highly beneficial for civil liberties as opposed to the alternative of "eye balling" suspects. Consider the Boston Bombing where police declared a "containment zone" and forced families into the street with their hands in the air.
The suspect, Dzhokhar Tsarnaev, moved around Boston and was ultimately found outside the "containment zone" once authorities abandoned near martial law. He was caught on some surveillance systems but not identified. FRT can help law enforcement avoid time-consuming area searches and the questionable practice of forcing people out of their homes to physically examine them.
If we are to avoid a post-privacy world, we will have to redefine what we are trying to protect and reconceive how we hope to protect it. In my view, the greatest threat of biometric technologies is to democratic values. Authoritarian nations like China have made huge investments into FRT precisely because they know that the threat of recognition in public deters citizens from associating or interacting with protesters or dissidents. Recognition changes conduct. That chilling effect is what we have the worry about the most.
Conventional privacy doctrines do not offer much protection. The very concept of "public privacy" is treated as something of an oxymoron by courts. Public acts and associations are treated as lacking any reasonable expectation of privacy. In the same vein, the right to anonymity is not a strong avenue for protection. We are not living in an anonymous world anymore.
Consumers want products like FaceFind, which link their images with others across social media. They like "frictionless" transactions and authentications using faceprints. Despite the hyperbole in places like San Francisco, civil libertarians will not succeed in getting that cat to walk backwards.
The basis for biometric privacy protection should not be focused on anonymity, but rather obscurity. You will be increasingly subject to transparency-forcing technology, but we can legislatively mandate ways of obscuring that information. That is the objective of the Biometric Privacy Act that I have proposed in recent research. However, no such comprehensive legislation has passed through Congress.
The ability to spot fraudulent entries at airports or recognizing a felon in flight has obvious benefits for all citizens.
We also need to recognize that FRT has many beneficial uses. Biometric guns can reduce accidents and criminals' conduct. New authentications using FRT and other biometric programs could reduce identity theft.
And, yes, FRT could help protect against unnecessary police stops or false arrests. Finally, and not insignificantly, this technology could stop serious crimes, from terrorist attacks to the capturing of dangerous felons. The ability to spot fraudulent entries at airports or recognizing a felon in flight has obvious benefits for all citizens.
We can live and thrive in a biometric era. However, we will need to bring together civil libertarians with business and government experts if we are going to control this technology rather than have it control us.
[Editor's Note: Read the opposite perspective here.]